Quest for the right Drug
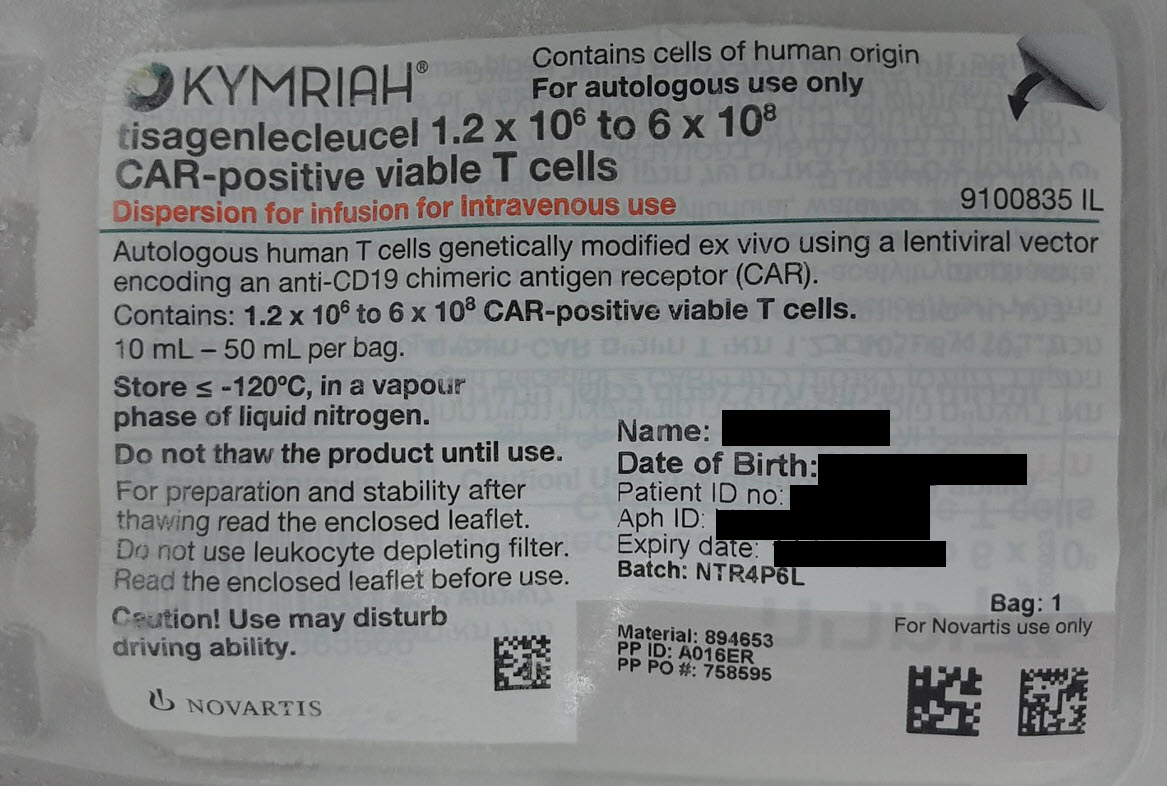
קימריה KYMRIAH (TISAGENLECLEUCEL)
תרופה במרשם
תרופה בסל
נרקוטיקה
ציטוטוקסיקה
צורת מתן:
תוך-ורידי : I.V
צורת מינון:
אין פרטים : DISPERSION FOR INFUSION
עלון לרופא
מינוניםPosology התוויות
Indications תופעות לוואי
Adverse reactions התוויות נגד
Contraindications אינטראקציות
Interactions מינון יתר
Overdose הריון/הנקה
Pregnancy & Lactation אוכלוסיות מיוחדות
Special populations תכונות פרמקולוגיות
Pharmacological properties מידע רוקחי
Pharmaceutical particulars אזהרת שימוש
Special Warning עלון לרופא
Physicians Leaflet
Pharmacological properties : תכונות פרמקולוגיות
Pharmacodynamic Properties
5.1 Pharmacodynamic properties Pharmacotherapeutic group: Antineoplastic agents, other antineoplastic agents, ATC code: L01XL04 Mechanism of action Tisagenlecleucel is an autologous, immunocellular cancer therapy which involves reprogramming a patient’s own T cells with a transgene encoding a chimeric antigen receptor (CAR) to identify and eliminate CD19 expressing cells. The CAR is comprised of a murine single chain antibody fragment which recognises CD19 and is fused to intracellular signalling domains from 4-1BB (CD137) and CD3 zeta. The CD3 zeta component is critical for initiating T-cell activation and anti-tumour activity, while 4-1BB enhances the expansion and persistence of tisagenlecleucel. Upon binding to CD19-expressing cells, the CAR transmits a signal promoting T-cell expansion and persistence of tisagenlecleucel. Clinical efficacy and safety Acute lymphoblastic leukaemia (ALL) The safety and efficacy of Kymriah treatment in paediatric and young adult patients up to and including 25 years of age, with relapsed or refractory (r/r) B-cell ALL were evaluated in a total of 203 patients in one pivotal (B2202, N=79) and two supportive (B2205J, N=64, and B2101J, N=60) open-label, single-arm phase I/II studies. All patients had leukapheresis products collected and cryopreserved prior to or during study entry. The pivotal study B2202 (ELIANA) is a multicentre, single-arm phase II study in paediatric and young adult patients with r/r B-cell ALL. Of 97 patients enrolled in the main cohort, 79 received infusion with Kymriah; for 8 patients (8%) Kymriah could not be manufactured; reasons for discontinuation prior to Kymriah infusion included death (n=7; 7%) or adverse events (n=3; 3%) while awaiting Kymriah manufacturing in the clinical study. The median duration of study follow-up defined as the time from Kymriah infusion to the date of completion or discontinuation from follow-up prior to the data cut-off date was 28.5 months (range: 0.4-65.5). The median time from Kymriah infusion to the data cut-off date was 79.4 months (range: 59.7-90.3). Key baseline information for enrolled and infused patients is presented in Table 3. The majority of patients (69/79, 87%) received bridging therapy while waiting for Kymriah. A total of 76 out of 79 patients (96%) who received Kymriah infusion also received lymphodepleting chemotherapy after enrolment and prior to infusion of a single dose of Kymriah (see section 4.2 for condition of lymphodepleting chemotherapy). Table 3 Study B2202: Baseline information across the enrolled and the infused patient population Enrolled Infused N=97 N=79 n (%) n (%) Age (years) Mean (standard deviation) 12 (5.48) 12 (5.38) Median (minimum – maximum) 11 (3 – 27) 11 (3 – 24) Age category (years) - n (%) <10 years 40 (41.2) 32 (40.5) ≥10 years and <18 years 40 (41.2) 33 (41.8) ≥18 years 17 (17.5) 14 (17.7) Sex - n (%) Male 54 (55.7) 45 (57.0) Female 43 (44.3) 34 (43) Disease status - n (%) Primary refractory1 8 (8.2) 6 (7.6) Relapsed disease2 89 (91.8) 73 (92.4) Prior stem-cell transplantation - n (%) 0 39 (40.2) 31 (39.2) 1 50 (51.5) 42 (53.2) 2 8 (8.2) 6 (7.6) 1 Primary refractory: Never had a morphologic complete remission (CR) prior to the study; 2 Relapsed disease: Had at least one relapse prior to the study Efficacy was established through the primary endpoint of overall remission rate (ORR), which includes best overall response as complete remission (CR) or complete remission with incomplete blood count recovery (CRi) within 3 months post infusion, as determined by Independent Review Committee (IRC) assessment, as well as secondary endpoints including duration of remission (DOR) and the proportion of patients who achieved CR or CRi with minimal residual disease (MRD) <0.01% by