Quest for the right Drug
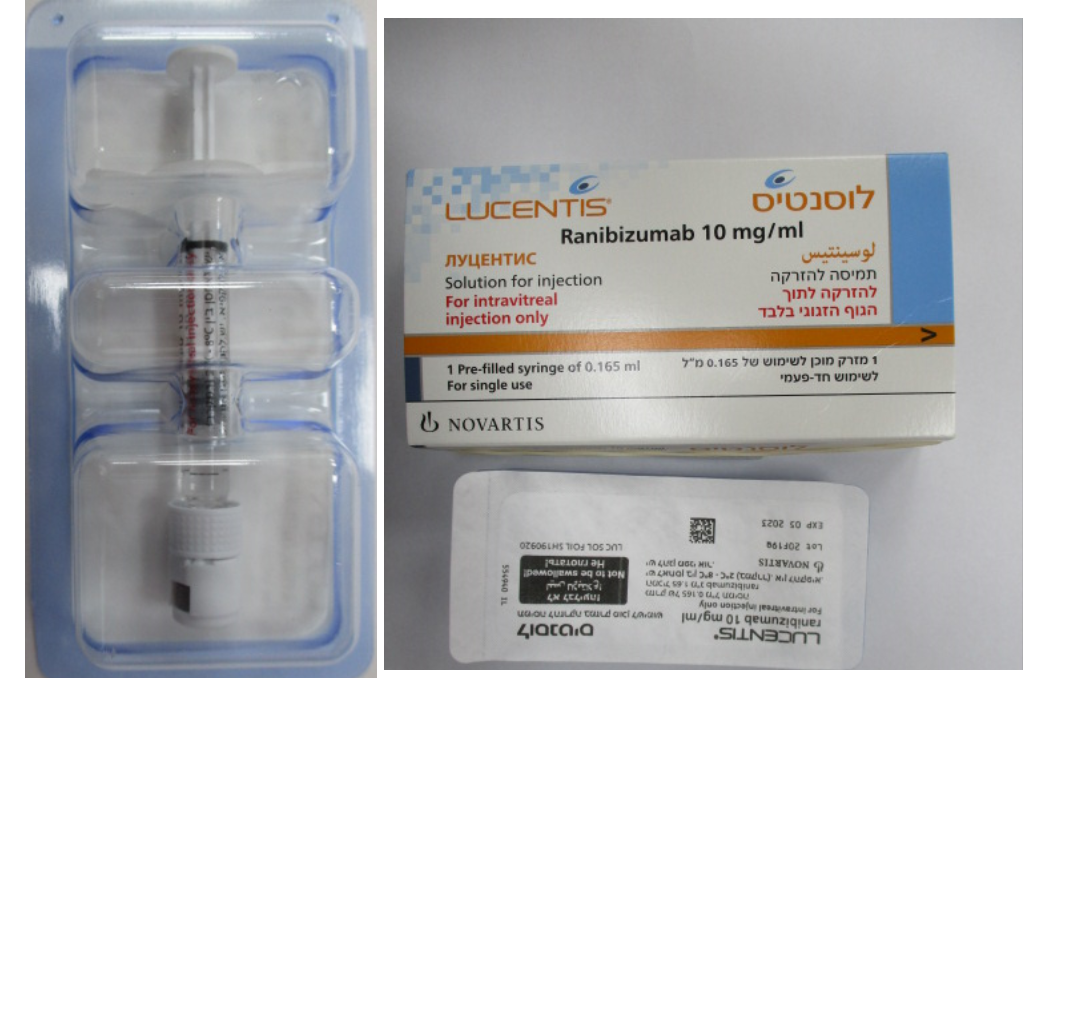
לוסנטיס LUCENTIS (RANIBIZUMAB)
תרופה במרשם
תרופה בסל
נרקוטיקה
ציטוטוקסיקה
צורת מתן:
לזגוגית העין : INTRAVITREAL
צורת מינון:
תמיסה להזרקה : SOLUTION FOR INJECTION
עלון לרופא
מינוניםPosology התוויות
Indications תופעות לוואי
Adverse reactions התוויות נגד
Contraindications אינטראקציות
Interactions מינון יתר
Overdose הריון/הנקה
Pregnancy & Lactation אוכלוסיות מיוחדות
Special populations תכונות פרמקולוגיות
Pharmacological properties מידע רוקחי
Pharmaceutical particulars אזהרת שימוש
Special Warning עלון לרופא
Physicians Leaflet
Pharmacological properties : תכונות פרמקולוגיות
Pharmacodynamic Properties
5.1 Pharmacodynamic properties Pharmacotherapeutic group: Ophthalmologicals, antineovascularisation agents, ATC code: S01LA04 Mechanism of action Ranibizumab is a humanised recombinant monoclonal antibody fragment targeted against human vascular endothelial growth factor A (VEGF-A). It binds with high affinity to the VEGF-A isoforms (e.g. VEGF110, VEGF121 and VEGF165), thereby preventing binding of VEGF-A to its receptors VEGFR-1 and VEGFR-2. Binding of VEGF-A to its receptors leads to endothelial cell proliferation and neovascularisation, as well as vascular leakage, all of which are thought to contribute to the progression of the neovascular form of age-related macular degeneration, pathologic myopia and CNV or to visual impairment caused by either diabetic macular oedema or macular oedema secondary to RVO in adults and retinopathy of prematurity in preterm infants. Clinical efficacy and safety Treatment of wet AMD In wet AMD, the clinical safety and efficacy of Lucentis have been assessed in three randomised, double- masked, sham- or active-controlled studies of 24 months duration in patients with neovascular AMD. A total of 1,323 patients (879 active and 444 control) were enrolled in these studies. In study FVF2598g (MARINA), 716 patients with minimally classic or occult with no classic lesions were randomised in a 1:1:1 ratio to receive monthly injections of Lucentis 0.3 mg, Lucentis 0.5 mg or sham. In study FVF2587g (ANCHOR), 423 patients with predominantly classic CNV lesions were randomised in a 1:1:1 ratio to receive Lucentis 0.3 mg monthly, Lucentis 0.5 mg monthly or verteporfin PDT (at baseline and every 3 months thereafter if fluorescein angiography showed persistence or recurrence of vascular leakage). Key outcome measures are summarised in Table 1 and Figure 1. Table 1 Outcomes at Month 12 and Month 24 in study FVF2598g (MARINA) and FVF2587g (ANCHOR) FVF2598g (MARINA) FVF2587g (ANCHOR) Outcome measure Month Sham Lucentis Verteporfin Lucentis (n=238) 0.5 mg PDT (n=143) 0.5 mg (n=240) (n=140) Loss of <15 letters in Month 12 62% 95% 64% 96% visual acuity (%)a Month 24 53% 90% 66% 90% (maintenance of vision, primary endpoint) Gain of ≥15 letters in Month 12 5% 34% 6% 40% visual acuity (%)a Month 24 4% 33% 6% 41% Mean change in Month 12 -10.5 (16.6) +7.2 (14.4) -9.5 (16.4) +11.3 (14.6) visual acuity (letters) Month 24 -14.9 (18.7) +6.6 (16.5) -9.8 (17.6) +10.7 (16.5) (SD)a a p<0.01 Figure 1 Mean change in visual acuity from baseline to Month 24 in study FVF2598g (MARINA) and study FVF2587g (ANCHOR) Study FVF2598g (MARINA) 15 Mean change in visual acuity ± SE 10 +6.6 5 (letters) 0 -5 + 21.5 -10 -15 -14.9 0 2 4 6 8 10 12 14 16 18 20 22 24 Month Study FVF2587g (ANCHOR) 15 Mean change in visual acuity ± SE +10.7 10 5 (letters) 0 +20.5 -5 -10 -9.8 -15 0 2 4 6 8 10 12 14 16 18 20 22 24 Month MARINA ANCHOR LUCENTIS 0.5 mg (n=240) LUCENTIS 0.5 mg (n=140) Sham (n=238) Verteporfin PDT (n=143) Results from both studies indicated that continued ranibizumab treatment may also be of benefit in patients who lost ≥15 letters of best-corrected visual acuity (BCVA) in the first year of treatment. Statistically significant patient-reported visual functioning benefits were observed in both MARINA and ANCHOR with ranibizumab treatment over the control group as measured by the NEI VFQ-25. In study FVF3192g (PIER), 184 patients with all forms of neovascular AMD were randomised in a 1:1:1 ratio to receive Lucentis 0.3 mg, Lucentis 0.5 mg or sham injections once a month