Quest for the right Drug
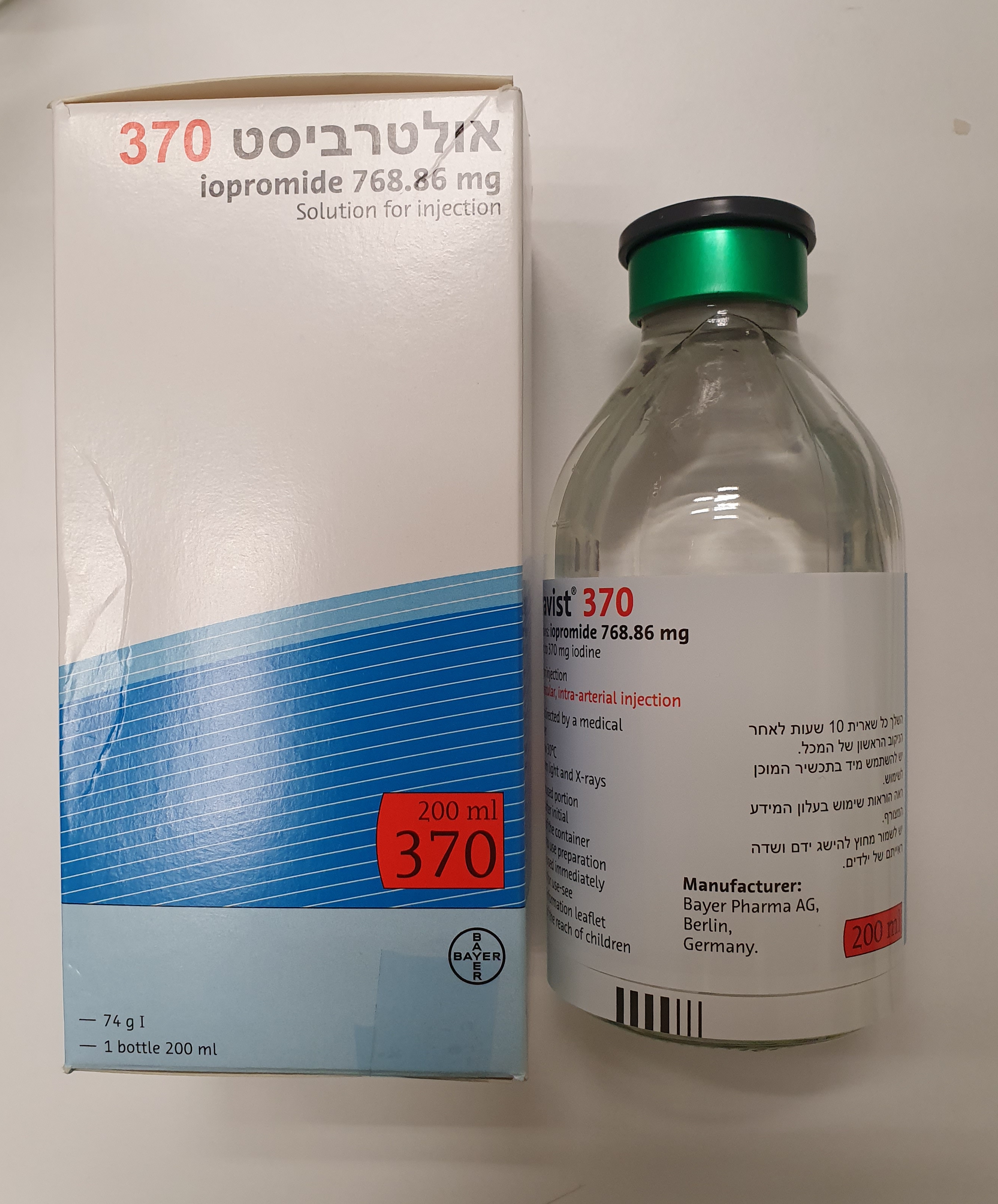
אולטרביסט 370 ULTRAVIST 370 (IOPROMIDE)
תרופה במרשם
תרופה בסל
נרקוטיקה
ציטוטוקסיקה
צורת מתן:
תוך-ורידי, תוך-עורקי : I.V, INTRA-ARTERIAL
צורת מינון:
תמיסה להזרקה : SOLUTION FOR INJECTION
עלון לרופא
מינוניםPosology התוויות
Indications תופעות לוואי
Adverse reactions התוויות נגד
Contraindications אינטראקציות
Interactions מינון יתר
Overdose הריון/הנקה
Pregnancy & Lactation אוכלוסיות מיוחדות
Special populations תכונות פרמקולוגיות
Pharmacological properties מידע רוקחי
Pharmaceutical particulars אזהרת שימוש
Special Warning עלון לרופא
Physicians Leaflet
Special Warning : אזהרת שימוש
4.4 Special warnings and precautions for use 4.4.1 For all indications 4.4.1.1 Hypersensitivity reactions Ultravist may be associated with anaphylactoid/hypersensitivity reactions or other idiosyncratic reactions characterised by cardiovascular, respiratory and cutaneous events. Allergic-type undesirable effects are possible, ranging from mild to severe reactions including shock (see section “Undesirable effects”). Most of these undesirable effects occur within 30 minutes of administration. However, delayed reactions (after several hours or even several days) may also occur. The risk of hypersensitivity reactions is higher in the following cases: - if the patient has had a previous reaction to a contrast medium - if the patient has a history of bronchial asthma or other allergic disorders. Due to an increased risk of hypersensitivity reactions (including serious reactions), a particularly careful risk/benefit assessment is necessary in patients with known hypersensitivity to Ultravist or to any of the excipients of Ultravist, and in patients who have experienced a previous hypersensitivity reaction to another iodinated contrast medium. However, these undesirable effects are sporadic and unpredictable. Patients who experience such reactions while taking beta blockers may not respond to beta agonist treatment (see also section “Interaction with other medicinal products and other forms of interaction”). In the event of a severe hypersensitivity reaction, patients with cardiovascular disease are more susceptible to serious or even fatal complications. Due to the possibility of severe hypersensitivity reactions after administration, the patient should continue to be monitored after the procedure. For all patients, healthcare professionals must be ready to institute emergency measures. Premedication with corticosteroids may be considered in patients with an increased risk of allergic- type reactions and patients who have previously developed a moderate or severe acute reaction, asthma or allergy requiring medical treatment. 4.4.1.2 Severe skin reactions Severe skin reactions, particularly cases of Stevens‑Johnson syndrome (SJS), toxic epidermal necrolysis (TEN), drug reaction with eosinophilia and systemic symptoms (DRESS syndrome) and acute generalised exanthematous pustulosis (AGEP) that may be life‑threatening or fatal have been associated with iopromide administration at a frequency that is not known. Patients must be informed of the associated signs and symptoms and close monitoring for the onset of skin reactions is required. In children, the skin rash observed initially may be misinterpreted as an infection, and physicians should consider the possibility of a reaction to iopromide in children who develop signs of skin rash and fever. In most cases, these reactions occurred within 8 weeks (1 to 12 days for AGEP, 2 to 8 weeks for DRESS syndrome, and 5 days to 8 weeks for SJS/TEN). If the patient develops a serious reaction such as SJS, TEN, AGEP or DRESS syndrome during iopromide use, iopromide must never be readministered. 