Quest for the right Drug
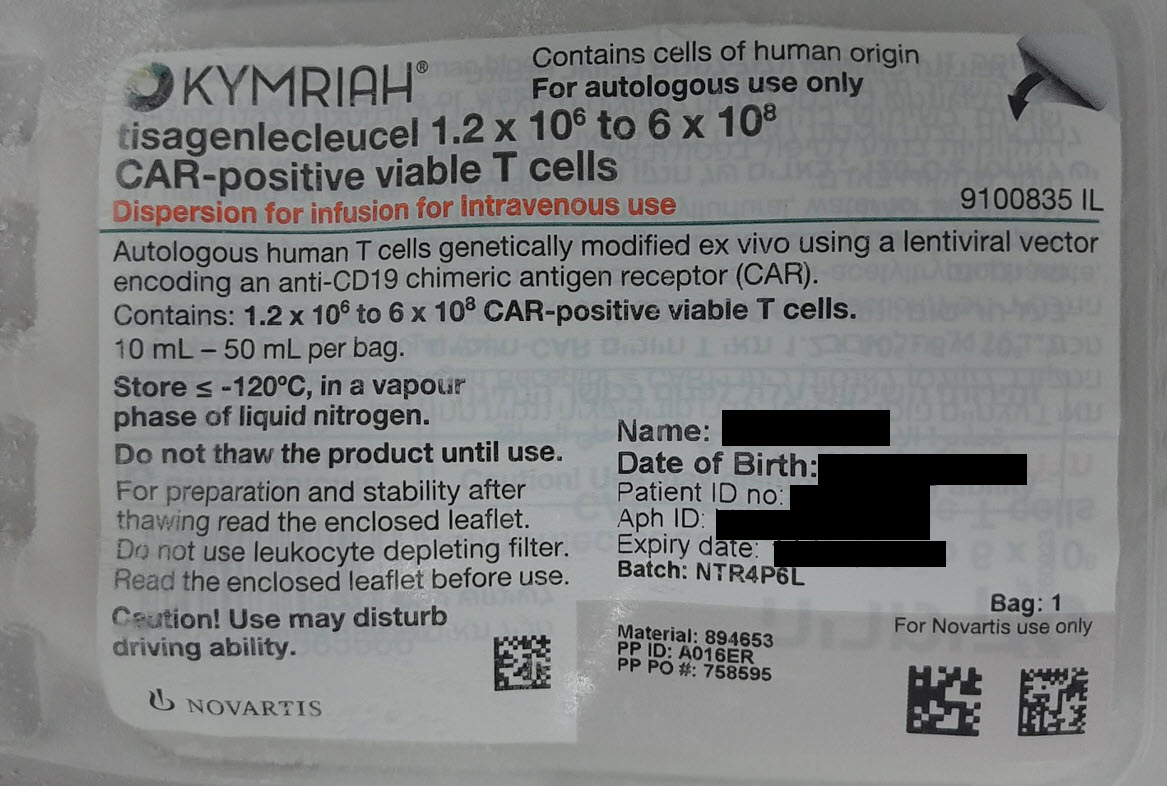
קימריה KYMRIAH (TISAGENLECLEUCEL)
תרופה במרשם
תרופה בסל
נרקוטיקה
ציטוטוקסיקה
צורת מתן:
תוך-ורידי : I.V
צורת מינון:
אין פרטים : DISPERSION FOR INFUSION
עלון לרופא
מינוניםPosology התוויות
Indications תופעות לוואי
Adverse reactions התוויות נגד
Contraindications אינטראקציות
Interactions מינון יתר
Overdose הריון/הנקה
Pregnancy & Lactation אוכלוסיות מיוחדות
Special populations תכונות פרמקולוגיות
Pharmacological properties מידע רוקחי
Pharmaceutical particulars אזהרת שימוש
Special Warning עלון לרופא
Physicians Leaflet
Adverse reactions : תופעות לוואי
4.8 Undesirable effects Summary of the safety profile Safety assessment was based on a total of 424 patients (with paediatric and young adult B-cell ALL, DLBCL and FL) who received Kymriah in three multicentre pivotal clinical studies. B-cell ALL The adverse reactions described in this section were characterised in 212 patients infused with Kymriah in the pivotal clinical study CCTL019B2202 and in the supportive studies CCTL019B2205J and CCTL019B2001X. The most common non-haematological adverse reactions were cytokine release syndrome (75%), infections (70%), hypogammaglobulinaemia (49%), pyrexia (43%) and decreased appetite (28%). The most common haematological laboratory abnormalities were decreased white blood cells (100%), decreased haemoglobin (99%), decreased neutrophils (98%), decreased lymphocytes (98%) and decreased platelets (95%). Grade 3 and 4 adverse reactions were reported in 86% of patients. The most common Grade 3 and 4 non-haematological adverse reaction was cytokine release syndrome (37%). The most common Grade 3 and 4 haematological laboratory abnormalities were white blood cells decreased (97%), lymphocytes decreased (94%), neutrophils decreased (96%), platelets decreased (70%) and haemoglobin decreased (46%). Grade 3 and 4 adverse reactions were more often observed within the initial 8 weeks post-infusion (78% of patients) compared to after 8 weeks post-infusion (49% of patients). DLBCL The adverse reactions described in this section were characterised in 115 patients infused with Kymriah in one global multicentre international study, i.e. the ongoing pivotal clinical study CCTL019C2201. The most common non-haematological adverse reactions were cytokine release syndrome (57%), infections (58%), pyrexia (35%), diarrhoea (31%), nausea (29%), fatigue (27%) and hypotension (25%). The most common haematological laboratory abnormalities were decreased lymphocytes (100%), decreased white blood cells (99%), decreased haemoglobin (99%), decreased neutrophils (97%), and decreased platelets (95%). Grade 3 and 4 adverse reactions were reported in 88% of patients. The most common Grade 3 and 4 non-haematological adverse reactions were infections (34%) and cytokine release syndrome (23%). The most common (>25%) Grade 3 and 4 haematological laboratory abnormalities were lymphocyte count decreased (95%), neutrophil count decreased (82%), white blood cell count decreased (78%), haemoglobin decreased (59%) and platelet count decreased (56%). Grade 3 and 4 adverse reactions were more often observed within the initial 8 weeks post-infusion (82%) compared to after 8 weeks post-infusion (48%). FL The adverse reactions described in this section were characterised in 97 patients infused with Kymriah in one global multicentre international study, i.e. the ongoing pivotal clinical study CCTL019E2202. The most common non-haematological adverse