Quest for the right Drug
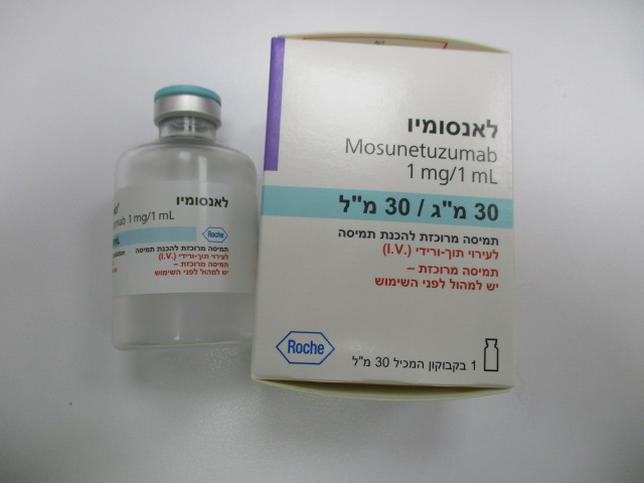
לאנסומיו LUNSUMIO (MOSUNETUZUMAB)
תרופה במרשם
תרופה בסל
נרקוטיקה
ציטוטוקסיקה
צורת מתן:
תוך-ורידי : I.V
צורת מינון:
תרכיז להכנת תמיסה לאינפוזיה : CONCENTRATE FOR SOLUTION FOR INFUSION
עלון לרופא
מינוניםPosology התוויות
Indications תופעות לוואי
Adverse reactions התוויות נגד
Contraindications אינטראקציות
Interactions מינון יתר
Overdose הריון/הנקה
Pregnancy & Lactation אוכלוסיות מיוחדות
Special populations תכונות פרמקולוגיות
Pharmacological properties מידע רוקחי
Pharmaceutical particulars אזהרת שימוש
Special Warning עלון לרופא
Physicians Leaflet
Pharmacological properties : תכונות פרמקולוגיות
Pharmacodynamic Properties
5.1 Pharmacodynamic properties Pharmacotherapeutic group: Antineoplastic agents; other antineoplastic agents; monoclonal antibodies, ATC code: L01FX25 Mechanism of action Mosunetuzumab is an anti-CD20/CD3 T-cell engaging bispecific antibody targeting CD20-expressing B-cells. It is a conditional agonist; targeted B-cell killing is observed only upon simultaneous binding to CD20 on B-cells and CD3 on T-cells. Engagement of both arms of mosunetuzumab results in the formation of an immunologic synapse between a target B cell and a cytotoxic T cell leading to T-cell activation. Subsequent directed release of perforin and granzymes from T-cell activation through the immunologic synapsis induce B-cell lysis leading to cell death. Lunsumio caused B-cell depletion (defined as CD19 B-cell counts < 0.07 x 109/L) and hypogammaglobulinemia (defined as IgG levels < 500 mg/dL). Clinical efficacy and safety Relapsed or refractory B-cell Non-Hodgkin's lymphoma An open-label, multicentre, multi-cohort study (GO29781) was conducted to evaluate Lunsumio in patients with relapsed or refractory B-cell non-Hodgkin's lymphoma for whom there was no available therapy expected to improve survival. In the follicular lymphoma (FL) cohort (n=90), patients with relapsed or refractory FL (Grade 1-3A) were required to have received at least two prior systemic therapies, including an anti-CD20 monoclonal antibody and an alkylating agent. Patients with FL Grade 3b and patients with transformed FL at study entry were not eligible; those with a history of transformed FL but FL Grade 1-3A at study entry were included in the FL cohort. The study excluded patients with Eastern Cooperative Oncology Group (ECOG) performance status ≥ 2, significant cardiovascular disease (such as New York Heart Association Class III or IV cardiac disease, myocardial infarction within the last 6 months, unstable arrhythmias, or unstable angina), significant active pulmonary disease, impaired renal functions (Creatinine clearance [CrCl] < 60 mL/min with elevated serum creatinine level), active autoimmune disease requiring immunosuppressive therapy, active infections (i.e., chronic active EBV, acute or chronic hepatitis C, hepatitis B, HIV), progressive multifocal leukoencephalopathy, current or a history of CNS lymphoma or CNS disease, a history of macrophage activation syndrome / hemophagocytic lymphohistiocytosis, prior allogeneic stem cell transplant, or prior organ transplantation. Patients received Lunsumio intravenously in a 21-day Cycle as follows: • Cycle 1 Day 1: 1 mg • Cycle 1 Day 8: 2 mg • Cycle 1 Day 15: 60 mg • Cycle 2 Day 1: 60 mg • Cycle 3 and beyond Day 