flow cytometry (MRD-negative). See Table 4 for efficacy results from this study. ORR was consistent across all subgroups. Eight patients (10.1%) who achieved CR/CRi after Kymriah infusion went to haematopoietic stem cell transplant while in remission of which 6 of the patients (7.6%) proceeded to transplant within the first 6 months post-infusion while in remission. Kymriah was administered in a qualified Kymriah treatment centre in an inpatient and outpatient setting. Table 4 Study B2202: Efficacy results in paediatric and young adult patients with relapsed/refractory B-cell acute lymphoblastic leukaemia (ALL) Enrolled patients Infused patients Primary endpoint N=97 N=79 Overall remission rate (ORR) within 3 months1,2, 65 (67.0) 65 (82.3) n (%) (56.7, 76.2) (72.1, 90.0) 95% CI p<0.0001 p<0.0001 CR3, n (%) 49 (50.5) 49 (62.0) CRi4, n (%) 16 (16.5) 16 (20.3) Key secondary endpoint N=97 N=79 CR or CRi with MRD negative bone marrow5,6, n 64 (66.0) 64 (81.0) (%) (55.7, 75.3) (70.6, 89.0) 95% CI p<0.0001 p<0.0001 Duration of remission (DOR)7 N=66 N=66 % event free probability at 12 months 67.4 67.4 % event free probability at 30 months 56.2 56.2 Median (months) (95% CI) 46.8(17.8, NE9) 46.8 (17.8, NE) Other secondary endpoint N=97 N=79 Overall survival (OS)8 % survival probability at 36 months 52.8 63.5 Median (months) (95% CI) 47.9 (19.4, NE) Not reached (45.6, NE) 1 Requires remission status to be maintained for at least 28 days without clinical evidence of relapse. 2 Nominal one-sided exact p-value based on H0: ORR ≤20% vs. Ha: ORR >20% 3 CR (complete remission) was defined as <5% of blasts in the bone marrow, circulating blasts in blood should be <1%, no evidence of extramedullary disease, and full recovery of peripheral blood counts (platelets >100,000/μL and absolute neutrophil counts [ANC] >1 000/μL) without blood transfusion. 4 CRi (complete remission with incomplete blood count recovery) was defined as <5% of blasts in the bone marrow, circulating blasts in blood should be <1%, no evidence of extramedullary disease, and without full recovery of peripheral blood counts with or without blood transfusion. 5 MRD (minimal residual disease) negative was defined as MRD by flow cytometry <0.01%. 6 Nominal one-sided exact p-value based on H0: Rate of MRD negative remission ≤15% vs. Ha: >15%. 7 DOR was defined as time since onset of CR or CRi to relapse or death due to underlying indication, whichever is earlier (N=66). One patient achieved remission after month 3. 8 OS was defined as time from date of Kymriah infusion to the date of death due to any cause for infused patients and from time of date of enrolment to the date of death due to any cause for enrolled patients. 9 Not estimable The supportive study B2205J (ENSIGN) was a multicentre single-arm phase II study in paediatric and young adult patients with r/r B‑cell ALL. The study had similar study design and enrolled comparable patient populations as the pivotal study B2202. The main difference between the two studies was the definition of the primary efficacy endpoint ORR, which was measured within 6 months after Kymriah infusion in study B2205J compared to 3 months in the pivotal study. Of 75 patients enrolled, 64 received infusion of Kymriah; for 5 patients (6.7%), Kymriah could not be manufactured and 6 patients (8.0%) died while awaiting Kymriah manufacturing in the clinical study. The median duration of study follow-up defined as the time from Kymriah infusion to the date of completion or discontinuation from follow-up prior to the data cut-off date in the final analyses was 12.2 months (range: 0.4-49.3). The median time from Kymriah infusion to the data cut-off date was 31.7 months (range: 17.6-56.0). Among the patients infused, the median age was 12.5 years (range: 3 to 25), 34 (53.1%) were female and 30 (46.9%) were male, 10.9% had primary refractory disease, 89.1% had relapsed disease, and 43.8% of patients had at least one prior haematopoietic stem cell transplant. Baseline disease characteristics were similar in the enrolled patients with regard to age (median age 13.0 years, range: 3 to 25), gender (46.7% female and 53.3% male), primary refractoriness (10.7%), and prior transplant history (42.7%). The majority of infused patients (57/64, 89.1%) received bridging chemotherapy while waiting for Kymriah. A total of 60 out of 64 patients (93.8%) who received Kymriah infusion