Quest for the right Drug
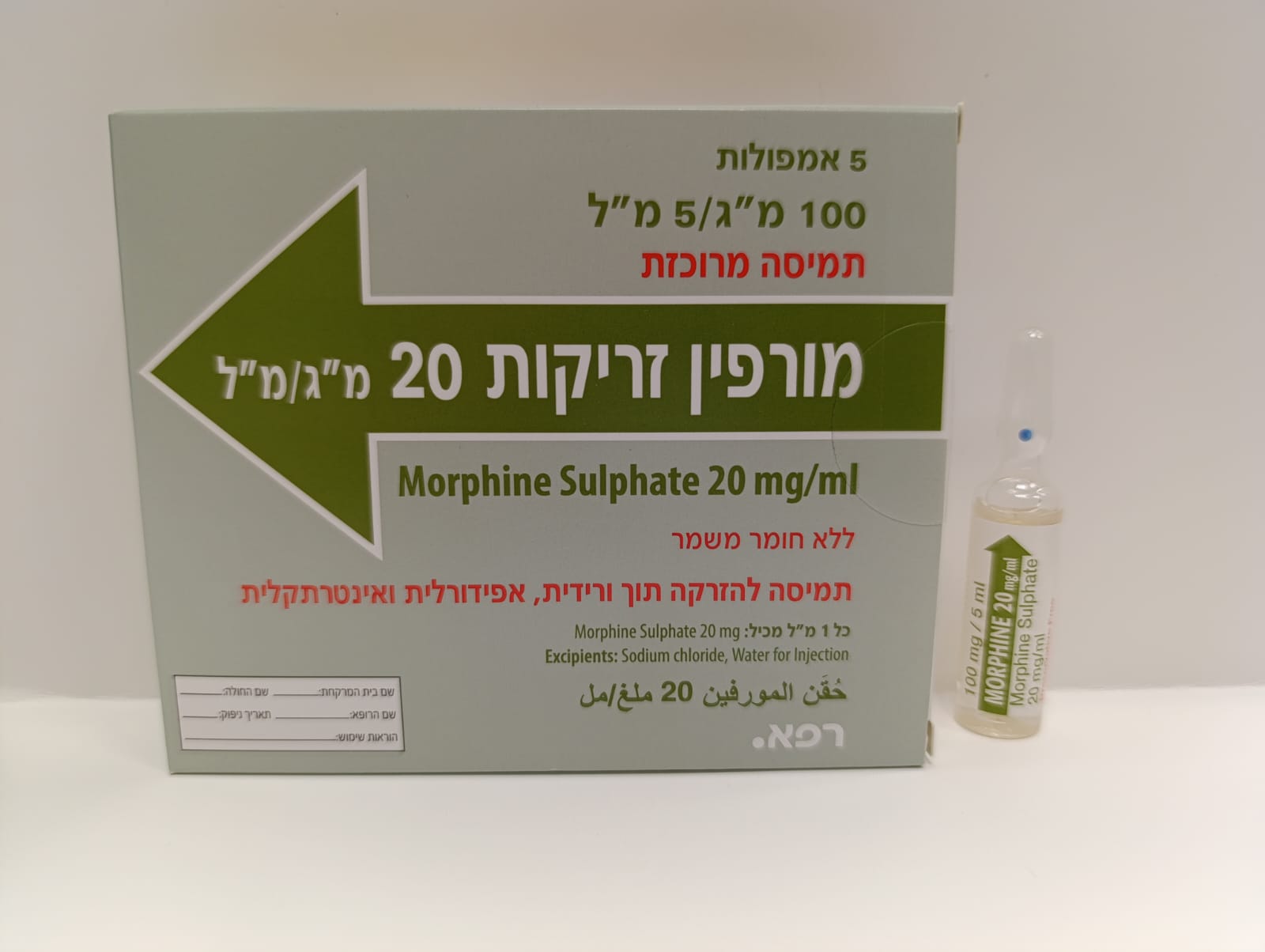
מורפין זריקות 20 מ"ג/מ"ל MORPHINE INJECTIONS 20 MG/ML (MORPHINE SULFATE)
תרופה במרשם
תרופה בסל
נרקוטיקה
ציטוטוקסיקה
צורת מתן:
תוך-שדרתי, תוך-ורידי, אפידורל : INTRATHECAL, I.V, EPIDURAL
צורת מינון:
תמיסה להזרקה : SOLUTION FOR INJECTION
עלון לרופא
מינוניםPosology התוויות
Indications תופעות לוואי
Adverse reactions התוויות נגד
Contraindications אינטראקציות
Interactions מינון יתר
Overdose הריון/הנקה
Pregnancy & Lactation אוכלוסיות מיוחדות
Special populations תכונות פרמקולוגיות
Pharmacological properties מידע רוקחי
Pharmaceutical particulars אזהרת שימוש
Special Warning עלון לרופא
Physicians Leaflet
Posology : מינונים
4.2 POSOLOGY AND METHOD OF ADMINISTRATION Morphine sulphate preservative-free injection is intended for IV, epidural or intrathecal administration. Posology General Dosing Information for Neuraxial (epidural, intathecal) Administration Epidural or intrathecal administration of opioid analgesics should be performed only by physicians experienced in these techniques. Solutions containing a preservative must not be injected via these routes. Upon initiation of continuous intraspinal therapy and following any subsequent dosage increments that are substantial, patients should be monitored in an adequate setting for at least 24 hours. Such facilities should have available resuscitative equipment and medications, including oxygen and a specific antagonist (naloxone HCI injection), for the management of respiratory depression or other complications that may arise [see Warnings and Precautions (4.4)]. For epidural or intrathecal administration, injection into the lumbar area may be preferred because of the increased risk of respiratory depression with injection into the thoracic area. Also, the epidural route is preferred, whenever possible, because of the increased risk of respiratory depression with intrathecal administration [see Warnings and Precautions (4.4)]. Prior to the initial epidural administration, proper placement of the needle or catheter in the epidural space must be verified. Aspiration to check for blood or cerebrospinal fluid may be performed; however, the fact that intravascular administration is possible even when aspiration for blood is negative must be kept in mind. Alternatively, administration of 5 ml (3ml for obstetrical patients) of preservative-free 1.5% lidocaine hydrochloride with epinephrine 1:200,000 injection may be used to verify placement in the epidural space. Tachycardia occurring after injection of the test medication indicates that the medication has entered the circulation; sudden onset of segmental anesthesia indicates that the medication has been administered intrathecally. Following epidural or intrathecal injection of an opioid analgesic, administration of low doses of naloxone via continuous IV infusion for 24 hours may decrease the incidence of potential side effects without interfering with the analgesic effectiveness of the medication. The desired amount of morphine should be withdrawn from the ampoule through a microfilter. To minimize risk from glass or other particles, the product must be filtered through a 5 micro (or smaller) microfilter before injecting into the microinfusion device. If dilution is required, 0.9% sodium chloride injection is recommended. Dosage and administration Specific Dosing Regimens For the correct and effective use of morphine it is critical to adjust the dosing regimen for each patient individually according to the severity of pain, the patient’s metabolism