Quest for the right Drug
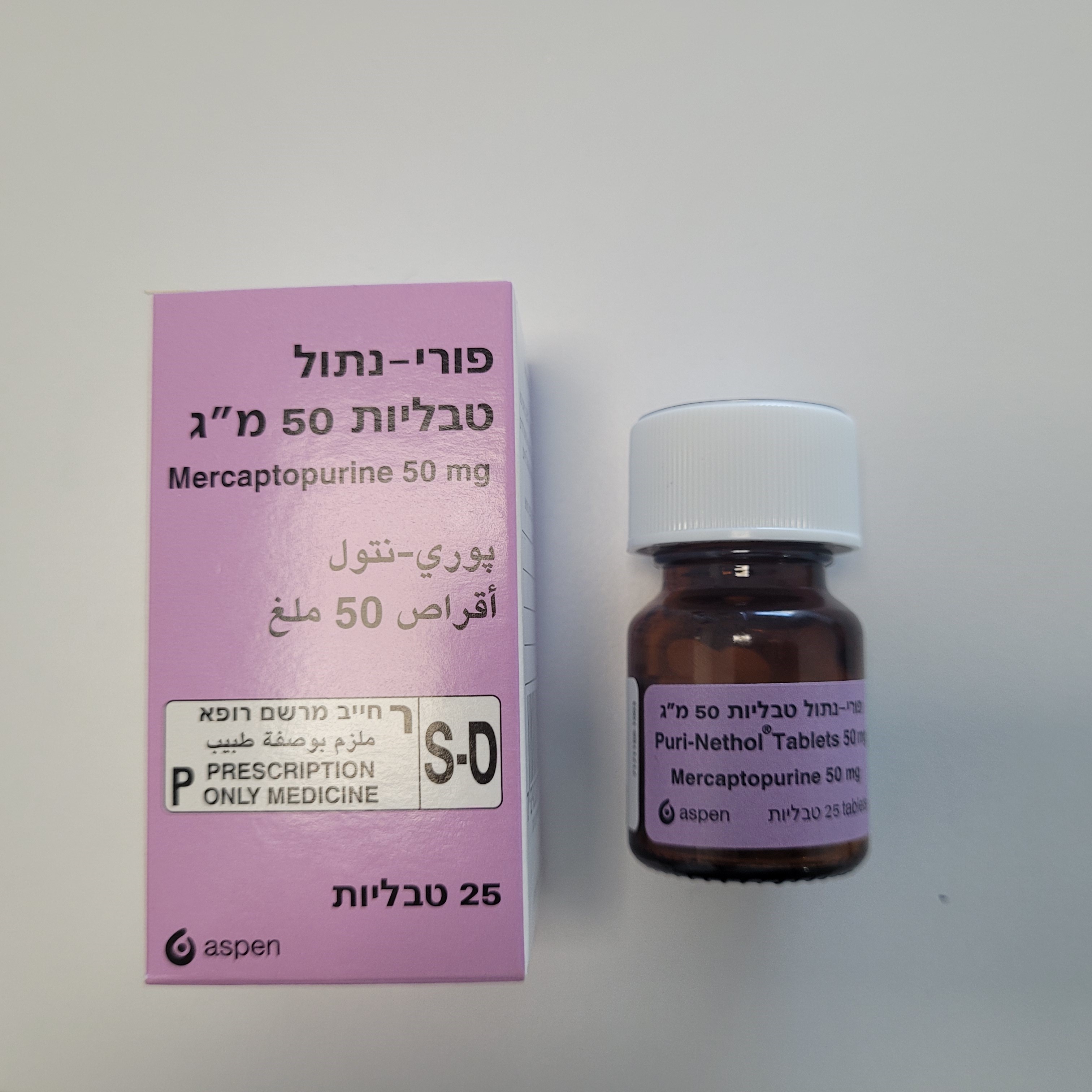
פורי-נתול טבליות 50 מ"ג PURI-NETHOL TABLETS 50 MG (MERCAPTOPURINE)
תרופה במרשם
תרופה בסל
נרקוטיקה
ציטוטוקסיקה
צורת מתן:
פומי : PER OS
צורת מינון:
טבליה : TABLETS
עלון לרופא
מינוניםPosology התוויות
Indications תופעות לוואי
Adverse reactions התוויות נגד
Contraindications אינטראקציות
Interactions מינון יתר
Overdose הריון/הנקה
Pregnancy & Lactation אוכלוסיות מיוחדות
Special populations תכונות פרמקולוגיות
Pharmacological properties מידע רוקחי
Pharmaceutical particulars אזהרת שימוש
Special Warning עלון לרופא
Physicians Leaflet
Special Warning : אזהרת שימוש
4.4 Special Warnings and Precautions for Use Mercaptopurine is an active cytotoxic agent and should be used only under the direction of physician experienced in the administration of such agents. Monitoring Since mercaptopurine is strongly myelosuppressive full blood counts must be taken daily during remission induction. Patients must be carefully monitored during therapy. Cytotoxicity and haematological monitoring Treatment with mercaptopurine causes bone marrow suppression leading to leucopenia and thrombocytopenia and, less frequently, to anaemia. Careful monitoring of haematological parameters should be conducted during therapy. The leucocyte and platelet counts continue to fall after treatment is stopped, so at the first sign of an abnormally large fall in the counts, treatment should be interrupted immediately. Bone marrow suppression is reversible if mercaptopurine is withdrawn early enough. There are individuals with an inherited deficiency of the TPMT enzyme activity who are very sensitive to the myelosuppressive effect of mercaptopurine and prone to developing rapid bone marrow depression following the initiation of treatment with mercaptopurine. This problem could be exacerbated by coadministration with active substances that inhibit TPMT, such as olsalazine, mesalazine or sulfasalazine. Some laboratories offer testing for TPMT deficiency, although these tests have not been shown to identify all patients at risk of severe toxicity. Therefore, close monitoring of blood counts is necessary. Substantial dose reductions are generally required for homozygous-TPMT deficiency patients to avoid the development of life-threatening bone marrow suppression. A possible association between decreased TPMT activity and secondary leukaemias and myelodysplasia has been reported in individuals receiving mercaptopurine in combination with other cytotoxics (see section 4.8). Increased haematological monitoring of the patient is advised when switching between different pharmaceutical formulations of mercaptopurine. Immunosuppression Immunisation using a live organism vaccine has the potential to cause infection in immunocompromised hosts. Therefore, immunisations with live organism vaccines are not recommended. In all cases, patients in remission should not receive live organism vaccines until the patient is deemed to be able to respond to the vaccine. The interval between discontinuation of chemotherapy and restoration of the patient's ability to respond to the vaccine depends on the intensity and type of immunosuppression-causing medications used, the underlying disease, and other factors. Co-administration of ribavirin and mercaptopurine is not advised. Ribavirin may reduce efficacy and increase toxicity of mercaptopurine (see section 4.5 Interaction with other medicinal products and other forms of interactions). During remission induction in acute myelogenous leukaemia, the patient may frequently have to survive a period of relative bone marrow aplasia and it is important that adequate supportive facilities are available. The dosage of mercaptopurine may need to