reactions (>25%) were cytokine release syndrome (50%), infections (50%) and headache (26%). The most common haematological laboratory abnormalities were decreased haemoglobin (94%), decreased lymphocytes (92%), decreased white blood cells (91%), decreased neutrophils (89%) and decreased platelets (89%). Grade 3 and 4 adverse reactions were reported in 75% of patients. The most common Grade 3 and 4 non-haematological adverse reactions were infections (16%). The most common (>25%) Grade 3 and 4 haematological laboratory abnormalities were lymphocyte count decreased (87%), white blood cell count decreased (74%), neutrophil count decreased (71%), platelet count decreased (26%) and haemoglobin decreased (25%). Grade 3 and 4 adverse reactions were more often observed within the initial 8 weeks post-infusion (70%) compared to after 8 weeks post-infusion (40%). Tabulated list of adverse reactions The adverse reactions described in this section were identified in 79, 115 and 97 patients in the ongoing multicentre pivotal clinical studies (CCTL019B2202, CCTL019C2201 and CCTL019E2202), as well as 64 and 69 patients in the supportive studies (CCTL019B2205J and CCTL019B2001X), and from post marketing reporting. Adverse drug reactions (Table 2) are listed by MedDRA system organ class. Within each system organ class, the adverse drug reactions are ranked by frequency, with the most frequent reactions first, using the following convention: very common (≥1/10); common (≥1/100 to <1/10); uncommon (≥1/1 000 to <1/100); rare (≥1/10 000 to <1/1 000); very rare (<1/10 000); not known (cannot be estimated from the available data). Within each frequency grouping, adverse drug reactions are presented in order of decreasing seriousness. Table 2 Adverse drug reactions Infections and infestations1) Very common: Infections - pathogen unspecified, viral infections, bacterial infections Common: Fungal infections Neoplasms benign, malignant and unspecified (incl cysts and polyps) Rare: Secondary malignancy of T-cell origin Blood and lymphatic system disorders Very common: Anaemia, febrile neutropenia, neutropenia, thrombocytopenia Common: Leukopenia, pancytopenia, coagulopathy, lymphopenia Uncommon: B-cell aplasia Immune system disorders Very common: Cytokine release syndrome, hypogammaglobulinaemia2) Common: Infusion-related reaction, graft-versus-host disease3), haemophagocytic lymphohistiocytosis Not known: Anaphylactic reaction Metabolism and nutrition disorders Very common: Decreased appetite, hypokalaemia, hypophosphataemia Common: Hypomagnesaemia, hypoalbuminaemia4), hyperglycaemia, hyponatraemia, hyperuricaemia5), hypercalcaemia, tumour lysis syndrome, hyperkalaemia, hyperphosphataemia6), hypernatraemia, hyperferritinaemia7), hypocalcaemia Uncommon: Hypermagnesaemia Psychiatric disorders Common: Anxiety, delirium8), sleep disorder9) Nervous system disorders Very common: Headache10), encephalopathy11) Common: Dizziness12), peripheral neuropathy13), tremor14), motor dysfunction15), seizure16), speech disorders17), neuralgia18) Uncommon: Ischaemic cerebral infarction, ataxia19), immune effector cell-associated neurotoxicity syndrome** Not known: Neurotoxicity Eye disorders Common: Visual impairment20) Cardiac disorders Very common: Tachycardia21) Common: Cardiac failure22), cardiac arrest, atrial fibrillation Uncommon: Ventricular extrasystoles Vascular disorders Very common: Haemorrhage23), hypotension24), hypertension Common: Thrombosis25), capillary leak syndrome