1: 30 mg The median number of cycles was 8, 59% received 8 cycles, and 18% received more than 8 cycles up to 17 cycles. The median age was 60 years (range 29 to 90 years) with 31% being > age 65, and 7.8% being ≥ age 75. Sixty-one percent were male, 82% were white, 9% were Asian, 4% were Black, 100% had an ECOG performance status of 0 or 1 and 34% of patients had bulky disease (at least one lesion > 6 cm). The median number of prior therapies was 3 (range: 2-10), with 38% receiving 2 prior therapies, 31% receiving 3 prior therapies and 31% receiving more than 3 prior therapies. All patients received prior anti-CD20 and alkylator therapies, 21% received autologous stem cell transplant, 19% received PI3K inhibitors, 9% received prior rituximab plus lenalidomide therapy, and 3% received CAR-T therapies. Seventy-nine percent of patients were refractory to prior anti-CD20 monoclonal antibody therapy and 53% were refractory to both anti-CD20 monoclonal antibody and alkylator therapy. Sixty-nine percent of patients were refractory to the last prior therapy and 52% had progression of disease within 24 months of first systemic therapy. The primary efficacy endpoint was complete response (CR) as assessed by an independent review facility (IRF) according to standard criteria for NHL (Cheson 2007). The efficacy results are summarised in Table 5. Table 5 Summary of efficacy in patients with relapsed/refractory FL Efficacy parameter Lunsumio N=90 Median observation time 18.3 months (range 2 – 27 months) Complete Response (CR), n (%), 54 (60.0) (95% CI) (49.1, 70.2) Objective Response Rate (ORR), n (%) 72 (80.0) (95% CI) (70.3, 87.7) Partial Response (PR) n (%) 18 (20.0) (95% CI) (12.3, 29.8) 1 Duration of Response (DOR) Patients with event, n (%) 29 (40.3) Median, months (95% CI) 22.8 (9.7, NR) K-M event-free proportion 12 months 61.8 (95% CI) (50.0, 73.7) 18 months 56.9 (95% CI) (44.1, 69.6) Duration of Complete Response (DOCR)2 Patients with event, n (%) 16 (29.6) Median, months (95% CI) NR (14.6, NR) K-M event-free proportion, 12 months 71.4 (95% CI) (57.9, 84.9) 18 months 63.7 (95% CI) (48.0, 79.4) CI=confidence interval; K-M=Kaplan-Meier; NR=not reached. Clinical Cut-off: 27 August 2021 Hypothesis testing was conducted on the primary endpoint of IRF assessed CR rate. 1 DOR is defined as the time from the initial occurrence of a documented PR or CR until the patient experiences an event (documented disease progression or death due to any cause, whichever occurs first). 2 DOCR is defined as the time from the initial occurrence of a documented CR until the patient experiences an event (documented disease progression or death due to any cause, whichever occurs first). The median follow-up for DOR was 14.9 months. Additional exploratory efficacy outcomes included the median time to first response (1.4 months, range: 1.1 - 8.9) and the median time to first complete response (3.0 months, range: 1.1- 18.9). Immunogenicity The immunogenicity of mosunetuzumab was evaluated using an enzyme-linked immunosorbent assay (ELISA). No patients tested positive for anti-mosunetuzumab antibodies in 418 ADA-evaluable patients who received Lunsumio single-agent intravenous treatments in Study GO27981. Based on the available information, the clinical relevance of anti-mosunetuzumab antibodies could not be assessed.