also received lymphodepleting chemotherapy after enrolment and prior to infusion of a single dose of Kymriah. Efficacy was established through the primary endpoint of ORR, which included best overall response as CR or CRi that were maintained for at least 28 days within 6 months post-infusion, as determined by IRC assessment, as well as secondary endpoints including DOR, proportion of patients who achieved CR or CRi with MRD-negative disease status, and OS. Among the patients infused, ORR was demonstrated in 45 patients (70.3%; 59.4% CR and 10.9% CRi). CR/CRi with MRD-negative bone marrow was reported in 43 patients (67.2%). The median DOR was not reached and the event-free probability at 12 months was 70.5%. The survival probability at 24 months was 54.7%, and the median OS was estimated as 29.9 months (95% CI: 15.1, 42.4). The OS results were confirmed in an updated OS analyses (i.e. median OS 29.9 months [95% CI: 15.2, NE] with 57.6% survival probability at 24 months; with a median follow-up for OS of 25.9 months), which included patients transitioned to a separate long-term follow-up study. Seven patients (10.9%) who achieved CR/CRi after Kymriah infusion proceeded to haematopoietic stem cell transplant while in remission during the study, of which 5 of the patients (7.8%) proceeded to transplant within the first 6 months post-infusion. Efficacy results reported for the enrolled patients (n=75) demonstrate an ORR of 60.0% (50.7% CR and 9.3% CRi; 57.3% with MRD-negative bone marrow). The reported overall survival in the enrolled population is in accordance with the infused population. Special populations No differences in efficacy or safety were observed between different age subgroups. Patients with active CNS leukaemia Of four patients with active CNS leukaemia (i.e. CNS-3) included in study B2101J, three experienced cytokine release syndrome (Grade 2-4) and transient neurological abnormalities (Grade 1-3) that resolved within 1-3 months of infusion. One patient died due to disease progression and the remaining three patients achieved a CR or CRi and remain alive 1.5-2 years after infusion. Diffuse large B-cell lymphoma (DLBCL) The safety and efficacy of Kymriah treatment in adult patients with relapsed or refractory (r/r) diffuse large B-cell lymphoma (DLBCL) who received ≥2 lines of chemotherapy, including rituximab and anthracycline, or relapsed following autologous haematopoietic stem cell transplantation (HSCT), was evaluated in the multicentre, open-label, pivotal, single-arm phase II study C2201 (JULIET). Patients with T-cell rich/histiocyte-rich large B-cell lymphoma (THRBCL), primary cutaneous large B-cell lymphoma, primary mediastinal B-cell lymphoma (PMBCL), EBV-positive DLBCL of the elderly, Richter’s transformation, and Burkitt lymphoma were not enrolled in study C2201. Of 167 patients enrolled in study C2201, 115 patients received infusion with Kymriah. Approximately 31% of patients discontinued the study prior to Kymriah infusion. For 13 patients (8%) Kymriah could not be manufactured. Other reasons for discontinuation prior to Kymriah infusion included death (n=16; 10%), physician decision/primary disease progression (n=16; 10%), patient decision (n=2; 1%), protocol deviation (n=1; 1%) or adverse events (n=4; 2%) while awaiting Kymriah manufacturing in the clinical study. The median duration of study follow-up defined as the time from Kymriah infusion to date of completion or discontinuation from follow-up prior to the data cut-off date in the final analysis was 7.7 months (range: 0.4-61.0). The median time from Kymriah infusion to the data cut-off date in the final analysis was 74.3 months (range: 58.1-86.6). Key baseline information for enrolled and infused patients is presented in Table 5. All patients had leukapheresis starting material collected and cryopreserved prior to or during study entry. The majority of patients (103/115, 90%) received bridging therapy for disease stabilisation. The type and duration of bridging therapy was left to the discretion of the physician. 