Uncommon: Flushing Respiratory, thoracic and mediastinal disorders Very common: Cough26), dyspnoea27), hypoxia Common: Oropharyngeal pain28), pulmonary oedema29), nasal congestion, pleural effusion, tachypnoea Uncommon: Acute respiratory distress syndrome, lung infiltration Gastrointestinal disorders Very common: Diarrhoea, nausea, vomiting, constipation, abdominal pain30) Common: Stomatitis, abdominal distension, dry mouth, ascites Hepatobiliary disorders Common: Hyperbilirubinaemia Skin and subcutaneous tissue disorders Very common: Rash31) Common: Pruritus, erythema, hyperhidrosis, night sweats Musculoskeletal and connective tissue disorders Very common: Arthralgia, musculoskeletal pain32) Common: Myalgia Renal and urinary disorders Very common: Acute kidney injury33) General disorders and administration site conditions Very common: Pyrexia, fatigue34), oedema35), pain36) Common: Influenza-like illness, asthenia, multiple organ dysfunction syndrome, chills Investigations Very common: Lymphocyte count decreased*, white blood cell count decreased*, haemoglobin decreased*, neutrophil count decreased*, platelet count decreased*, hepatic enzyme increased37) Common: Blood bilirubin increased, weight decreased, blood fibrinogen decreased, international normalised ratio increased, fibrin D dimer increased, activated partial thromboplastin time prolonged, prothrombin time prolonged 1) Infections and infestations presented reflect high-level group terms. 2) Hypogammaglobulinaemia includes blood immunoglobulin A decreased, blood immunoglobulin G decreased, blood immunoglobulin M decreased, hypogammaglobulinaemia, immunodeficiency, immunodeficiency common variable and immunoglobulins decreased. 3) Graft-versus-host disease (GvHD) includes GvHD, GvHD in gastrointestinal tract, GvHD in skin 4) Hypoalbuminaemia includes blood albumin decreased, hypoalbuminaemia 5) Hyperuricaemia includes blood uric acid increased, hyperuricaemia 6) Hyperphosphataemia includes blood phosphorus increased, hyperphosphataemia 7) Hyperferritinaemia includes hyperferritinaemia, serum ferritin increased 8) Delirium includes agitation, delirium, hallucination, hallucination visual, irritability and restlessness. 9) Sleep disorder includes insomnia, nightmare and sleep disorder. 10) Headache includes headache and migraine. 11) Encephalopathy includes automatism, cognitive disorder, confusional state, depressed level of consciousness, disturbance in attention, encephalopathy, lethargy, memory impairment, mental status changes, metabolic encephalopathy, somnolence and thinking abnormal. Encephalopathy is a dominant feature of immune effector cell-associated neurotoxicity syndrome (ICANS), along with other symptoms. 12) Dizziness includes dizziness, presyncope and syncope. 13) Peripheral neuropathy includes dysaesthesia, hyperaesthesia, hypoaesthesia, neuropathy peripheral, paraesthesia and peripheral sensory neuropathy. 14) Tremor includes dyskinesia and tremor. 15) Motor dysfunction includes muscle spasms, muscle twitching, myoclonus and myopathy. 16) Seizure includes generalised tonic-clonic seizures, seizure and status epilepticus. 17) Speech disorders includes aphasia, dysarthria and speech disorders. 18) Neuralgia includes neuralgia and sciatica. 19) Ataxia includes ataxia and dysmetria. 20) Visual impairment includes vision blurred and visual impairment. 21) Tachycardia includes sinus tachycardia, supraventricular tachycardia, tachycardia 22) Cardiac failure includes cardiac failure, cardiac failure congestive, left ventricular dysfunction and right ventricular dysfunction. 