and condition, previous history of analgesic therapy, concomitant medications, and response to morphine, The following dosage recommendations are, therefore, only suggested approaches to what is actually a series of clinical decisions in the management of pain of an individual patient. Dosage for Continuous IV Administration For patients with severe chronic pain in whom the oral route is not feasible (e.g., bowel obstruction), parenteral opioids are needed. Since intermittent injections are expensive, uncomfortable, induce “clock watching” and are associated with the “bolus effect” (peak levels associated with intolerable adverse effects and trough levels associated with inadequate analgesia), a continuous IV infusion is preferable. Continuous IV infusions (CIVI) are especially suitable for patients who already require IV access and maintenance for other reasons. Opioid therapy with CIVI should usually be attempted prior to initiating intraspinal therapy since this route of administration is less invasive, less expensive and is associated with a lower risk of serious complications. For patients transferring from oral opioids, standard equianalgesic tables should be consulted for calculating the total daily opioid dose in parenteral morphine equivalents. For CIVI, the daily parenteral morphine dose should be added to solution (e.g., 500ml saline) and delivered over the ensuing 24 hours (e.g., 20ml/ hour). A loading bolus of 15 mg may be given by slow IV injection at the start of the infusion. Arrangements for rescue medication for breakthrough pain should always be ensured. It is important to remember that all conversion tables/ratios are meant to serve only as a guide and the dosage must always be adjusted according to the patient’s response. Following assessment, the initial dose should be titrated up or down accordingly, until analgesia is adequate and side effects minimal. Following initiation of the infusion and after any subsequent changes in the infusion rate that are substantial, the patient should be monitored closely for several hours in a setting where an opioid antagonist, oxygen and resuscitative equipment, and personnel trained in their use, are available. During the course of treatment, the patient may experience a recurrence of pain due to an increase in the level of pain because of disease progression or the development of tolerance to the drug. If this occurs, an increase in the dosage may be required. As there is no upper limit to the amount of morphine that may be given in intractable oncologic pain, the quantity administered should be that which produces adequate analgesia with no or tolerable side effects. In published reports of adults with severe, chronic pain, maintenance dosages of CIVI usually have ranged from 0.8-80mg/hr. In a limited number of children with severe, chronic cancer pain, maintenance dosages of 0.025-2.6mg/kg/hr have been infused IV (median 0.04-0.07). Dosage for Neuraxial Administration In most cases the patient who initiates therapy with continuous intraspinal opioids will have been treated previously (unsuccessfully) with opioids either orally or parenterally. A patient’s intraspinal analgesic requirements can be estimated by using the following conversion ratio: 300 mg oral morphine equals 100 mg parenteral morphine equals 10 mg epidural morphine equals 1 mg intrathecal morphine (For patients who previously took opioids other than morphine, standard equianalgesic tables should be consulted for calculating the total daily opioid dose in morphine