for 3 consecutive doses, followed by a dose administered once every 3 months. From Month 14 of the study, sham-treated patients were allowed to receive ranibizumab and from Month 19, more frequent treatments were possible. Patients treated with Lucentis in PIER received a mean of 10 total treatments. After an initial increase in visual acuity (following monthly dosing), on average, patients’ visual acuity declined with quarterly dosing, returning to baseline at Month 12 and this effect was maintained in most ranibizumab-treated patients (82%) at Month 24. Limited data from sham subjects who later received ranibizumab suggested that early initiation of treatment may be associated with better preservation of visual acuity. Data from two studies (MONT BLANC, BPD952A2308 and DENALI, BPD952A2309) conducted post approval confirmed the efficacy of Lucentis but did not demonstrate additional effect of the combined administration of verteporfin (Visudyne PDT) and Lucentis compared to Lucentis monotherapy. Treatment of visual impairment due to CNV secondary to PM The clinical safety and efficacy of Lucentis in patients with visual impairment due to CNV in PM have been assessed based on the 12-month data of the double-masked, controlled pivotal study F2301 (RADIANCE). In this study 277 patients were randomised in a 2:2:1 ratio to the following arms: • Group I (ranibizumab 0.5 mg, dosing regimen driven by “stability” criteria defined as no change in BCVA compared to two preceding monthly evaluations). • Group II (ranibizumab 0.5 mg, dosing regimen driven by “disease activity” criteria defined as vision impairment attributable to intra- or subretinal fluid or active leakage due to the CNV lesion as assessed by optical coherence tomography and/or fluorescence angiography). • Group III (vPDT - patients were allowed to receive ranibizumab treatment as of Month 3). In Group II, which is the recommended posology (see section 4.2), 50.9% of patients required 1 or 2 injections, 34.5% required 3 to 5 injections and 14.7% required 6 to 12 injections over the 12-month study period. 62.9% of Group II patients did not require injections in the second 6 months of the study. The key outcomes from RADIANCE are summarised in Table 2 and Figure 2. Table 2 Outcomes at Month 3 and 12 (RADIANCE) Group I Group II Group III Ranibizumab Ranibizumab vPDTb 0.5 mg 0.5 mg “vision stability” “disease activity” (n=105) (n=116) (n=55) Month 3 Mean average BCVA change from Month 1 +10.5 +10.6 +2.2 to Month 3 compared to baselinea (letters) Proportion of patients who gained: ≥15 letters, or reached ≥84 letters in BCVA 38.1% 43.1% 14.5% Month 12 Number of injections up to Month 12: Mean 4.6 3.5 N/A Median 4.0 2.5 N/A Mean average BCVA change from Month 1 +12.8 +12.5 N/A to Month 12 compared to baseline (letters) Proportion of patients who gained: ≥15 letters, or reached ≥84 letters in BCVA 53.3% 51.7% N/A a p<0.00001 comparison with vPDT control b Comparative control up to Month 3. Patients randomised to vPDT were allowed to receive ranibizumab treatment as of Month 3 (in Group III, 38 patients received ranibizumab as of Month 3) Figure 2 Mean change from baseline BCVA over time to Month 12 (RADIANCE) 20 +14.4 15 +12.5 Mean VA change from BL + - SE (letters) +13.8 10 +12.1 +9.3 5 +1.4 0 Ranibizumab allowed -5 0 1 2 3 4 5 6 7 8 9 10 11 12 Month Ranibizumab 0.5 mg Group I Ranibizumab 0.5 mg Group II by stabilisation (n=105) by disease activity (n=116) Verteporfin PDT Group III (n=55) Ranibizumab 0.5 mg/Verteporfin PDT Group III from Month 3 onwards (n=55) The improvement of vision was accompanied by a reduction in central retinal thickness. Patient-reported benefits were observed with ranibizumab treatment arms over vPDT (p-value <0.05) in terms of improvement in the composite score and several subscales (general vision, near activities, mental health and dependency) of the NEI VFQ-25. Treatment of visual impairment due to CNV (other than secondary to PM and wet AMD) The clinical safety and efficacy of Lucentis in patients with visual impairment due to CNV have been assessed based on the 12-month data of the double-masked, sham-controlled pivotal study