23) Haemorrhage includes anal haemorrhage, blood blister, blood urine present, catheter site haemorrhage, cerebral haemorrhage, conjunctival haemorrhage, contusion, cystitis haemorrhagic, disseminated intravascular coagulation, duodenal ulcer haemorrhage, ecchymosis, epistaxis, eye contusion, gastrointestinal haemorrhage, gingival bleeding, haemarthrosis, haematemesis, haematochezia, haematoma, haematuria, haemoptysis, heavy menstrual bleeding, injection site haematoma, intermenstrual bleeding, large intestinal haemorrhage, lip haemorrhage, melaena, mouth haemorrhage, mucosal haemorrhage, oral blood blister, periorbital haematoma, peritoneal haematoma, petechiae, pharyngeal haemorrhage, postprocedural haemorrhage, pulmonary haemorrhage, purpura, rectal haemorrhage, retinal haemorrhage, stoma site haemorrhage, subcutaneous haematoma, subdural haematoma, subdural haemorrhage, tooth socket haemorrhage, tracheal haemorrhage, traumatic haematoma, tumour haemorrhage, upper gastrointestinal haemorrhage and vaginal haemorrhage. 24) Hypotension includes hypotension and orthostatic hypotension. 25) Thrombosis includes deep vein thrombosis, embolism, pulmonary embolism, thrombosis, vena cava thrombosis and venous thrombosis. 26) Cough includes cough, productive cough and upper-airway cough syndrome. 27) Dyspnoea includes acute respiratory failure, dyspnoea, dyspnoea exertional, respiratory distress and respiratory failure. 28) Oropharyngeal pain includes oral pain and oropharyngeal pain. 29) Pulmonary oedema includes acute pulmonary oedema and pulmonary oedema. 30) Abdominal pain includes abdominal discomfort, abdominal pain, abdominal pain lower, abdominal pain upper and gastrointestinal pain. 31) Rash includes dermatitis, dermatitis acneiform, dermatitis contact, rash, rash maculo-papular, rash papular and rash pruritic. 32) Musculoskeletal pain includes back pain, bone pain, flank pain, musculoskeletal chest pain, musculoskeletal pain, neck pain, non-cardiac chest pain. 33) Acute kidney injury includes acute kidney injury, anuria, azotaemia, blood creatinine abnormal, blood creatinine increased, blood urea increased, renal failure, renal tubular dysfunction and renal tubular necrosis. 34) Fatigue includes fatigue and malaise. 35) Oedema includes face oedema, fluid retention, generalised oedema, hypervolaemia, localised oedema, oedema peripheral, periorbital oedema and peripheral swelling. 36) Pain includes pain and pain in extremity. 37) Hepatic enzyme increased includes alanine aminotransferase increased, aspartate aminotransferase increased, blood alkaline phosphatase increased, hepatic enzyme increased, transaminases increased. * Frequency is based on laboratory values. Patients are counted only for the worst grade observed post baseline. ** Abbreviated as ICANS. Symptoms or signs can be progressive and may include aphasia, altered level of consciousness, impairment of cognitive skills, motor weakness, seizures, and cerebral oedema. Description of selected adverse drug reactions Cytokine release syndrome In the clinical studies in paediatric and young adult B-cell ALL (N=212), cytokine release syndrome was reported in 75% of patients (37% with Grade 3 or 4; 0.5% [1 patient] with fatal outcome). In the ongoing clinical study in DLBCL (N=115), cytokine release syndrome was reported in 57% of patients (23% with Grade 3 or 4). In the ongoing