107/115 patients (93%) received lymphodepleting chemotherapy prior to Kymriah infusion. Kymriah was given as a single-dose (0.6-6.0 × 108 CAR-positive viable T cells) intravenous infusion in a qualified Kymriah treatment centre in an inpatient and outpatient setting. Table 5 Study C2201: Baseline information across the enrolled and the infused patient populations Enrolled Infused N=167 N=115 n (%) n (%) Age (years) Mean (standard deviation) 56 (12.9) 54 (13.1) Median (minimum – maximum) 58 (22 - 76) 56 (22 - 76) Age category (years) - n (%) <65 years 120 (71.9) 89 (77.4) ≥65 years 47 (28.1) 26 (22.6) Sex - n (%) Male 105 (62.9) 71 (61.7) Female 62 (37.1) 44 (38.3) Prior haematopoietic stem cell transplant (SCT) - n (%) No 93 (55.7) 59 (51.3) Yes 74 (44.3) 56 (48.7) Stage III/IV disease at study entry - n (%) No 36 (21.6) 27 (23.5) Yes 131 (78.4) 88 (76.5) Number of prior lines of antineoplastic therapy – n (%) 1 6 (3.6) 5 (4.3) 2 73 (43.7) 51 (44.3) 3 52 (31.1) 36 (31.3) ≥4 36 (21.6) 23 (20.0) Disease status - n (%) Refractory to last line of therapy 98 (58.7) 63 (54.8) Relapse to last line of therapy 69 (41.3) 52 (45.2) The efficacy of Kymriah was evaluated through the primary endpoint of best overall response rate (ORR), which includes complete response (CR) and partial response (PR) as determined by Independent Review Committee (IRC) assessment as well as secondary endpoints including duration of response (Table 6). Table 6 Study C2201: Efficacy results in adult patients with relapsed or refractory diffuse large B-cell lymphoma (DLBCL) after two or more lines of systemic therapy Enrolled patients Infused patients N=167 N=115 Primary endpoint1 N=147 N=99 Overall response rate (ORR) (CR+PR)2, n (%) 54 (36.7) 54 (54.5) 95% CI (28.9, 45.1) (44.2, 64.6) CR, n (%) 41 (27.9) 41 (41.4) PR, n (%) 13 (8.8) 13 (13.1) Response at month 3 N=147 N=99 ORR (%) 40 (27.2) 40 (40.4) CR (%) 34 (23.1) 34 (34.3) Response at month 6 N=147 N=99 ORR (%) 34 (23.1) 34 (34.3) CR (%) 31 (21.1) 31 (31.3) Duration of response (DOR)3 N=54 N=54 Median (months) (95% CI) Not reached (10.0, NE5) Not reached (10.0, NE5) % relapse free probability at 12 months 63.4 63.4 % relapse free probability at 24 months 60.8 60.8 % relapse free probability at 36 months 60.8 60.8 % relapse free probability at 54 months 60.8 60.8 Other secondary endpoints N=167 N=115 Overall survival (OS)4 % survival probability at 12 months 41.0 48.2 % survival probability at 36 months 29.4 36.6 % survival probability at 60 months 25.5 31.7 Median (months) (95% CI) 8.2 (5.8, 11.7) 11.1 (6.6, 23.9) 1 The primary endpoint was analysed on all patients whose Kymriah was manufactured at the Novartis US facility. 2 ORR is the proportion of patients with best overall response (BOR) of CR or PR based on the Lugano response criteria (Cheson 2014); non-infused patients were assigned BOR=Unknown (i.e. non-responders). 3 DOR was defined as time from achievement of CR or PR to relapse or death due to DLBCL, whichever occurs first. 4 OS was defined as time from date of Kymriah infusion to the date of death due to any cause (N=115) and time from date of enrolment to the date of death due to any cause for enrolled patients (N=167). 5 Not estimable. Among 41 patients who achieved CR, 16 patients initially had an overall disease response of PR which improved to CR over time; most patients (13/16) achieved PR to CR conversion within 6 months post-tisagenlecleucel infusion. ORR was consistent across subgroups. Follicular lymphoma (FL) The safety and efficacy of Kymriah treatment in adult patients with relapsed or refractory (r/r) follicular lymphoma (FL) were evaluated in an open label, multicentre, single-arm, phase II study (E2202, N=97). The pivotal study E2202 (ELARA) included patients who were refractory to or relapsed within 6 months after completion of a second or later line of systemic therapy (including an anti-CD20 antibody and an alkylating agent), relapsed during or within 6 months after completion of anti-CD20 antibody maintenance therapy following at least two lines of therapy, or relapsed after autologous haematopoietic stem cell transplant (HSCT). The study excluded patients with active or serious infections, transformed lymphoma or other aggressive lymphomas, including patients with FL Grade 3b, those who had received prior allogeneic HSCT, or who had disease with active CNS involvement. Of 98 patients who were enrolled and underwent leukapheresis, 97 patients received infusion with Kymriah. One patient achieved a complete response prior to infusion which was attributed to their prior last line of therapy and was subsequently discontinued from the study due to physician decision prior to infusion. All patients had leukapheresis products collected