G2301 (MINERVA). In this study 178 adult patients were randomised in a 2:1 ratio to receive: • ranibizumab 0.5 mg at baseline, followed by an individualized dosing regimen driven by disease activity as assessed by visual acuity and/or anatomical parameters (e.g. visual acuity impairment, intra/sub-retinal fluid, hemorrhage or leakage); • sham injection at baseline, followed by an individualized treatment regimen driven by disease activity. At Month 2, all patients received open-label treatment with ranibizumab as needed. Key outcome measures from MINERVA are summarized in Table 3 and Figure 3. An improvement of vision was observed and was accompanied by a reduction in central subfield thickness over the 12-month period. The mean number of injections given over 12 months was 5.8 in the ranibizumab arm versus 5.4 in those patients in the sham arm who were eligible to receive ranibizumab from Month 2 onwards. In the sham arm 7 out of 59 patients did not receive any treatment with ranibizumab in the study eye during the 12- month period. Table 3 Outcomes at Month 2 (MINERVA) Ranibizumab Sham (n=59) 0.5 mg (n=119) Mean BCVA change from baseline to Month 2 a 9.5 letters -0.4 letters Patients gaining ≥15 letters from baseline or reaching 31.4% 12.3% 84 letters at Month 2 Patients not losing >15 letters from baseline at Month 2 99.2% 94.7% Reduction in CSFTb from baseline to Month 2 a 77 µm -9.8 µm a One-sided p<0.001 comparison with sham control b CSFT - central retinal subfield thickness Figure 3 Mean change from baseline BCVA over time to Month 12 (MINERVA) 11.0 9.4* 9.3 Mean BCVA change +/- 95% CI (letters) -0.3* Double-masked, Open-label, randomised, Ranibizumab allowed in both arms Ranibizumab vs Sham Month Treatment: Ranibizumab 0.5 mg (N=119) Sham (N=59) * Observed mean BCVA may differ from the Least Squares Mean BCVA (applicable only at Month 2) When comparing ranibizumab versus sham control at Month 2, a consistent treatment effect both overall and across baseline aetiology subgroups was observed: Table 4 Treatment effect overall and across baseline aetiology subgroups Overall and per baseline aetiology Treatment effect over Patient numbers [n] sham [letters] (treatment +sham) Overall 9.9 178 Angioid streaks 14.6 27 Post-inflammatory retinochoroidopathy 6.5 28 Central serous chorioretinopathy 5.0 23 Idiopathic chorioretinopathy 11.4 63 Miscellaneous aetiologies a 10.6 37 a encompasses different aetiologies of low frequency of occurrence not included in the other subgroups Treatment of visual impairment due to DME The efficacy and safety of Lucentis have been assessed in three randomised, controlled studies of at least 12 months duration. A total of 868 patients (708 active and 160 control) were enrolled in these studies. In the phase II study D2201 (RESOLVE), 151 patients were treated with ranibizumab (6 mg/ml, n=51, 10 mg/ml, n=51) or sham (n=49) by monthly intravitreal injections. The mean average change in BCVA from Month 1 to Month 12 compared to baseline was +7.8 (±7.72) letters in the pooled ranibizumab- treated patients (n=102), compared to -0.1 (±9.77) letters for sham-treated patients; and the mean change in BCVA at Month 12 from baseline was 10.3 (±9.1) letters compared to -1.4 (±14.2) letters, respectively (p<0.0001 for the treatment difference). In the phase III study D2301 (RESTORE), 345 patients were randomised in a 1:1:1 ratio to receive ranibizumab 0.5 mg monotherapy and sham laser photocoagulation, combined ranibizumab 0.5 mg and laser photocoagulation or sham injection and laser photocoagulation. 