clinical study in FL (N=97), cytokine release syndrome was reported in 50% of patients. No Grade 3 or 4 events were reported. Cytokine release syndrome was graded per Penn criteria in the paediatric and young adult B-cell ALL and DLBCL studies as follows: Grade 1: mild reactions, reactions requiring supportive care; Grade 2: moderate reactions, reactions requiring intravenous therapies; Grade 3: severe reactions, reactions requiring low-dose vasopressors or supplemental oxygen; Grade 4: life-threatening reactions, those requiring high-dose vasopressors or intubation; Grade 5: death. Cytokine release syndrome was graded per the Lee criteria in the FL study as follows: Grade 1: mild general symptoms requiring symptomatic treatment; Grade 2: symptoms requiring moderate intervention such as low-flow oxygen supplementation or low-dose vasopressor; Grade 3: symptoms requiring aggressive intervention, such as high-flow oxygen supplementation and high-dose vasopressor; Grade 4: life-threatening symptoms requiring intubation; Grade 5: death. For clinical management of cytokine release syndrome, see section 4.4 and Table 1. Infections and febrile neutropenia In B-cell ALL patients severe infections (Grade 3 and higher), which can be life-threatening or fatal, occurred in 36% of patients after Kymriah infusion. The overall incidence (all grades) was 70% (unspecified 55%, viral 31%, bacterial 24% and fungal 12%) (see section 4.4). 41% of the patients experienced an infection of any type within 8 weeks after Kymriah infusion. In DLBCL patients severe infections (Grade 3 and higher), which can be life-threatening or fatal, occurred in 34% of patients. The overall incidence (all grades) was 58% (unspecified 48%, bacterial 15%, fungal 11% and viral 11%) (see section 4.4). 37% of the patients experienced an infection of any type within 8 weeks. In FL patients severe infections (Grade 3 or 4), occurred in 16% of patients. The overall incidence (all grades) was 50% (unspecified 36%, viral 17%, bacterial 6%, and fungal 2%) (see section 4.4). 19% of the patients experienced an infection of any type within 8 weeks. Severe febrile neutropenia (Grade 3 or 4) was observed in 26% of paediatric and young adult B-cell ALL patients, 17% of DLBCL patients and 12% of FL patients. See section 4.4 for the management of febrile neutropenia before and after Kymriah infusion. Prolonged cytopenias Cytopenias are very common based on prior chemotherapies and Kymriah therapy. All paediatric and young adult B-cell ALL patients had a Grade 3 or 4 cytopenia at some time after Kymriah infusion. Grade 3 and 4 cytopenias not resolved by day 28 after Kymriah infusion based on laboratory findings included decreased count of white blood cells (50%), neutrophils (56%), lymphocytes (43%), and thrombocytes (32%) and decreased haemoglobin (11%). All adult DLBCL patients had Grade 3 and 4 cytopenias at some time after Kymriah infusion. Grade 3 and 4 cytopenias not resolved by day 28 based on laboratory findings included decreased count of thrombocytes (39%), lymphocytes (29%), neutrophils (25%), and white blood cells (21%) and decreased haemoglobin (14%). In adult patients with FL, 99% had Grade 3 and 4 cytopenias at any time post Kymriah infusion. Grade 3 and 4 cytopenias not resolved by day 28 after Kymriah infusion based on laboratory findings included a decreased count of lymphocytes (23%), thrombocytes (17%), neutrophils (16%), white blood cells (13%) and decreased haemoglobin (3%). Neurological