Quest for the right Drug
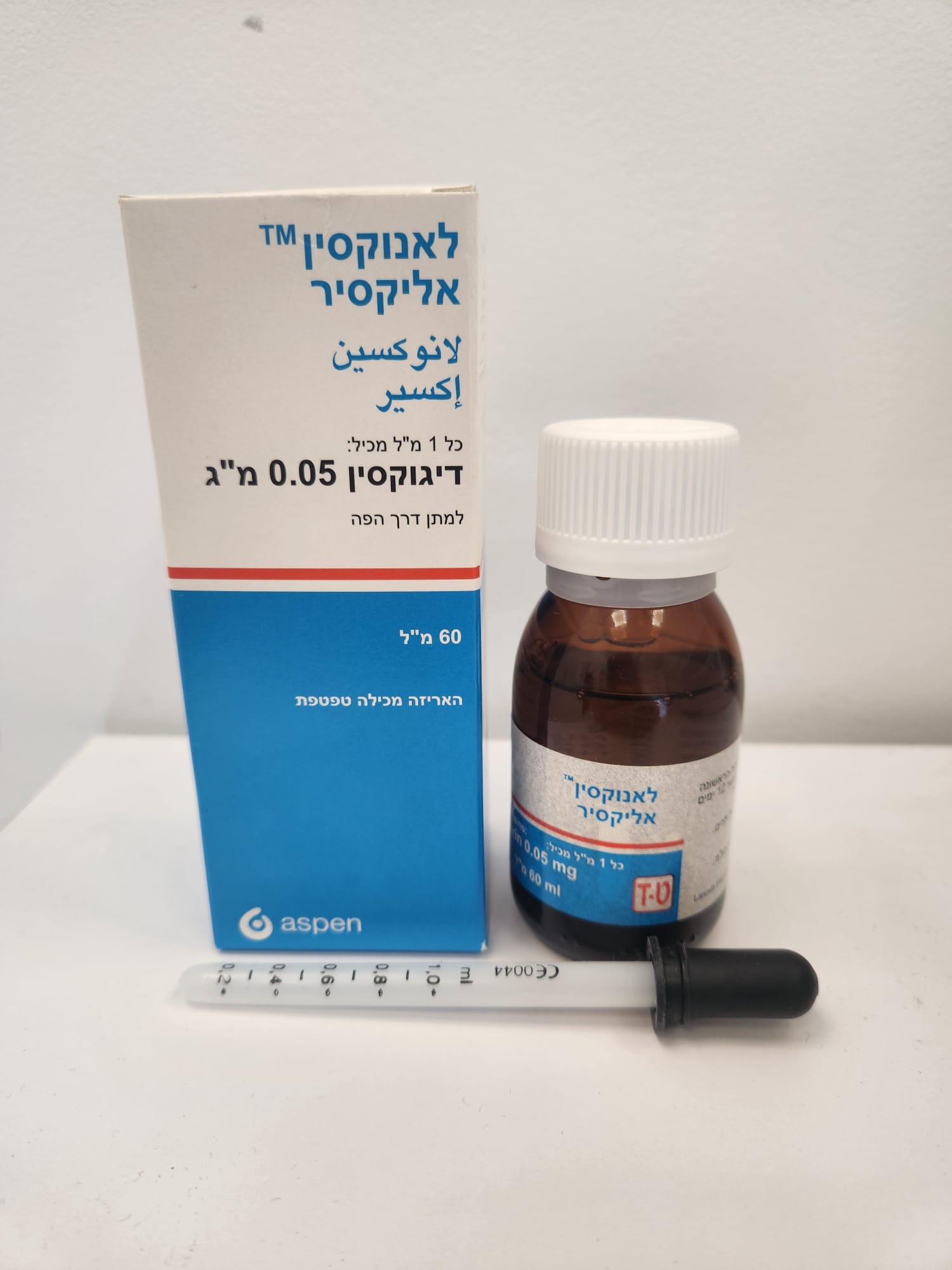
לאנוקסין אליקסיר LANOXIN ELIXIR (DIGOXIN)
תרופה במרשם
תרופה בסל
נרקוטיקה
ציטוטוקסיקה
צורת מתן:
פומי : PER OS
צורת מינון:
תמיסה אלכוהולית : ELIXIR
עלון לרופא
מינוניםPosology התוויות
Indications תופעות לוואי
Adverse reactions התוויות נגד
Contraindications אינטראקציות
Interactions מינון יתר
Overdose הריון/הנקה
Pregnancy & Lactation אוכלוסיות מיוחדות
Special populations תכונות פרמקולוגיות
Pharmacological properties מידע רוקחי
Pharmaceutical particulars אזהרת שימוש
Special Warning עלון לרופא
Physicians Leaflet
Overdose : מינון יתר
4.9. Overdose Symptoms and signs The symptoms and signs of toxicity are generally similar to those described in section 4.8, but may be more frequent and can be more severe. Signs and symptoms of digoxin toxicity become more frequent with levels above 2.0 nanograms/ml (2.56 nanomol/l) although there is considerable inter-individual variation. However, in deciding whether a patient's symptoms are due to digoxin, the clinical state, together with serum electrolyte levels and thyroid function are important factors (see Section 4.2). In patients undergoing haemodialysis, digoxin use is associated with increased mortality; patients with low pre-dialysis potassium concentrations are most at risk. Adults In adults without heart disease, clinical observation suggests that an overdose of digoxin of 10 to 15 mg was the dose resulting in death of half of the patients. If more than 25 mg of digoxin was ingested by an adult without heart disease, death or progressive toxicity responsive only to digoxin- binding Fab antibody fragments resulted. Cardiac manifestations Cardiac manifestations are the most frequent and serious sign of both acute and chronic toxicity. Peak cardiac effects generally occur 3 to 6 hours following overdose and may persist for the ensuing 24 hours or longer. Digoxin toxicity may result in almost any type of arrhythmia. Multiple rhythm disturbances in the same patient are common. These include paroxysmal atrial tachycardia with variable atrioventricular (AV) block, accelerated junctional rhythm, slow atrial fibrillation (with very little variation in the ventricular rate) and bi directional ventricular tachycardia. Premature ventricular contractions (PVCs) are often the earliest and most common arrhythmia. Bigeminy or trigeminy also occur frequently. Sinus bradycardia and other bradyarrhythmias are very common. First, second, third degree heart blocks and AV dissociation are also common. Early toxicity may only be manifested by prolongation of the PR interval. Ventricular tachycardia may also be a manifestation of toxicity. Cardiac arrest from asystole or ventricular fibrillation due to digoxin toxicity is usually fatal. Acute massive digoxin overdose can result in mild to pronounced hyperkalaemia due to inhibition of the sodium-potassium (Na+-K+) pump. Hypokalaemia may contribute to toxicity (see Section 4.4). Non-cardiac manifestations Gastrointestinal symptoms are very common in both acute and chronic toxicity. The symptoms precede cardiac manifestations in approximately half of the patients in most literature reports. Anorexia, nausea and vomiting have been reported with an incidence up to 80%. These symptoms usually present early in the course of an overdose. Neurologic and visual manifestations occur in both acute and chronic toxicity. Dizziness, various CNS disturbances, fatigue and malaise are very common. The most frequent visual disturbance is an aberration of colour vision (predominance of yellow green). These neurological and visual symptoms may persist even after other signs of toxicity have resolved. In chronic toxicity, non-specific non-cardiac symptoms, such as malaise and weakness, may predominate. Paediatric population In children aged 1 to 3 years