240 patients, who had previously completed the 12-month RESTORE study, were enrolled in the open-label, multicentre 24-month extension (RESTORE Extension) study. Patients were treated with ranibizumab 0.5 mg pro re nata (PRN) in the same eye as the core study (D2301 RESTORE). Key outcome measures are summarised in Table 5 (RESTORE and Extension) and Figure 4 (RESTORE). Figure 4 Mean change in visual acuity from baseline over time in study D2301 (RESTORE) 12 Mean VA change from BL + / - SE (letters) 10 8 + 6.8/+ 6.4 6 4 + 6.2/+ 5.4* 2 + 0.9 0 -2 -4 0 1 2 3 4 5 6 7 8 9 10 11 12 Month Treatment group Ranibizumab 0.5 mg (N = 115) Ranibizumab 0.5 mg + Laser (N = 118) Laser (N = 110) BL=baseline; SE=standard error of mean * Difference in least square means, p<0.0001/0.0004 based on two-sided stratified Cochran-Mantel- Haenszel test The effect at 12 months was consistent in most subgroups. However, subjects with a baseline BCVA >73 letters and macular oedema with central retinal thickness <300 µm did not appear to benefit from treatment with ranibizumab compared to laser photocoagulation. Table 5 Outcomes at Month 12 in study D2301 (RESTORE) and at Month 36 in study D2301- E1 (RESTORE Extension) Outcome measures at Month 12 compared Ranibizumab Ranibizumab Laser to baseline in study D2301 (RESTORE) 0.5 mg 0.5 mg + Laser n=115 n=118 n=110 Mean average change in BCVA from 6.1 (6.4)a 5.9 (7.9)a 0.8 (8.6) Month 1 to Month 12a (±SD) Mean change in BCVA at Month 12 (±SD) 6.8 (8.3)a 6.4 (11.8)a 0.9 (11.4) Gain of ≥15 letters or BCVA ≥84 letters at 22.6 22.9 8.2 Month 12 (%) Mean number of injections (Months 0-11) 7.0 6.8 7.3 (sham) Outcome measure at Month 36 compared Prior ranibizumab Prior ranibizumab Prior laser to D2301 (RESTORE) baseline in study 0.5 mg 0.5 mg + laser D2301-E1 (RESTORE Extension) n=83 n=83 n=74 Mean change in BCVA at Month 24 (SD) 7.9 (9.0) 6.7 (7.9) 5.4 (9.0) Mean change in BCVA at Month 36 (SD) 8.0 (10.1) 6.7 (9.6) 6.0 (9.4) Gain of ≥15 letters or BCVA ≥84 letters at 27.7 30.1 21.6 Month 36 (%) Mean number of injections 6.8 6.0 6.5 (Months 12-35)* a p<0.0001 for comparisons of ranibizumab arms vs. laser arm. n in D2301-E1 (RESTORE Extension) is the number of patients with a value at both D2301 (RESTORE) baseline (Month 0) and at the Month 36 visit. * The proportion of patients who did not require any ranibizumab treatment during the extension phase was 19%, 25% and 20% in the prior ranibizumab, prior ranibizumab + laser and prior laser groups, respectively. Statistically significant patient-reported benefits for most vision-related functions were observed with ranibizumab (with or without laser) treatment over the control group as measured by the NEI VFQ-25. For other subscales of this questionnaire no treatment differences could be established. The long-term safety profile of ranibizumab observed in the 24-month extension study is consistent with the known Lucentis safety profile. In the phase IIIb study D2304 (RETAIN), 372 patients were randomised in 1:1:1 ratio to receive: • ranibizumab 0.5 mg with concomitant laser photocoagulation on a treat-and-extend (TE) regimen, • ranibizumab 0.5 mg monotherapy on a TE regimen, • ranibizumab 0.5 mg monotherapy on a PRN regimen. In all groups, ranibizumab was administered monthly until BCVA was stable for at least three consecutive monthly assessments. On TE, ranibizumab was administered at treatment intervals of 2-3 months. In all groups, monthly treatment was re-initiated upon a decrease in BCVA due to DME progression and continued until stable BCVA was reached again. The number of scheduled treatment visits after the initial 3 injections, was 13 and 20 for the TE and PRN regimens, respectively. With both TE regimens, more than 70% of patients maintained their BCVA with an average visit frequency of ≥2 months. The key outcome measures are summarised in Table 6. Table 6 Outcomes in study D2304 (RETAIN) Outcome measure TE ranibizumab TE ranibizumab PRN ranibizumab compared to baseline 0.5 mg + laser 0.5 mg alone 0.5 mg n=117 n=125 n=117 Mean average change in BCVA from 5.9 (5.5) a 6.1 (5.7) a 6.2 (6.0) Month 1 to Month 12 (SD) Mean average change in BCVA from 6.8 (6.0) 6.6 (7.1) 7.0 (6.4) Month 1 to Month 24 (SD) Mean change in BCVA 8.3 (8.1) 6.5 (10.9) 8.1 (8.5) at Month 24 (SD) Gain of ≥15 letters or BCVA ≥84 letters at 25.6 28.0 30.8 Month 24(%) Mean number of injections 12.4 12.8 10.7 (months 0-23) a p<0.0001 for assessment of non-inferiority to PRN In DME studies, the improvement in BCVA was accompanied by a reduction over time in mean CSFT in all the treatment groups. Treatment of PDR The clinical safety and efficacy of Lucentis in patients with PDR have been assessed in Protocol S which evaluated the treatment with ranibizumab 0.5 mg intravitreal