and cryopreserved prior to or during study entry. Kymriah was delivered for all enrolled patients. The median duration of study follow-up defined as the time from Kymriah infusion to date of completion or discontinuation from follow-up prior to the data cut-off date was 18.6 months (range: 1.8-29.9). The median time from Kymriah infusion to the data cut-off date was 20.8 months (range: 14.4-29.9). The study is still ongoing. Of the 97 patients infused with Kymriah, 94 patients had measurable disease at baseline per Independent Review Committee (IRC) and are included in the efficacy analysis set (EAS). Key baseline information for the enrolled set and EAS is presented in Table 7. Approximately half of the patients (44/94; 47%) received bridging therapy for disease stabilisation between leukapheresis and administration of Kymriah and all patients received lymphodepleting chemotherapy. For all infused patients, Kymriah was administered as a single dose intravenous infusion in a qualified treatment centre in an inpatient or outpatient (18%) setting. Table 7 Study E2202: Baseline information across the enrolled and the EAS patient populations Enrolled EAS* N=98 N=94 n (%) n (%) Age (years) Mean (standard deviation) 56.5 (10.34) 56.4 (10.54) Median (minimum – maximum) 57.5 (29-73) 57.0 (29-73) Age category (years) – n (%) <65 years 74 (75.5) 70 (74.5) ≥65 years 24 (24.5) 24 (25.5) Sex – n (%) Male 65 (66.3) 64 (68.1) Female 33 (33.7) 30 (31.9) Stage III/IV disease at study entry – n (%) 84 (85.7) 81 (86.2) High FLIPI score1 – n (%) 59 (60.2) 57 (60.6) 2 Bulky disease at baseline – n (%) 62 (63.3) 61 (64.9) Number of prior lines of antineoplastic therapy – n (%) 2 24 (24.5) 24 (25.5) 3 21 (21.4) 19 (20.2) 4 25 (25.5) 24 (25.5) ≥5 28 (28.6) 27 (28.7) Median (minimum – maximum) 4.0 (2.0 -13.0) 4.0 (2.0 - 13.0) Disease status – n (%) Refractory to last line of therapy 76 (77.6) 74 (78.7) Relapse to last line of therapy 17 (17.3) 17 (18.1) Double refractory3 – n (%) 67 (68.4) 65 (69.1) Progression of disease within 24 months 61 (62.2) 61 (64.9) (POD24)4 – n (%) Prior haematopoietic stem cell transplant (HSCT) – n (%) 36 (36.7) 35 (37.2) Prior PI3K inhibitor – n (%) 21 (21.4) 19 (20.2) * Infused patients who had measurable disease at baseline per Independent Review Committee (IRC) and are included in the efficacy analysis set. 1 FLIPI includes 5 labelled prognostic factors; FLIPI = sum (where prognostic factor = ‘Yes’); Low: 0-1 criteria met; intermediate: 2 criteria met; high: 3 or more met. 2 Bulky disease defined per IRC as imaging showing any nodal or extra nodal tumour mass that is >7 cm in diameter or involvement of at least 3 nodal sites, each with a diameter >3 cm. 3 Double refractory is defined as patients who failed to respond or relapsed within 6 months following therapy with anti-CD20 and alkylating agents, any regimen. 4 POD24: subjects with primary refractory or experiencing progression of disease within 24 months from initiation of a first-line anti-CD20 mAb containing treatment. Efficacy was evaluated through the primary endpoint of complete response rate (CRR), recorded from infusion until progressive disease or start of new therapy. CRR was determined by IRC based on Lugano classification criteria (Cheson 2014). Secondary endpoints included overall response rate (ORR), duration of response (DOR), progression-free survival (PFS), overall survival (OS). Median time from enrolment to infusion was 46 days (range: 23 to 127). The first disease assessment was scheduled to be performed at month 3 post-infusion. Table 8 Study E2202: Efficacy results in adult patients with relapsed or refractory follicular lymphoma (FL) after two or more lines of therapy Enrolled patients EAS patients* N=98 N=94 Complete response rate (CRR)1, per IRC n (%) 67 (68.4) 65 (69.1) 95% CI (58.2, 77.4) (58.8, 78.3) Overall response rate (ORR)2, per IRC n (%) 84 (85.7) 81 (86.2) Duration of response (DOR)3, per IRC N=84 N=81 Median (months) (95% CI) NE (20.9, NE) NE (15.6, NE) % event-free probability at 9 months (95% CI) 75.9 (64.8, 83.9) 76.2 (64.9, 84.3) CI=Confidence interval, NE=Not estimable * Infused patients who had measurable disease at baseline per Independent Review Committee (IRC) and are included in the efficacy analysis set. 1 The primary endpoint was CRR per IRC based on Lugano response criteria (Cheson 2014) and defined as the proportion of patients with a best overall response (BOR) of complete response (CR). The non-infused patient was treated as a non-responder. 