adverse reactions The majority of neurotoxic events occurred within 8 weeks following infusion and were transient. In paediatric and young adult B-cell ALL patients, serious neurological adverse reactions including manifestations of encephalopathy and/or delirium occurred in 32% of patients (10% were Grade 3 or 4) within 8 weeks after Kymriah infusion. In DLBCL patients, manifestations of encephalopathy and/or delirium occurred in 20% of patients (11% were Grade 3 or 4) within 8 weeks after Kymriah infusion. In FL patients, these occurred in 9% of patients (1% Grade 3 or 4) within 8 weeks after Kymriah infusion. Among the neurotoxic events in FL patients, immune effector cell-associated neurotoxicity syndrome (ICANS) occurred in 4% of patients (1% Grade 3 or 4), all within 8 weeks of Kymriah infusion. Hypogammaglobulinaemia Hypogammaglobulinaemia was reported in 49% of patients treated with Kymriah for r/r ALL,17% of patients with r/r DLBCL and 17% of patients with r/r FL. Pregnant women who have received Kymriah may have hypogammaglobulinaemia. Immunoglobulin levels should be assessed in newborns of mothers treated with Kymriah. Immunogenicity In clinical studies, humoral immunogenicity of tisagenlecleucel was measured by determination of anti-murine CAR19 antibodies (anti-mCAR19) in serum pre and post-administration. The majority of patients tested positive for pre-dose anti-mCAR19 antibodies in paediatric and young adult ALL (B2202, B2205J, B2001X, 84.0%), adult DLBCL (C2201, 93.9%) and adult FL (E2202, 66.0%) patients. Treatment-induced anti-mCAR19 antibodies were found in 40.5% of paediatric and young adult ALL (B2202), 8.7% of adult DLBCL and 28.7% of adult FL patients. Pre-existing and treatment-induced antibodies were not associated with an impact on clinical response nor did they have an impact on the expansion and persistence of tisagenlecleucel. There is no evidence that the presence of pre-existing and treatment-induced anti-mCAR19 antibodies impacts the safety or effectiveness of Kymriah. T-cell immunogenicity responses were not observed in paediatric and young adult B-cell ALL, adult r/r DLBCL and adult FL patients. Reporting of suspected adverse reactions Reporting suspected adverse reactions after authorisation of the medicinal product is important. It allows continued monitoring of the benefit/risk balance of the medicinal product. Any suspected adverse events should be reported to the Ministry of Health according to the National Regulation by using an online form https://sideeffects.health.gov.il/ And to Novartis using the following email address: Safetydest.israel@novaris.com

פרטי מסגרת הכללה בסל
א. התרופה תינתן לטיפול במקרים האלה:1. ילדים ומבוגרים צעירים שמלאו להם 3 שנים וטרם מלאו להם 25 שנים החולים בלוקמיה חוזרת או עמידה (רפרקטורית) מסוג CD19+ B cell Acute Lymphoblastic Leukemia (ALL).לעניין זה מחלה חוזרת תוגדר בחולה שקיבל שני קווי טיפול קודמים או שעבר השתלה של תאי גזע המטופואטיים.במהלך מחלתו יהיה החולה זכאי לטיפול באחת מאלה – Brexucabtagene autoleucel, Tisagenlecleucel. 2. מבוגרים החולים בלימפומה חוזרת או עמידה (רפרקטורית) מסוג Diffuse large B cell lymphoma, לאחר שני קווי טיפול ומעלה. במהלך מחלתו יהיה החולה זכאי לטיפול באחת מאלה – Axicabtagene ciloleucel, Tisagenlecleucel. 3. מבוגרים החולים בלימפומה פוליקולרית חוזרת או רפרקטורית לאחר שלושה קווי טיפול קודמים ומעלה. במהלך מחלתו יהיה החולה זכאי לטיפול באחת מאלה – Axicabtagene ciloleucel, Tisagenlecleucel. ב. מתן התרופה האמורה ייעשה לפי מרשם של מומחה בהמטולוגיה.