injections compared with panretinal photocoagulation (PRP). The primary endpoint was the mean visual acuity change at year 2. Additionally, change in diabetic retinopathy (DR) severity was assessed based on fundus photographs using the DR severity score (DRSS). Protocol S was a multicentre, randomised, active-controlled, parallel-assignment, non-inferiority phase III study in which 305 patients (394 study eyes) with PDR with or without DME at baseline were enrolled. The study compared ranibizumab 0.5 mg intravitreal injections to standard treatment with PRP. A total of 191 eyes (48.5%) were randomised to ranibizumab 0.5 mg and 203 eyes (51.5%) eyes were randomised to PRP. A total of 88 eyes (22.3%) had baseline DME: 42 (22.0%) and 46 (22.7%) eyes in the ranibizumab and PRP groups, respectively. In this study, the mean visual acuity change at year 2 was +2.7 letters in the ranibizumab group compared to -0.7 letters in the PRP group. The difference in least square means was 3.5 letters (95% CI: [0.2 to 6.7]). At year 1, 41.8% of eyes experienced a ≥2-step improvement in the DRSS when treated with ranibizumab (n=189) compared to 14.6% of eyes treated with PRP (n=199). The estimated difference between ranibizumab and laser was 27.4% (95% CI: [18.9, 35.9]). Table 7 DRSS improvement or worsening of ≥2 or ≥3 steps at year 1 in Protocol S (LOCF Method) Categorised change Protocol S from baseline Ranibizumab PRP Difference in 0.5 mg (N=199) proportion (%), CI (N=189) ≥2-step improvement n (%) 79 29 27.4 (41.8%) (14.6%) (18.9, 35.9) ≥3-step improvement n (%) 54 6 25.7 (28.6%) (3.0%) (18.9, 32.6) ≥2-step worsening n (%) 3 23 -9.9 (1.6%) (11.6%) (-14.7, -5.2) ≥3-step worsening n (%) 1 8 -3.4 (0.5%) (4.0%) (-6.3, -0.5) DRSS = diabetic retinopathy severity score, n = number of patients who satisfied the condition at the visit, N = total number of study eyes. At year 1 in the ranibizumab-treated group in Protocol S, ≥2-step improvement in DRSS was consistent in eyes without DME (39.9%) and with baseline DME (48.8%). An analysis of year 2 data from Protocol S demonstrated that 42.3% (n=80) of eyes in the ranibizumab- treated group had ≥2-step improvement in DRSS from baseline compared with 23.1% (n=46) of eyes in the PRP group. In the ranibizumab-treated group, ≥2-step improvement in DRSS from baseline was observed in 58.5% (n=24) of eyes with baseline DME and 37.8% (n=56) of eyes without DME. DRSS was also assessed in three separate active-controlled phase III DME studies (ranibizumab 0.5 mg PRN vs laser) that included a total of 875 patients, of whom approximately 75% were of Asian origin. In a meta-analysis of these studies, 48.4% of the 315 patients with gradable DRSS scores in the subgroup of patients with moderately severe non-proliferative DR (NPDR) or worse at baseline experienced a ≥2-step improvement in the DRSS at Month 12 when treated with ranibizumab (n=192) vs 14.6% of patients treated with laser (n=123). The estimated difference between ranibizumab and laser was 29.9% (95% CI: [20.0, 39.7]). In the 405 DRSS gradable patients with moderate NPDR or better, a ≥2-step DRSS improvement was observed in 1.4% and 0.9% of the ranibizumab and laser groups, respectively. Treatment of visual impairment due to macular oedema secondary to RVO The clinical safety and efficacy of Lucentis in patients with visual impairment due to macular oedema secondary to RVO have been assessed in the randomised, double-masked, controlled studies BRAVO and CRUISE that recruited subjects with BRVO (n=397) and CRVO (n=392), respectively. In both studies, subjects received either 0.3 mg or 0.5 mg ranibizumab or sham injections. After 6 months, patients in the sham-control arms switched to 0.5 mg ranibizumab. Key outcome measures from BRAVO and CRUISE are summarised in Table 8 and Figures 5 and 6. Table 8 Outcomes at Month 6 and 12 (BRAVO and CRUISE) BRAVO CRUISE Sham/Lucentis Lucentis Sham/Lucentis Lucentis 0.5 mg 0.5 mg 0.5 mg 0.5 mg (n=132) (n=131) (n=130) (n=130) Mean change in visual acuity 7.3 (13.0) 18.3 (13.2) 0.8 (16.2) 14.9 (13.2) at Month 6a (letters) (SD) (primary endpoint) Mean change in BCVA at 12.1 (14.4) 18.3 (14.6) 7.3 (15.9) 