2 ORR was defined as the proportion of patients with a BOR of CR or partial response (PR). The non- infused patient was treated as a non-responder. 3 DOR was defined as time from achievement of CR or PR to relapse or death due to FL, whichever occurs first. All responders achieved their first response (CR or PR) at the first disease assessment performed post- infusion, at 3 months. Of the 65 patients who eventually achieved a CR, 15 patients (16%) initially had a PR. The majority of patients converted from PR to CR within 6 months post-infusion. No patient who received Kymriah infusion went to transplant while in response (CR or PR). The probability for a patient to remain in response (DOR) ≥9 months was 76% (95% CI: 64.9, 84.3), while the probability for a patient who achieved a CR to remain in response ≥9 months was 87% (95% CI: 75.6, 93.3). Subgroup analyses demonstrated a generally consistent CRR across all subgroups, including the following high-risk prognostic subgroups: high FLIPI score (CRR of 63%), prior HSCT (CRR of 66%), POD24 (CRR of 59%), and double refractoriness (CRR of 66%). Special populations There are not enough data to determine whether there are any differences in efficacy or safety between different age subgroups, although the clinical benefit and safety experience in elderly patients with DLBCL and FL above the age of 65 years (23% and 24.7% of the study population for DLBCL and FL, respectively) were comparable to the overall population.
Pharmacokinetic Properties
5.2 Pharmacokinetic properties Following infusion of Kymriah into paediatric and young adult r/r B-cell ALL, r/r DLBCL and r/r FL patients, tisagenlecleucel typically exhibited an initial rapid expansion followed by a slower bi-exponential decline. High inter-subject variability was associated with the in vivo exposure metrics (AUC0-28d and Cmax) across all indications. Cellular kinetics in paediatric and young adult B-cell ALL patients A summary of cellular kinetic parameters of tisagenlecleucel in paediatric and young adult B-cell ALL patients is provided in Table 9 below. The maximal expansion (Cmax) was approximately 1.5-fold higher in CR/CRi patients (n=114) compared with non-responding (NR) patients (n=10) as measured by qPCR. Delayed and lower expansion was observed in NR patients compared to CR/CRi patients. Table 9 Cellular kinetic parameters of tisagenlecleucel in paediatric and young adult r/r B-cell ALL (Studies B2202 and B2205J) Parameter Summary statistics Responding patients Non-responding (CR/CRi) patients (NR) N=114 N=12 Cmax (copies/μg) Geometric mean 32 900 (173.8), 114 21 900 (80.7), 10 (CV%), n Tmax‡ (day) Median [min;max], n 9.85 [5.70; 54.8], 114 20.1 [12.6; 62.7], 10 AUC0-28d Geometric mean 286 000 (194.9), 114 232 000 (104.5), 8 (copies/μg*day) (CV%), n T½ (day) Geometric mean 40.0 (436.8), 72 3.78 (222.0), 4 (CV%), n Tlast (day) Median [min;max], n 190 [17.8; 1 860], 114 28.8 [13.9; 888], 11 Cellular kinetics in adult DLBCL patients A summary of cellular kinetic parameters of tisagenlecleucel in DLBCL patients is provided in Table 10 below. Table 10 Cellular kinetic parameters of tisagenlecleucel in r/r DLBCL patients Parameter Summary statistics Responding patients Non-responding patients (CR and PR) (SD/PD/Unknown) N=44 N=71 Cmax (copies/μg) Geometric mean 6 070 (256.8), 44 5 000 (391.7), 67 (CV%), n Tmax (day) Median [min;max], n 9.02 [5.78; 27.7], 44 8.84 [0.994; 26.7], 67 AUC0-28d Geometric mean 63 000 (177.7), 43 52 300 (321.4), 62 (copies/μg*day) (CV%), n T½ (day) Geometric mean 151 (487.5), 31 11.6 (196.2), 49 (CV%), n Tlast (day) Median [min;max], n 930 [17.1; 1 830], 44 41.9 [0.994; 1 480], 67 Cellular kinetics in FL patients A summary of cellular kinetic parameters of tisagenlecleucel in FL patients by BOR is provided in Table 11 below. The geometric mean AUC0-28d value of responders was 2.9 fold higher compared to non-responders, while the geometric mean Cmax value was 2.1 fold higher in responders compared to non-responders. Table 11 Cellular kinetic parameters of tisagenlecleucel in r/r FL patients Parameter Summary statistics Responding patients Non-responding (CR and PR) patients N=81 (SD/PD) N=12 Cmax Geometric mean (CV%), n 6 280 (331), 67 3 000 (1 190), 8 (copies/micrograms) Tmax (day) Median [min;max], n 9.92 [2.62; 28.0], 67 13.0 [7.73; 16.0], 8 AUC0-28d Geometric mean (CV%), n 57 500 (261), 66 20 100 (18 100), 7 (copies/micrograms*day) T½ (day) Geometric mean (CV%), n 43.8 (287), 43 24.4 (180), 6 Tlast (day) Median [min;max], n 191 [19.9; 558], 73 107 [18.7; 366], 10 Biodistribution In paediatric and young adult B-cell ALL patients, tisagenlecleucel has been shown to be present in the blood and bone marrow for up to 5 years and 6 months, respectively. The blood to bone marrow partitioning of tisagenlecleucel in bone marrow was 50% of that present in blood at day 28 while at both months 3 and 6 it distributes at 67% (Studies B2202 and B2205J). Tisagenlecleucel also traffics and persists in cerebrospinal fluid in paediatric and young adult B-cell ALL patients (Study B2101J) for up to 1 year. In adult DLBCL patients (Study C2201), tisagenlecleucel has been detected for up to 5 years in peripheral blood and up to month 9 in bone marrow for complete responder patients. The blood to bone marrow partitioning in bone marrow was nearly 70% of that present in blood at day 28 and 50% at month 3 in both responder and non-responder patients. In adult FL patients (Study E2202), tisagenlecleucel has been detected for up to 18 months in peripheral blood and up to month 3 in bone marrow for complete responder patients. The blood to bone marrow partitioning in bone marrow was nearly 54% of that present in blood at month 3 in both responder and non-responder patients. Elimination The elimination profile of Kymriah includes a bi-exponential decline in peripheral blood and bone marrow. Linearity/non-linearity There is no apparent relationship between dose and AUC0-28d or Cmax. Special populations Elderly The scatter plots of cellular kinetic parameters versus age (22 to 76 years in DLBCL patients and 29 to 73 years in FL patients) revealed no relevant relationship between cellular kinetic parameters (AUC0-28d and Cmax) with age. Gender Gender has not been identified as a significant characteristic influencing tisagenlecleucel expansion in B-cell ALL, DLBCL and FL patients. In Study B2202, there were 43% female and 57% male patients, in Study C2201 38% female and 62% male patients and in Study E2202 34% female and 66% male patients who received Kymriah. Further, in Study E2202, the geometric means of the exposure parameters (Cmax and AUC0-28d) were shown to be 111% and 106% higher, respectively, in female patients compared to male patients. Although the interpretation of expansion in relation to gender is difficult due to overlapping ranges and high inter-subject variability. Race/ethnicity There is limited evidence that race/ethnicity impact the expansion of Kymriah in paediatric and young adult ALL, DLBCL and FL patients. In Study B2202 there were 73.4% Caucasian, 12.7% Asian and 13.9% other ethnic patients. In Study C2201 there were 85% Caucasian, 9% Asian, 4% Black or African American patients, and 3 patients (3%) of unknown race. In Study E2202, there were 75% Caucasian, 13% Asian, 1% Black or African American patients, and 10% of unknown race. Body weight In ALL, DLBCL and FL patients, across the weight ranges (ALL; 14.4 to 137 kg; DLBCL: 38.3 to 186.7 kg; FL: 44.3 to 127.7 kg), the scatter plots of qPCR cellular kinetic parameters versus weight revealed no apparent relationship between cellular kinetic parameters with weight. Prior transplantation Prior transplantation did not impact the expansion/persistence of Kymriah in paediatric and young adult B-cell ALL patients, adult DLBCL or adult FL patients.

פרטי מסגרת הכללה בסל
א. התרופה תינתן לטיפול במקרים האלה:1. ילדים ומבוגרים צעירים שמלאו להם 3 שנים וטרם מלאו להם 25 שנים החולים בלוקמיה חוזרת או עמידה (רפרקטורית) מסוג CD19+ B cell Acute Lymphoblastic Leukemia (ALL).לעניין זה מחלה חוזרת תוגדר בחולה שקיבל שני קווי טיפול קודמים או שעבר השתלה של תאי גזע המטופואטיים.במהלך מחלתו יהיה החולה זכאי לטיפול באחת מאלה – Brexucabtagene autoleucel, Tisagenlecleucel. 2. מבוגרים החולים בלימפומה חוזרת או עמידה (רפרקטורית) מסוג Diffuse large B cell lymphoma, לאחר שני קווי טיפול ומעלה. במהלך מחלתו יהיה החולה זכאי לטיפול באחת מאלה – Axicabtagene ciloleucel, Tisagenlecleucel. 3. מבוגרים החולים בלימפומה פוליקולרית חוזרת או רפרקטורית לאחר שלושה קווי טיפול קודמים ומעלה. במהלך מחלתו יהיה החולה זכאי לטיפול באחת מאלה – Axicabtagene ciloleucel, Tisagenlecleucel. ב. מתן התרופה האמורה ייעשה לפי מרשם של מומחה בהמטולוגיה.