Pharmacokinetic Properties
5.2 Pharmacokinetic properties Mosunetuzumab pharmacokinetic (PK) exposure increased in an approximately dose-proportional manner over the dose range studied, from 0.05 to 60 mg. The population pharmacokinetic following intravenous administrations of Lunsumio was described by a 2-compartment PK model with time- dependent clearance, which was parameterized as descending to a steady-state plateau (CLss) from a baseline value (CLbase) at the start of treatment according to transitional half-life of 16.3 days. Moderate to high pharmacokinetic variability for mosunetuzumab was observed and characterized by inter-individual variability (IIV) ranging from 18% to 86% coefficient of variation (CV) for mosunetuzumab PK parameters: IIV was estimated for CLbase (63% CV), central volume of distribution (31% CV), peripheral volume of distribution (25% CV), CLss (18% CV), and transitional half-life (86% CV). After the first two Cycles (i.e., 42 days) of the dosing with Lunsumio, the serum concentration reaches the Cmax at the end of dose of Cycle 2 Day 1 of the Lunsumio intravenous infusion with an average maximal concentration of 17.9 µg/mL and %CV of 49.6%. The average total two cycles (42 days) mosunetuzumab exposure AUC was 126 day•g/mL with %CV of 44.4%. Absorption Lunsumio is administered intravenously. Distribution The population estimate of central volume of distribution for mosunetuzumab was 5.49 L with intravenous infusion of Lunsumio. Because mosunetuzumab is an antibody, protein binding studies were not conducted. Biotransformation The metabolic pathway of mosunetuzumab has not been directly studied. Like other protein therapeutics, mosunetuzumab is expected to be degraded into small peptides and amino acids via catabolic pathways. Elimination Based on a population pharmacokinetic analysis, the estimated mean CLss and baseline clearance (CLbase) were 1.08 L/day and 0.584 L/day, respectively. The terminal half-life estimate was 16.1 days at steady state based on population pharmacokinetic model estimates. The results obtained in study GO29781 indicate that mosunetuzumab serum concentration reaches the Cmax at the end of the intravenous infusion and declines in a bi-exponential fashion. Special populations Elderly Age did not have an effect on the pharmacokinetics of mosunetuzumab based on a population pharmacokinetic analysis with patients aged 19-96 years (n=439). No clinically important difference was observed in the pharmacokinetics of mosunetuzumab for patients in this age group. Bodyweight Like other therapeutic proteins, bodyweight was positively associated with mosunetuzumab estimated clearance and volume of distribution. However, based on exposure-response analysis and clinical exposure margins, considering the exposures in patients at either “low” (<50 kg) or “high” (≥112 kg) weight, no dose adjustment is required due to patient bodyweight. Gender Based upon population pharmacokinetic analysis, steady-state clearance of mosunetuzumab is marginally lower in females (~13%) compared to males. No dose adjustment is required due to gender, based on exposure-response analysis. Race Race (Asian vs. non-Asian) was not identified as a covariate influencing mosunetuzumab pharmacokinetics. Renal impairment No dedicated studies have been conducted to determine the effect of renal impairment on the pharmacokinetics of mosunetuzumab. The renal elimination of intact mosunetuzumab, an IgG monoclonal antibody, is expected to be low and of minor importance. The population PK analysis of mosunetuzumab showed that creatinine clearance (CrCl) does not affect pharmacokinetics of mosunetuzumab. Pharmacokinetics of mosunetuzumab in patients with mild (CrCl 60 to 89 mL/min, n=178) or moderate (CrCl 30 to 59 mL/min, n=53) renal impairment were similar to those in patients with normal renal function (CrCl ≥ 90 mL/min, n=200). Pharmacokinetic data in patients with severe renal impairment (CrCl 15 to 29 mL/min) is limited (n=1), therefore no dose recommendations can be made. Lunsumio was not studied in patients with end-stage renal disease and/or who are on dialysis. Hepatic impairment No specific studies have been conducted to determine the effect of hepatic impairment on the pharmacokinetics of mosunetuzumab. IgGs are mainly eliminated via intracellular catabolism and hepatic impairment is not expected to influence clearance of mosunetuzumab. The population PK analysis of mosunetuzumab showed that hepatic impairment does not affect pharmacokinetics of mosunetuzumab. Pharmacokinetics of mosunetuzumab in patients with mild hepatic impairment (total bilirubin > ULN to 1.5 x ULN or AST > ULN, n=53) were similar to those in patients with normal hepatic function (n=384). The number of patients with moderate hepatic impairment is limited (total bilirubin > 1.5–3 x ULN, any AST, n=2) and no patients with severe hepatic impairment have been studied. Paediatric population No studies have been conducted to investigate the pharmacokinetics of mosunetuzumab in the paediatric population (< 18 years old).

שימוש לפי פנקס קופ''ח כללית 1994
לא צוין
תאריך הכללה מקורי בסל
לא צוין
הגבלות
לא צוין
יצרן
GENENTECH INC., USAבעל רישום
ROCHE PHARMACEUTICALS (ISRAEL) LTDרישום
172 15 37418 00
מחיר
0 ₪
מידע נוסף