be reduced when this agent is combined with other medicinal products whose primary or secondary toxicity is myelosuppression (see Section 4.5 Interaction with other medicinal products and other forms of interactions: Myelosuppressive agents). Hepatotoxicity Mercaptopurine is hepatotoxic and liver function tests should be monitored weekly during treatment. Gamma glutamyl transferase (GGT) levels in plasma may be particularly predictive of withdrawal due to hepatotoxicity. More frequent monitoring may be advisable in those with pre-existing liver disease or receiving other potentially hepatotoxic therapy. The patient should be instructed to discontinue mercaptopurine immediately if jaundice becomes apparent (see section 4.8). Renal toxicity During remission induction when rapid cell lysis is occurring, uric acid levels in blood and urine should be monitored as hyperuricaemia and/or hyperuricosuria may develop, with the risk of uric acid nephropathy. Hydration and urine alkalinisation may minimize potential renal complications. Renal and/or hepatic impairment Caution is advised during the administration of mercaptopurine in patients with renal impairment and/or hepatic impairment (see section 4.2 and section 5.2). Consideration should be given to reducing the dosage in these patients and haematological response should be carefully monitored. Pancreatitis in off-label treatment of patients with inflammatory bowel disease Pancreatitis has been reported to occur at a frequency of ≥ 1/100 to < 1/10 (“common”) in patients treated for the unlicensed indication inflammatory bowel disease. Mutagenicity and carcinogenicity Patients receiving immunosuppressive therapy, including Puri-Nethol, are at an increased risk of developing lymphoproliferative disorders and other malignancies, notably skin cancers (melanoma and non-melanoma), sarcomas (Kaposi's and non-Kaposi's) and uterine cervical cancer in situ. The increased risk appears to be related to the degree and duration of immunosuppression. It has been reported that discontinuation of immunosuppression may provide partial regression of the lymphoproliferative disorder. A treatment regimen containing multiple immunosuppressants (including thiopurines) should therefore be used with caution as this could lead to lymphoproliferative disorders, some with reported fatalities. A combination of multiple immunosuppressants, given concomitantly increases the risk of Epstein-Barr virus (EBV)-associated lymphoproliferative disorders. Increases in chromosomal aberrations were observed in the peripheral lymphocytes of leukaemic patients, in a renal cell carcinoma patient who received an unstated dose of mercaptopurine and in patients with chronic renal disease treated at doses of 0.4 - 1.0 mg/kg/day. In view of its action on cellular deoxyribonucleic acid (DNA) mercaptopurine is potentially carcinogenic and consideration should be given to the theoretical risk of carcinogenesis with this treatment. Two cases have been documented of the occurrence of acute non-lymphatic leukaemia in patients who received mercaptopurine, in combination with other medicinal products, for non-neoplastic disorders. A single case has been reported where a patient was treated for pyoderma gangrenosum with mercaptopurine and later developed acute non-lymphatic leukaemia, but it is not clear whether this was part of the natural history of the disease or if the mercaptopurine played a causative role. A patient with Hodgkin’s disease treated with mercaptopurine and multiple additional cytotoxic agents developed acute myelogenous leukaemia. Twelve and a half years after mercaptopurine treatment for myasthenia gravis, a female patient developed chronic myeloid