13.9 (14.2) Month 12 (letters) (SD) Gain of ≥15 letters in visual 28.8 61.1 16.9 47.7 acuity at Month 6a (%) Gain of ≥15 letters in visual 43.9 60.3 33.1 50.8 acuity at Month 12 (%) Proportion (%) receiving laser 61.4 34.4 NA NA rescue over 12 months a p<0.0001for both studies Figure 5 Mean change from baseline BCVA over time to Month 6 and Month 12 (BRAVO) Figure 6 Mean change from baseline BCVA over time to Month 6 and Month 12 (CRUISE) In both studies, the improvement of vision was accompanied by a continuous and significant reduction in the macular oedema as measured by central retinal thickness. In patients with CRVO (CRUISE and extension study HORIZON): Subjects treated with sham in the first 6 months who subsequently received ranibizumab did not achieve comparable gains in visual acuity by Month 24 (~6 letters) compared to subjects treated with ranibizumab from study start (~12 letters). Statistically significant patient-reported benefits in subscales related to near and distance activity were observed with ranibizumab treatment over the control group as measured by the NEI VFQ-25. The long-term (24 months) clinical safety and efficacy of Lucentis in patients with visual impairment due to macular oedema secondary to RVO were assessed in the BRIGHTER (BRVO) and CRYSTAL (CRVO) studies. In both studies, subjects received a 0.5 mg ranibizumab PRN dosing regimen driven by individualised stabilisation criteria. BRIGHTER was a 3-arm randomised active-controlled study that compared 0.5 mg ranibizumab given as monotherapy or in combination with adjunctive laser photocoagulation to laser photocoagulation alone. After 6 months, subjects in the laser arm could receive 0.5 mg ranibizumab. CRYSTAL was a single-arm study with 0.5 mg ranibizumab monotherapy. Key outcome measures from BRIGHTER and CRYSTAL are shown in Table 9. Table 9 Outcomes at Months 6 and 24 (BRIGHTER and CRYSTAL) BRIGHTER CRYSTAL Lucentis 0.5 mg Lucentis 0.5 mg + Laser* Lucentis 0.5 mg N=180 Laser N=90 N=356 N=178 Mean change in BCVA at +14.8 +14.8 +6.0 +12.0 Month 6a (letters) (10.7) (11.13) (14.27) (13.95) (SD) Mean change in BCVA at +15.5 +17.3 +11.6 +12.1 Month 24b (13.91) (12.61) (16.09) (18.60) (letters) (SD) Gain of ≥15 letters in 52.8 59.6 43.3 49.2 BCVA at Month 24 (%) Mean number of 11.4 injections (SD) 11.3 (6.02) NA 13.1 (6.39) (5.81) (months 0-23) a p<0.0001for both comparisons in BRIGHTER at Month 6: Lucentis 0.5 mg vs Laser and Lucentis 0.5 mg + Laser vs Laser. b p<0.0001for null hypothesis in CRYSTAL that the mean change at Month 24 from baseline is zero. * Starting at Month 6 ranibizumab 0.5 mg treatment was allowed (24 patients were treated with laser only). In BRIGHTER, ranibizumab 0.5 mg with adjunctive laser therapy demonstrated non-inferiority versus ranibizumab monotherapy from baseline to Month 24 (95% CI -2.8, 1.4). In both studies, a rapid and statistically significant decrease from baseline in central retinal subfield thickness was observed at Month 1. This effect was maintained up to Month 24. The effect of ranibizumab treatment was similar irrespective of the presence of retinal ischaemia. In BRIGHTER, patients with ischaemia present (N=46) or absent (N=133) and treated with ranibizumab monotherapy had a mean change from baseline of +15.3 and +15.6 letters, respectively, at Month 24. In CRYSTAL, patients with ischaemia present (N=53) or absent (N=300) and treated with ranibizumab monotherapy had a mean change from baseline of +15.0 and +11.5 letters, respectively. The effect in terms of visual improvement was observed in all patients treated with 0.5 mg ranibizumab monotherapy regardless of their disease duration in both BRIGHTER and CRYSTAL. In patients with <3 months disease duration an increase in visual acuity of 13.3 and 10.0 letters was seen at Month 1; and 17.7 and 13.2 letters at Month 24 in BRIGHTER and CRYSTAL, respectively. The corresponding visual acuity gain in patients with ≥12 months disease duration was 8.6 and 8.4 letters in the respective studies. Treatment initiation at the time of diagnosis should be considered. The long-term safety profile of ranibizumab observed in the 24-month studies is