equivalents.) It is important to remember that all conversion tables/ ratios are meant to serve only as a guide and the dosage must always be adjusted according to the patient’s response. Patients whose pain is unusually severe or has a marked neuropathic component will often require higher intraspinal doses, while elderly patients will usually require lower intraspinal doses. In all cases, the starting dose must be individualized, based upon in-hospital evaluation of the response to serial single-dose epidural/intrathecal bolus injections of regular Morphine injections (preservative free) 0.5mg/ml and 1.0mg/ ml, with close observation of the analgesic efficacy and adverse effects prior to surgery involving the continuous microinfusion device. The usual starting dose for continuous epidural infusion, based upon limited data in patients who have some degree of opioid tolerance, is 4.5 to 10mg/ day. (The recommended initial epidural dose in patients who are not tolerant to opioids ranges from 3.5 to 7.5mg/day. However, continuous intraspinal opioid administration in opioid-naive patients is not generally recommended!!) The dose requirements may increase significantly during treatment. The upper daily limit for each patient must be individualized. The published literature suggests that most patients with severe chronic intractable pain will eventually require 10-100 mg/day. The recommended initial lumbar intrathecal dose range in patients with no tolerance to opioids is 0.2 to 1 mg/day. However, continuous intraspinal opioid administration in opioid-naive patients is not generally recommended!! The published range of doses for individuals who have some degree of opioid tolerance varies from 1 to 10mg/day. Limited experience with continuous intrathecal infusion of morphine has shown that the daily doses have to be increased over time. The upper daily dosage limit for each patient must be individualized. In a minority of patients, a daily dose of 10-20mg may be necessary. Doses greater than 20mg/day are rarely necessary and should be employed with caution since they may be associated with a higher likelihood of serious side effects such as myoclonus and respiratory depression. During the course of treatment, the patient may experience a recurrence of pain due to an increase in the level of pain because of disease progression or the development of tolerance to the drug. If this occurs, an increase in the dosage may be required. As there is no upper limit to the amount of morphine that may be given in intractable oncologic pain, the quantity administered should be that which produces adequate analgesia with no or tolerable side effects. If other measures to relieve pain (e.g. nerve blocks, cordotomy) are employed, the morphine dosage should be reduced to an appropriate level. In debilitated or geriatric patients, epidural or intrathecal administration should be undertaken only with extreme caution, using relatively small doses. Safety and efficacy of epidural or intrathecal administration in children have not been determined, and usage in this population is not generally recommended [see Use in Specific Populations (4.7)].

מסגרת הכללה בסל
התוויות הכלולות במסגרת הסל
| התוויה | תאריך הכללה | תחום קליני | Class Effect | מצב מחלה |
|---|---|---|---|---|
| MORPHINE | ||||
| HYDROMORPHONE | ||||
| For the relief of severe pain in cancer. |
שימוש לפי פנקס קופ''ח כללית 1994
Severe and intractable oncological and postoperative pain
תאריך הכללה מקורי בסל
01/01/1995
הגבלות
תרופה שאושרה לשימוש כללי בקופ'ח
מידע נוסף