מסגרת הכללה בסל
התוויות הכלולות במסגרת הסל
| התוויה | תאריך הכללה | תחום קליני | Class Effect | מצב מחלה |
|---|---|---|---|---|
| מבוגרים החולים בלימפומה חוזרת או עמידה (רפרקטורית) מסוג Diffuse large B cell lymphoma, לאחר שני קווי טיפול ומעלה. במהלך מחלתו יהיה החולה זכאי לטיפול באחת מאלה – Axicabtagene ciloleucel, Tisagenlecleucel. | 16/01/2019 | המטולוגיה | DLBCL, Diffusa large B cell lymphoma | |
| ילדים ומבוגרים צעירים שמלאו להם 3 שנים וטרם מלאו להם 25 שנים החולים בלוקמיה חוזרת או עמידה (רפרקטורית) מסוג CD19+ B cell Acute Lymphoblastic Leukemia (ALL). לעניין זה מחלה חוזרת תוגדר בחולה שקיבל שני קווי טיפול קודמים או שעבר השתלה של תאי גזע המטופואטיים. | 16/01/2019 | המטולוגיה | ALL, Acute lymphoblastic leukemia | |
| מבוגרים החולים בלימפומה פוליקולרית חוזרת או רפרקטורית לאחר שלושה קווי טיפול קודמים ומעלה. במהלך מחלתו יהיה החולה זכאי לטיפול באחת מאלה – Axicabtagene ciloleucel, Tisagenlecleucel. | 01/02/2023 | המטולוגיה | לימפומה פוליקולרית, Follicular lymphoma | |
| ילדים ומבוגרים צעירים שמלאו להם 3 שנים וטרם מלאו להם 25 שנים החולים בלוקמיה חוזרת או עמידה (רפרקטורית) מסוג CD19+ B cell Acute Lymphoblastic Leukemia (ALL). לעניין זה מחלה חוזרת תוגדר בחולה שקיבל שני קווי טיפול קודמים או שעבר השתלה של תאי גזע המטופואטיים. במהלך מחלתו יהיה החולה זכאי לטיפול באחת מאלה – Brexucabtagene autoleucel, Tisagenlecleucel. | 01/02/2023 | המטולוגיה | ALL, Acute lymphoblastic leukemia |
שימוש לפי פנקס קופ''ח כללית 1994
לא צוין
תאריך הכללה מקורי בסל
16/01/2019
הגבלות
תרופה מוגבלת לרישום ע'י רופא מומחה או הגבלה אחרת
ATC
מידע נוסף
עלון מידע לצרכן
05.04.22 - עלון לצרכן אנגלית 05.04.22 - עלון לצרכן עברית 05.04.22 - עלון לצרכן ערבית 05.04.22 - עלון לצרכן 02.05.22 - עלון לצרכן אנגלית 05.04.22 - עלון לצרכן אנגלית 05.04.22 - עלון לצרכן עברית 05.04.22 - עלון לצרכן ערבית 05.04.22 - עלון לצרכן 05.04.22 - עלון לצרכן אנגלית 16.12.21 - עלון לצרכן אנגלית 07.08.22 - עלון לצרכן עברית 16.12.21 - עלון לצרכן ערבית 11.10.22 - עלון לצרכן אנגלית 11.10.22 - עלון לצרכן עברית 11.10.22 - עלון לצרכן ערבית 18.12.22 - עלון לצרכן אנגלית 18.12.22 - עלון לצרכן עברית 18.12.22 - עלון לצרכן ערבית 18.12.22 - עלון לצרכן 18.12.22 - עלון לצרכן אנגלית 18.12.22 - עלון לצרכן אנגלית 09.01.23 - עלון לצרכן עברית 28.02.23 - עלון לצרכן אנגלית 28.02.23 - עלון לצרכן עברית 28.02.23 - עלון לצרכן ערבית 04.08.23 - עלון לצרכן עברית 07.09.23 - עלון לצרכן אנגלית 07.09.23 - עלון לצרכן עברית 07.09.23 - עלון לצרכן ערבית 16.08.24 - עלון לצרכן עברית 12.09.24 - עלון לצרכן אנגלית 12.09.24 - עלון לצרכן ערבית 07.11.24 - עלון לצרכן עברית 10.02.20 - החמרה לעלון 09.06.21 - החמרה לעלון 22.11.21 - החמרה לעלון 07.08.22 - החמרה לעלון 05.09.22 - החמרה לעלון 09.01.23 - החמרה לעלון 04.08.23 - החמרה לעלון 28.12.23 - החמרה לעלון 19.08.24 - החמרה לעלוןלתרופה במאגר משרד הבריאות
קימריה