consistent with the known Lucentis safety profile. Paediatric population Treatment of ROP in preterm infants The clinical safety and efficacy of Lucentis 0.2 mg for the treatment of ROP in preterm infants have been assessed based on the 6-month data of the randomized, open-label, 3-arm, parallel-group superiority study H2301 (RAINBOW), which was designed to evaluate ranibizumab 0.2 mg and 0.1 mg given as intravitreal injections in comparison to laser therapy. Eligible patients had one of the following retinal findings in each eye: • Zone I, stage 1+, 2+, 3 or 3+ disease, or • Zone II, stage 3+ disease, or • Aggressive posterior (AP)-ROP In this study, 225 patients were randomized in a 1:1:1 ratio to receive intravitreal ranibizumab 0.2 mg (n=74), 0.1 mg (n=77), or laser therapy (n=74). Treatment success, as measured by the absence of active ROP and absence of unfavorable structural outcomes in both eyes 24 weeks after the first study treatment, was highest with ranibizumab 0.2 mg (80%) compared to laser therapy (66.2%) (see Table 10). The majority of patients treated with ranibizumab 0.2 mg (78.1%) received a single injection per eye. Table 10 Outcomes at Week 24 (RAINBOW) Treatment success Treatment n/M (%) 95% CI Comparison Odds ratio 95% CI p-valueb (OR)a Ranibizumab 56/70 (0.6873, Ranibizumab 2.19 (0.9932, 0.0254 0.2 mg (80.0) 0.8861) 0.2 mg vs 4.8235) (N=74) laser Laser therapy 45/68 (0.5368, (N=74) (66.2) 0.7721) CI = confidence interval, M = total number of patients with non-missing value on primary efficacy outcome (including imputed values), n = number of patients with absence of active ROP and absence of unfavourable structural outcome in both eyes 24 weeks after the first study treatment (including imputed values). If a patient died or switched study treatment before or at week 24, then the patient was considered as having active ROP and unfavourable structural outcomes at week 24. a Odds ratio is calculated by using Cochran-Mantel-Haenszel test with ROP zone at baseline (zone I and II; per CRF) as stratum factor. b p-value for pairwise comparison is one-sided. For the primary endpoint the pre-specified significance level for the one-sided p-value was 0.025. During the 24 weeks of the study, fewer patients in the ranibizumab 0.2 mg group switched to another treatment modality due to lack of response compared with the laser group (14.9% vs. 24.3%). Unfavourable structural outcomes were less frequently reported for ranibizumab 0.2 mg (1 patient, 1.4%) compared with laser therapy (7 patients, 10.1%). The long-term efficacy and safety of ranibizumab 0.2 mg for the treatment of ROP in preterm infants have been assessed in study H2301E1 (RAINBOW extension), an extension study of study H2301 (RAINBOW), following patients to their 5th birthday. The primary objective was to evaluate visual function at the patient’s 5th birthday visit by assessing visual acuity using Early Treatment Diabetic Retinopathy Study (ETDRS) with Lea symbols optotypes in the better-seeing eye (the eye with the higher ETDRS score). An ETDRS score in patients who completed the 5th birthday visit was recorded for 83.3% (45/54) and 76.6% (36/47) of patients in the ranibizumab 0.2 mg arm and the laser arm, respectively. The least-squares (LS) mean (SE) was numerically higher in the ranibizumab 0.2 mg arm (66.8 [1.95]) compared to the laser arm (62.1 [2.18]) with a difference in LS mean ETDRS score of 4.7 (95% CI: -1.1, 10.5). The categorised visual acuity outcomes in the better-seeing eye at the patients’ 5th birthday is presented in Table 11. Table 11 Visual acuity outcomes in the better-seeing eye1 at the patients’ 5th birthday visit Ranibizumab 0.2 mg Laser N=61 N=54 Visual acuity category n (%) n (%) ≥1 to ≤34 letters 1 (1.6) 2 (3.7) ≥35 to ≤70 letters 24 (39.3) 23 (42.6) ≥71 letters 20 (32.8) 11 (20.4) 1 The better-seeing eye is the eye with a higher ETDRS letter score at the 5th birthday visit. If both eyes have the same ETDRS letter score, then the right eye is assigned as the better-seeing eye. Paediatric population (PFS) The safety and efficacy of ranibizumab 0.5 mg in pre-filled syringe have not been studied in paediatric patients.
