Quest for the right Drug
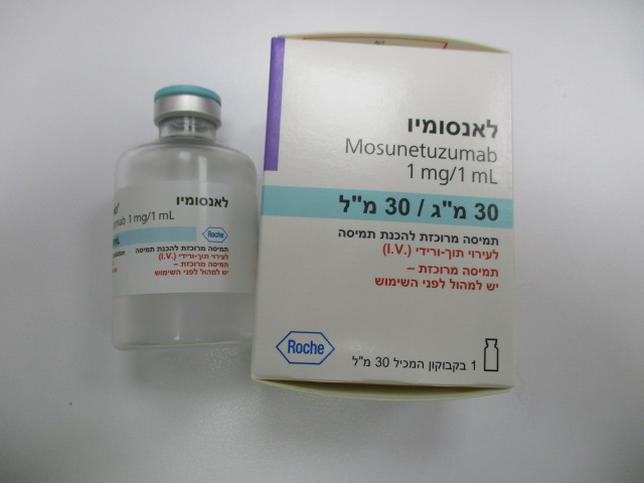
לאנסומיו LUNSUMIO (MOSUNETUZUMAB)
תרופה במרשם
תרופה בסל
נרקוטיקה
ציטוטוקסיקה
צורת מתן:
תוך-ורידי : I.V
צורת מינון:
תרכיז להכנת תמיסה לאינפוזיה : CONCENTRATE FOR SOLUTION FOR INFUSION
עלון לרופא
מינוניםPosology התוויות
Indications תופעות לוואי
Adverse reactions התוויות נגד
Contraindications אינטראקציות
Interactions מינון יתר
Overdose הריון/הנקה
Pregnancy & Lactation אוכלוסיות מיוחדות
Special populations תכונות פרמקולוגיות
Pharmacological properties מידע רוקחי
Pharmaceutical particulars אזהרת שימוש
Special Warning עלון לרופא
Physicians Leaflet
Adverse reactions : תופעות לוואי
4.8 Undesirable effects Summary of safety profile The adverse reactions (ARs) described in this section were identified from the pivotal clinical trial GO29781 in patients treated at the recommended dose (n=218). Patients had follicular lymphoma (41.3%), diffuse large B-cell lymphoma/transformed follicular lymphoma (40.4%) mantle cell lymphoma (11.5%), Richter’s transformation (6.4%), and other histologies (0.5%). The median number of cycles of Lunsumio received was 8 (range 1 -17), 37% of patients received 8 cycles, and 15% received more than 8 cycles up to 17 cycles. The most common adverse reactions (≥ 20%) observed were cytokine release syndrome, neutropenia, pyrexia, hypophosphatemia and headache. The most common serious adverse reactions (≥ 2%) observed included cytokine release syndrome (CRS) (21% by ASTCT grading system), pyrexia (5%), and pneumonia (3%). Nine of 218 patients (4.1%) discontinued Lunsumio due to an adverse event. CRS was the only adverse reaction that led to discontinuation in more than one patient (2 patients [0.9%]). Tabulated list of adverse reactions The adverse reactions are listed below by MedDRA system organ class (SOC) and categories of frequency. Frequency categories are defined as very common (≥ 1/10), common (≥ 1/100 to < 1/10), uncommon (≥ 1/1,000 to < 1/100), rare (≥ 1/10,000 to < 1/1,000), very rare (< 1/10,000) and not known (cannot be estimated from the available data). Within each frequency grouping, adverse reactions are presented in order of decreasing seriousness. Table 4 Adverse reactions occurring in patients treated with Lunsumio System organ class / preferred term or All grades Grade 3 – 4 adverse reaction Infections and infestations Upper respiratory tract infection Common Common Urinary tract infection Common Common Pneumonia Common Common Neoplasms benign, malignant and unspecified (including cysts and polyps) Tumour flare Common Common Blood and lymphatic system disorders Neutropenia1 Very common Very common Anaemia Very common Common Thrombocytopenia2 Very common Common Febrile neutropenia Common Common Haemophagocytic lymphohistiocytosis5 Uncommon Uncommon System organ class / preferred term or All grades Grade 3 – 4 adverse reaction Immune system disorders Cytokine release syndrome3 Very common Common Metabolism and nutrition disorders Hypophosphataemia Very common Very common Hypokalaemia Very common Common Hypomagnesaemia Very common Very rare Tumour lysis syndrome Uncommon Uncommon Nervous system disorders Headache Very common Uncommon Immune effector cell-associated Common Very rare neurotoxicity syndrome4,5 Gastrointestinal disorders Diarrhoea Very common Very rare Skin and subcutaneous tissue disorders Rash Very common Uncommon Pruritus Very common Very rare Dry skin Very common Very rare General disorders and administration site conditions Pyrexia Very common Common Chills Very common Uncommon Investigations Alanine aminotransferase, increased Very common Common Aspartate aminotransferase, increased Common Common 1 Neutropenia includes neutropenia and neutrophil count decreased 2 Thrombocytopenia includes thrombocytopenia and platelet count decreased 3 By American Society for Transplant and Cellular Therapy 4 Consistent with the medical concept of ICANS according to American Society for Transplant and Cellular Therapy and includes confusional state, ICANS, lethargy, encephalopathy, depressed level of consciousness, and memory impairment 5 The frequency calculation is based on additional clinical studies Description of selected adverse reactions Cytokine release syndrome (CRS) CRS (ASTCT grading system) of any grade occurred in 39% (86/218) of patients, with grade 2 occurring in 14%, grade 3 occurring in 2.3%, and grade 4 