4.4.1.3 Thyroid dysfunction In patients with known or suspected hypothyroidism or goitre, a very careful risk/benefit assessment is necessary because the iodinated contrast medium may cause hyperthyroidism and a thyrotoxic crisis in these patients. In patients with known or suspected hyperthyroidism, testing of thyroid function and/or a prophylactic thyrostatic medicinal product should be considered before Ultravist administration. Thyroid function tests indicating hypothyroidism or a transient decrease in thyroid function have been reported following administration of iodinated contrast media in adult and paediatric patients. The potential risk of hypothyroidism must be evaluated in patients with known or suspected thyroid disease prior to the use of iodinated contrast media. Thyroid Dysfunction in Pediatric Patients 0 to 3 Years of Age: Thyroid dysfunction characterized by hypothyroidism or transient thyroid suppression has been reported after both single exposure and multiple exposures to iodinated contrast media (ICM) in pediatric patients 0 to 3 years of age. The incidence has been reported between 1% and 15% depending on the age of the subjects and the dose of the iodinated contrast agent and is more commonly observed in neonates and premature infants. Neonates may also be exposed through the mother during pregnancy. Younger age, very low birth weight, prematurity, underlying medical conditions affecting thyroid function, admission to neonatal or pediatric intensive care units, and congenital cardiac conditions are associated with an increased risk of hypothyroidism after ICM exposure. Pediatric patients with congenital cardiac conditions may be at the greatest risk given that they often require high doses of contrast during invasive cardiac procedures. An underactive thyroid during early life may be harmful for cognitive and neurological development and may require thyroid hormone replacement therapy. After exposure to ICM, individualize thyroid function monitoring based on underlying risk factors, especially in term and preterm neonates. 4.4.1.4 CNS disorders Patients with CNS disorders may be at an increased risk of neurological complications following Ultravist administration. Neurological complications are more common in the context of cerebral angiography and related procedures. Cases of encephalopathy have been reported following the use of iopromide (see section 4.8). Contrast media-induced encephalopathy may manifest as signs and symptoms of neurological dysfunction, such as headache, vision disorders, cortical blindness, confusion, seizures, loss of coordination, hemiparesis, aphasia, loss of consciousness, coma, and cerebral oedema. Symptoms generally appear within a few minutes or hours of iopromide administration and generally resolve within a few days. Caution should be exercised in situations in which there may be a reduced seizure threshold, as in patients with a history of epileptic episodes and in the concomitant use of specific medicinal products. Factors which increase blood-brain barrier permeability promote the passage of the contrast medium into cerebral tissue, which may induce CNS reactions such as encephalopathy. If contrast media-induced encephalopathy is suspected, appropriate medical care must be given and iopromide must never be readministered to this patient. 4.4.1.5 Hydration Good hydration must be ensured in all patients before intravascular Ultravist administration (see also section “Intravascular use” – “Acute kidney injury”). This applies especially to patients presenting renal impairment risk factors, such as patients with multiple myeloma, diabetes, polyuria, oliguria or hyperuricaemia, and to newborns, babies, toddlers, young children and elderly patients. Adequate hydration must be ensured in patients presenting renal impairment. However, the prophylactic administration of intravenous fluid in patients with moderate renal impairment (eGFR 30-59 mL/min./1.73 m2) is not recommended as no additional benefit in terms of renal safety has been demonstrated. In patients with severe renal impairment (eGFR < 30 mL/min./1.73 m2) and cardiac comorbidity, the prophylactic administration of intravenous fluid can lead to an increase in serious cardiac complications. See sections 4.4.2.1 Acute kidney injury, 4.4.2.2 Cardiovascular disorders and 4.8.2 Summary table of undesirable effects. If prophylactic intravenous fluids are administered, monitoring of cardiac function parameters is recommended. 