without heart disease, clinical observation suggests that an overdose of digoxin of 6 to 10 mg was the dose resulting in death in half of the patients. If more than 10 mg of digoxin was ingested by a child aged 1 to 3 years without heart disease, the outcome was uniformly fatal when Fab fragment treatment was not given. Most manifestations of chronic toxicity in children occur during or shortly after digoxin overdose. Cardiac manifestations The same arrhythmias or combination of arrhythmias that occur in adults can occur in paediatrics. Sinus tachycardia, supraventricular tachycardia, and rapid atrial fibrillation are seen less frequently in the paediatric population. Paediatric patients are more likely to present with an AV conduction disturbance or a sinus bradycardia. Ventricular ectopy is less common, however in massive overdose, ventricular ectopy, ventricular tachycardia and ventricular fibrillation have been reported. In neonates, sinus bradycardia or sinus arrest and/or prolonged PR intervals are frequent signs of toxicity. Sinus bradycardia is common in young infants and children. In older children, AV blocks are the most common conduction disorders. Any arrhythmia or alteration in cardiac conduction that develops in a child taking digoxin should be assumed to be caused by digoxin, until further evaluation proves otherwise. Non-cardiac manifestations The frequent non-cardiac manifestations are similar to those seen in adults are gastrointestinal, CNS and visual. However, nausea and vomiting are not frequent in infants and small children. In addition to the undesirable effects seen with recommended doses, weight loss in older age groups and failure to thrive in infants, abdominal pain due to mesenteric artery ischaemia, drowsiness and behavioural disturbances including psychotic manifestations have been reported in overdose. Treatment After recent ingestion, such as accidental or deliberate self-poisoning, the load available for absorption may be reduced by gastric lavage. Gastric lavage increases vagal tone and may precipitate or worsen arrhythmias. Consider pre-treatment with atropine if gastric lavage is performed. Treatment with digitalis Fab antibody usually renders gastric lavage unnecessary. In the rare instances in which gastric lavage is indicated, it should only be performed by individuals with proper training and expertise. Patients with massive digitalis ingestion should receive large doses of activated charcoal to prevent absorption and bind digoxin in the gut during enteroenteric recirculation. If hypokalaemia is present, it should be corrected with potassium supplements either orally or intravenously, depending on the urgency of the situation. In cases where a large amount of digoxin has been ingested hyperkalaemia may be present due to release of potassium from skeletal muscle. Before administering potassium in digoxin overdose the serum potassium level must be known. Bradyarrhythmias may respond to atropine but temporary cardiac pacing may be required. Ventricular arrhythmias may respond to lignocaine or phenytoin. Dialysis is not particularly effective in removing digoxin from the body in potentially life-threatening toxicity. Digoxin-specific antibody Fab is a specific treatment for digoxin toxicity and is very effective. Rapid reversal of the complications that are associated with serious poisoning by digoxin, digitoxin and related glycosides has followed I.V. administration of digoxin-specific (ovine) antibody fragments (Fab). For details, consult the literature supplied with antibody fragments.

שימוש לפי פנקס קופ''ח כללית 1994
Congestive heart failure, pulmonary edema, acute and chronic atrial fibrillation and flutter, other supraventricular arrhythmias
תאריך הכללה מקורי בסל
01/01/1995
הגבלות
תרופה שאושרה לשימוש כללי בקופ'ח
מידע נוסף