occurring in 0.5% of patients treated with Lunsumio. The one patient with the grade 4 event was a patient with FL in the leukemic phase who also experienced concurrent TLS. CRS of any grade occurred in 15% of patients after the Cycle 1, Day 1 dose; 5% after the Cycle 1, Day 8 dose; 33% after the Cycle 1, Day 15 dose, 5% occurred in patients after the Cycle 2 and 1% in Cycles 3 and beyond. The median time to CRS onset from the start of administration in Cycle 1 Day 1 was 5 hours (range: 1-73 hours), Cycle 1 Day 8 was 28 hours (range: 5-81 hours), Cycle 1 Day 15 was 25 hours (range: 0.1-391 hours), and Cycle 2 Day 1 was 46 hours (range: 12-82 hours). CRS resolved in all patients, and the median duration of CRS events was 3 days (range 1-29 days). Of the 86 patients that experienced CRS, the most common signs and symptoms of CRS included pyrexia (98%), chills (36%), hypotension (35%), tachycardia (24%), hypoxia (22%) and headache (16%). Tocilizumab and/or corticosteroids were used to manage a CRS event in 16% of patients: 6% received tocilizumab alone, 6% received corticosteroids alone, and 4% received both tocilizumab and corticosteroids. Among the 10% of patients who received tocilizumab (with or without a corticosteroid), 86% received only one dose of tocilizumab, with no more than two doses of tocilizumab administered for a single CRS event. In patients experiencing Grade 2 CRS, 48% of patients were treated with symptomatic management without corticosteroids or tocilizumab, 18% received tocilizumab alone, 21% received corticosteroids alone, and 12% received both corticosteroids and tocilizumab. Patients with grade 3 or grade 4 CRS received tocilizumab, corticosteroids, vasopressors and/or oxygen supplementation. Three percent of patients experienced hypotension and/or hypoxia without fever following Lunsumio administration; 2% of patients received tocilizumab and/or corticosteroids in the absence of fever. Hospitalizations due to CRS occurred in 21% of patients and the median duration of hospitalization was 5 days (range 0-30 days). Neutropenia Neutropenia of any grade occurred in 28% of patients, including 24% Grade 3-4 events. The median time to onset of first neutropenia/neutrophil count decreased events was 48 days (range: 1-280 days), with median duration of 8 days (range: 1-314 days). Of the 60 patients who had neutropenia/neutrophil count decreased events 68% received treatment G-CSF to treat the events. Serious infections Serious infections of any grade occurred in 17% of patients. 1.8% of patients experienced serious infections concurrently with grade 3-4 neutropenia. The median time to onset of first serious infection was 50 days (range: 1-561 days), with median duration of 12 days (range: 2-174 days). Grade 5 events occurred in 0.9% of patients, which included pneumonia and sepsis. Immune Effector Cell-Associated Neurotoxicity Syndrome Immune Effector Cell-Associated Neurotoxicity Syndrome (ICANS) occurred in 2.1% (20/949) of patients, 19 patients had Grade 1-2 events and 1 patient had Grade 3 event. The majority of events occurred during the first cycle of treatment. The majority of cases resolved. The median time to onset from initial dose was 17 days (range: 1 to 48 days). The median duration was 3 days (range: 1-20 days). Tumour flare Tumour flare (including pleural effusion and tumour inflammation) occurred in 4% of patients, which included 1.8% grade 2 and 2.3% grade 3 events. The median time to onset was 13 days (range 5-84 days), and median duration was 10 days (range 1-77 days). Tumour Lysis Syndrome (TLS) TLS occurred in 0.9% of patients, concurrent with CRS. One patient with follicular lymphoma was in the leukemic phase who experienced Grade 4 TLS. TLS onset was on days 2 and 24, and resolved within 4 and 6 days, respectively. Reporting of suspected adverse reactions Reporting suspected adverse reactions after authorization of the medicinal product is important. It allows continued monitoring of the benefit/risk balance of the medicinal product. Any suspected adverse events should be reported to the Ministry of Health according to the National Regulation by using an online form sideeffects.health.gov.il/

שימוש לפי פנקס קופ''ח כללית 1994
לא צוין
תאריך הכללה מקורי בסל
לא צוין
הגבלות
לא צוין
יצרן
GENENTECH INC., USAבעל רישום
ROCHE PHARMACEUTICALS (ISRAEL) LTDרישום
172 15 37418 00
מחיר
0 ₪
מידע נוסף