4.4.1.6 Anxiety Pronounced states of agitation, anxiety and pain may increase the risk of undesirable effects or intensify contrast medium-related reactions. In these patients, measures should be taken to relieve the anxiety. 4.4.1.7 Pretesting Sensitivity testing using a small test dose of contrast medium is not recommended as it has no predictive value. Furthermore, sensitivity testing itself may lead to serious or even fatal hypersensitivity reactions. 4.4.2 Intravascular use 4.4.2.1 Acute kidney injury Post-contrast acute kidney injury (PC-AKI) can occur after intravascular administration of Ultravist, manifesting in the form of temporary renal impairment. Acute kidney injury may also occur in a few cases. The main risk factors are: - pre-existing renal impairment (see section 4.2 Patients with renal impairment) - dehydration (see section 4.4.1.5 Hydration) - diabetes - multiple myeloma/paraproteinaemia, - repeated and/or high doses of Ultravist. Patients with moderate to severe renal impairment (eGFR 44-30 mL/min./1.73 m2) or severe renal impairment (eGFR < 30 mL/min./1.73 m2) are at increased risk of post-contrast acute kidney injury (PC-AKI) during arterial administration of contrast media with first-pass renal exposure. Patients with severe renal impairment (eGFR < 30 mL/min./1.73 m2) are at increased risk of PC-AKI when administration is intravenous or intraarterial with second-pass renal exposure (see section 4.4.1.5 Hydration). Patients on dialysis and without residual renal function may receive Ultravist for radiological examinations because the iodinated contrast medium is cleared by dialysis. 4.4.2.2 Cardiovascular disease Patients with significant cardiac disease or severe coronary artery disease are at an increased risk of developing clinically relevant haemodynamic changes and arrhythmias. Intravascular injection of Ultravist may cause pulmonary oedema in patients with heart failure. 4.4.2.3 Phaeochromocytoma Patients with phaeochromocytoma may be at an increased risk of developing a hypertensive crisis. 4.4.2.4 Myasthenia gravis The administration of Ultravist may aggravate the symptoms of myasthenia gravis. 4.4.2.5 Thromboembolic events A property of non-ionic contrast media is their low interference with normal physiological functions. As a result of this, non-ionic contrast media have lower anticoagulant activity in vitro than ionic media. Numerous other factors not related to the contrast medium, particularly the length of examination, number of injections, catheter and syringe materials, underlying disease and concomitant medicinal products, may contribute to the development of thromboembolic events. This should therefore be borne in mind when performing vascular catheterisation procedures, and particular attention should be paid to the angiographic technique, with frequent flushing of the catheter with physiological saline (if possible with the addition of heparin) and minimisation of the length of the procedure so as to limit the risk of procedure-related thrombosis and embolism. 4.4.3 Contrast-enhanced mammography (CEM) Contrast-enhanced mammography increases patient exposure to ionising radiation compared with standard mammography. The radiation dose depends on breast thickness, the type of mammography machine and on the system settings of the machine. The total radiation dose for CEM remains lower than the threshold value defined in the international guidelines for mammography (below 3 mGy). 4.4.4 Information on excipients This medicinal product contains less than 1 mmol (23 mg) sodium per 1 mL, i.e. it is essentially “sodium-free”.
Effects on Driving
4.7 Effects on ability to drive and use machines No data available. However, because of the risk of reactions, driving or operating machinery is not advisable for 30 minutes after the last injection (see Section 4.4).

שימוש לפי פנקס קופ''ח כללית 1994
לא צוין
תאריך הכללה מקורי בסל
לא צוין
הגבלות
לא צוין
מידע נוסף