leukaemia. Hepatosplenic T-cell lymphoma has been reported in patients with inflammatory bowel disease* treated with azathioprine (the prodrug to mercaptopurine) or mercaptopurine, either with or without concomitant treatment with anti- TNF alpha antibody. This rare type of T cell lymphoma has an aggressive disease course and is usually fatal (see also section 4.8). *inflammatory bowel disease (IBD) is an unlicensed indication. Macrophage activation syndrome Macrophage activation syndrome (MAS) is a known, life-threatening disorder that may develop in patients with autoimmune conditions, in particular with inflammatory bowel disease (IBD) (unlicensed indication), and there could potentially be an increased susceptibility for developing the condition with the use of mercaptopurine. If MAS occurs, or is suspected, evaluation and treatment should be started as early as possible, and treatment with mercaptopurine should be discontinued. Physicians should be attentive to symptoms of infection such as EBV and cytomegalovirus (CMV), as these are known triggers for MAS. Metabolism and nutrition disorders Administration of purine analogues, azathioprine and mercaptopurine, may interfere with the niacin pathway, potentially leading to nicotinic acid deficiency (pellagra). Few cases have been reported with the use of azathioprine and mercaptopurine, especially in patients with IBD (Crohn’s disease, colitis ulcerative). Diagnosis of pellagra should be considered in a patient presenting with localised pigmented rash (dermatitis); gastroenteritis (diarrhoea); or neurologic deficits, including cognitive decline (dementia). Appropriate medical care with niacin/nicotinamide supplementation must be initiated, and dose reduction or discontinuation of azathioprine must be considered. Infections Patients treated with mercaptopurine alone or in combination with other immunosuppressive agents, including corticosteroids, have shown increased susceptibility to viral, fungal and bacterial infections, including severe or atypical infection, and viral reactivation. The infectious disease and complications may be more severe in these patients than in non-treated patients. Prior exposure to or infection with varicella zoster virus should be taken into consideration prior to starting treatment. Local guidelines may be considered, including prophylactic therapy if necessary. Serologic testing prior to starting treatment should be considered with respect to hepatitis B. Local guidelines may be considered, including prophylactic therapy for cases which have been confirmed positive by serologic testing. Cases of neutropenic sepsis have been reported in patients receiving mercaptopurine for ALL. If the patient is infected during treatment appropriate measures should be taken, which may include appropriate antimicrobial therapy and supportive care. Paediatric population Cases of symptomatic hypoglycaemia have been reported in children with ALL receiving mercaptopurine (see Section 4.8 Undesirable Effects). The majority of reported cases were in children under the age of six or with a low body mass index. Interactions Xanthine oxidase inhibitors Patients treated with the xanthine oxidase inhibitors allopurinol, oxipurinol or thiopurinol, and mercaptopurine should only receive 25% of the usual dose of mercaptopurine since allopurinol decreases the rate of catabolism of mercaptopurine (see Section 4.2 Posology and method of administration and Section 4.5 Interaction with other medicinal products and other forms of interaction). Anticoagulants When oral anticoagulants are co-administered with mercaptopurine, a reinforced monitoring of INR (International Normalised Ratio) is recommended (see section 4.5) TPMT Deficiency