מסגרת הכללה בסל
התוויות הכלולות במסגרת הסל
| התוויה | תאריך הכללה | תחום קליני | Class Effect | מצב מחלה |
|---|---|---|---|---|
| מבוגרים החולים בלימפומה חוזרת או עמידה (רפרקטורית) מסוג Diffuse large B cell lymphoma, לאחר שני קווי טיפול ומעלה. במהלך מחלתו יהיה החולה זכאי לטיפול באחת מאלה – Axicabtagene ciloleucel, Tisagenlecleucel. | 16/01/2019 | המטולוגיה | DLBCL, Diffusa large B cell lymphoma | |
| ילדים ומבוגרים צעירים שמלאו להם 3 שנים וטרם מלאו להם 25 שנים החולים בלוקמיה חוזרת או עמידה (רפרקטורית) מסוג CD19+ B cell Acute Lymphoblastic Leukemia (ALL). לעניין זה מחלה חוזרת תוגדר בחולה שקיבל שני קווי טיפול קודמים או שעבר השתלה של תאי גזע המטופואטיים. | 16/01/2019 | המטולוגיה | ALL, Acute lymphoblastic leukemia | |
| מבוגרים החולים בלימפומה פוליקולרית חוזרת או רפרקטורית לאחר שלושה קווי טיפול קודמים ומעלה. במהלך מחלתו יהיה החולה זכאי לטיפול באחת מאלה – Axicabtagene ciloleucel, Tisagenlecleucel. | 01/02/2023 | המטולוגיה | לימפומה פוליקולרית, Follicular lymphoma | |
| ילדים ומבוגרים צעירים שמלאו להם 3 שנים וטרם מלאו להם 25 שנים החולים בלוקמיה חוזרת או עמידה (רפרקטורית) מסוג CD19+ B cell Acute Lymphoblastic Leukemia (ALL). לעניין זה מחלה חוזרת תוגדר בחולה שקיבל שני קווי טיפול קודמים או שעבר השתלה של תאי גזע המטופואטיים. במהלך מחלתו יהיה החולה זכאי לטיפול באחת מאלה – Brexucabtagene autoleucel, Tisagenlecleucel. | 01/02/2023 | המטולוגיה | ALL, Acute lymphoblastic leukemia |
שימוש לפי פנקס קופ''ח כללית 1994
לא צוין
תאריך הכללה מקורי בסל
16/01/2019
הגבלות
תרופה מוגבלת לרישום ע'י רופא מומחה או הגבלה אחרת
ATC
מידע נוסף
עלון מידע לצרכן
05.04.22 - עלון לצרכן אנגלית 05.04.22 - עלון לצרכן עברית 05.04.22 - עלון לצרכן ערבית 05.04.22 - עלון לצרכן 02.05.22 - עלון לצרכן אנגלית 05.04.22 - עלון לצרכן אנגלית 05.04.22 - עלון לצרכן עברית 05.04.22 - עלון לצרכן ערבית 05.04.22 - עלון לצרכן 05.04.22 - עלון לצרכן אנגלית 16.12.21 - עלון לצרכן אנגלית 07.08.22 - עלון לצרכן עברית 16.12.21 - עלון לצרכן ערבית 11.10.22 - עלון לצרכן אנגלית 11.10.22 - עלון לצרכן עברית 11.10.22 - עלון לצרכן ערבית 18.12.22 - עלון לצרכן אנגלית 18.12.22 - עלון לצרכן עברית 18.12.22 - עלון לצרכן ערבית 18.12.22 - עלון לצרכן 18.12.22 - עלון לצרכן אנגלית 18.12.22 - עלון לצרכן אנגלית 09.01.23 - עלון לצרכן עברית 28.02.23 - עלון לצרכן אנגלית 28.02.23 - עלון לצרכן עברית 28.02.23 - עלון לצרכן ערבית 04.08.23 - עלון לצרכן עברית 07.09.23 - עלון לצרכן אנגלית 07.09.23 - עלון לצרכן עברית 07.09.23 - עלון לצרכן ערבית 16.08.24 - עלון לצרכן עברית 12.09.24 - עלון לצרכן אנגלית 12.09.24 - עלון לצרכן ערבית 07.11.24 - עלון לצרכן עברית 10.02.20 - החמרה לעלון 09.06.21 - החמרה לעלון 22.11.21 - החמרה לעלון 07.08.22 - החמרה לעלון 05.09.22 - החמרה לעלון 09.01.23 - החמרה לעלון 04.08.23 - החמרה לעלון 28.12.23 - החמרה לעלון 19.08.24 - החמרה לעלוןלתרופה במאגר משרד הבריאות
קימריה