There are individuals with an inherited deficiency of the enzyme thiopurine methyltransferase (TPMT) who may be unusually sensitive to the myelosuppressive effect of mercaptopurine and prone to developing rapid bone marrow depression following the initiation of treatment with mercaptopurine. This problem could be exacerbated by co- administration with medicinal products that inhibit TPMT, such as olsalazine, mesalazine or sulfazalazine. Also a possible association between decreased TPMT activity and secondary leukaemias and myelodysplasia has been reported in individuals receiving mercaptopurine in combination with other cytotoxics (see Section 4.8 Undesirable effects). Approximately 0.3 % (1:300) of patients have little or no detectable enzyme activity. Approximately 10 % of patients have low or intermediate TPMT activity and 90 % of individuals have normal TPMT activity. There may also be a group of approximately 2 % who have very high TPMT activity. Some laboratories offer testing for TPMT deficiency, although these tests have not been shown to identify all patients at risk of severe toxicity. Therefore close monitoring of blood counts is still necessary. Cross Resistance Cross resistance usually exists between mercaptopurine and 6-thioguanine. Hypersensitivity Patients suspected to have previously presented with a hypersensitivity reaction to mercaptopurine should not be recommended to use its pro-drug azathioprine, unless the patient has been confirmed as hypersensitive to mercaptopurine with allergological tests, and tested negative for azathioprine. As azathioprine is a pro-drug of mercaptopurine, patients with a previous history of hypersensitivity to azathioprine must be assessed for hypersensitivity to mercapopurine prior to initiating treatment. Lesch-Nyhan syndrome Limited evidence suggests that neither mercaptopurine nor its pro-drug azathioprine are effective in patients with the rare inherited condition complete hypoxanthine-guanine-phosphoribosyltransferase deficiency (Lesch-Nyhan syndrome). The use of mercaptopurine or azathioprine is not recommended in these patients. UV exposure Patients treated with mercaptopurine are more sensitive to the sun. Exposure to sunlight and UV light should be limited, and patients should be recommended to wear protective clothing and to use a sunscreen with a high protection factor. Excipients Patients with rare hereditary problems of galactose intolerance, total lactase deficiency or glucose-galactose malabsorption should not take this medicine. Safe handling of mercaptopurine tablets- See section 6.6.
Effects on Driving
4.7 Effects on ability to drive and use machines There are no data on the effect of mercaptopurine on driving performance or the ability to operate machinery. A detrimental effect on these activities cannot be predicted from the pharmacology of the medicinal product.

שימוש לפי פנקס קופ''ח כללית 1994
Acute lymphatic leukemia
תאריך הכללה מקורי בסל
01/01/1995
הגבלות
תרופה שאושרה לשימוש כללי בקופ'ח
מידע נוסף
עלון מידע לצרכן
13.06.16 - עלון לצרכן אנגלית 12.04.21 - עלון לצרכן אנגלית 14.08.22 - עלון לצרכן עברית 13.06.16 - עלון לצרכן ערבית 12.04.21 - עלון לצרכן ערבית 19.10.22 - עלון לצרכן אנגלית 19.10.22 - עלון לצרכן עברית 19.10.22 - עלון לצרכן ערבית 06.12.22 - עלון לצרכן 16.03.23 - עלון לצרכן אנגלית 07.06.23 - עלון לצרכן עברית 16.03.23 - עלון לצרכן ערבית 14.08.23 - עלון לצרכן אנגלית 14.08.23 - עלון לצרכן עברית 14.08.23 - עלון לצרכן ערבית 14.09.23 - עלון לצרכן עברית 02.12.23 - עלון לצרכן אנגלית 02.12.23 - עלון לצרכן עברית 02.12.23 - עלון לצרכן ערבית 26.07.15 - החמרה לעלון 02.12.20 - החמרה לעלון 06.12.22 - החמרה לעלון 07.06.23 - החמרה לעלון 14.09.23 - החמרה לעלוןלתרופה במאגר משרד הבריאות
פורי-נתול טבליות 50 מ"ג