Pharmacokinetic Properties
5.2 Pharmacokinetic properties Following monthly intravitreal administration of Lucentis to patients with neovascular AMD, serum concentrations of ranibizumab were generally low, with maximum levels (Cmax) generally below the ranibizumab concentration necessary to inhibit the biological activity of VEGF by 50% (11-27 ng/ml, as assessed in an in vitro cellular proliferation assay). Cmax was dose proportional over the dose range of 0.05 to 1.0 mg/eye. Serum concentrations in a limited number of DME patients indicate that a slightly higher systemic exposure cannot be excluded compared to those observed in neovascular AMD patients. Serum ranibizumab concentrations in RVO patients were similar or slightly higher compared to those observed in neovascular AMD patients. Based on analysis of population pharmacokinetics and disappearance of ranibizumab from serum for patients with neovascular AMD treated with the 0.5 mg dose, the average vitreous elimination half-life of ranibizumab is approximately 9 days. Upon monthly intravitreal administration of Lucentis 0.5 mg/eye, serum ranibizumab Cmax, attained approximately 1 day after dosing, is predicted to generally range between 0.79 and 2.90 ng/ml, and Cmin is predicted to generally range between 0.07 and 0.49 ng/ml. Serum ranibizumab concentrations are predicted to be approximately 90,000-fold lower than vitreal ranibizumab concentrations. Patients with renal impairment: No formal studies have been conducted to examine the pharmacokinetics of Lucentis in patients with renal impairment. In a population pharmacokinetic analysis of neovascular AMD patients, 68% (136 of 200) of patients had renal impairment (46.5% mild [50-80 ml/min], 20% moderate [30-50 ml/min], and 1.5% severe [<30 ml/min]). In RVO patients, 48.2% (253 of 525) had renal impairment (36.4% mild, 9.5% moderate and 2.3% severe). Systemic clearance was slightly lower, but this was not clinically significant. Hepatic impairment: No formal studies have been conducted to examine the pharmacokinetics of Lucentis in patients with hepatic impairment. Paediatric population Following intravitreal administration of Lucentis to preterm infants with ROP at a dose of 0.2 mg (per eye), serum ranibizumab concentrations were higher than those observed in neovascular AMD adult patients receiving 0.5 mg in one eye. Based on a population pharmacokinetic analysis, the differences in Cmax and AUCinf were approximately 16-fold and 12-fold higher, respectively. The apparent systemic half-life was approximately 6 days. A PK/PD analysis showed no clear relationship between systemic ranibizumab concentrations and systemic VEGF concentrations.

פרטי מסגרת הכללה בסל
א. התרופה תינתן לטיפול במקרים האלה:1. פגיעה בראיה על רקע בצקת מקולרית סוכרתית (Diabetic macular edema - DME) בחולים שמיצו טיפול ב-Bevacizumab.במהלך מחלתו חולה יהיה זכאי לקבל טיפול באחת מהתרופות – Aflibercept, Dexamethasone implant, Faricimab, Ranibizumab.2. פגיעה בראיה על רקע CNV משנית לקוצר ראיה (מיופיה) פתולוגי בחולים שמיצו טיפול ב-Bevacizumab.במהלך מחלתו חולה יהיה זכאי לקבל טיפול באחת מהתרופות – Aflibercept, Ranibizumabב. לעניין זה מיצוי יוגדר בהתאם לכל התנאים האלה: 1. חולים לאחר סדרה של לפחות ארבע זריקות Bevacizumab(זריקה אחת לחודש) .2. ירידה של לפחות שורה בחדות הראיה או עליה של 10% או 50 מיקרון בעובי הרשתית המרכזית בהשוואה לממצאים טרם הזרקת Bevacizumab. אולא חל שינוי או שיפור של פחות משורה בחדות הראיה או ירידה של פחות מ-25% בעובי הרשתית המרכזית או העדר ספיגה או הצטברות של נוזל חדש בהשוואה לממצאים טרם הזרקת Bevacizumab. ג. הטיפול בתרופה ייעשה על פי מרשם של רופא מומחה ברפואת עיניים.
מסגרת הכללה בסל
התוויות הכלולות במסגרת הסל
| התוויה | תאריך הכללה | תחום קליני | Class Effect | מצב מחלה |
|---|---|---|---|---|
| פגיעה בראיה על רקע CNV משנית לקוצר ראיה (מיופיה) פתולוגי בחולים שמיצו טיפול ב-Bevacizumab. במהלך מחלתו חולה יהיה זכאי לקבל טיפול באחת מהתרופות – Aflibercept, Ranibizumab ב. לעניין זה מיצוי יוגדר בהתאם לכל התנאים האלה: 1. חולים לאחר סדרה של לפחות ארבע זריקות Bevacizumab(זריקה אחת לחודש) . 2. ירידה של לפחות שורה בחדות הראיה או עליה של 10% או 50 מיקרון בעובי הרשתית המרכזית בהשוואה לממצאים טרם הזרקת Bevacizumab. או לא חל שינוי או שיפור של פחות משורה בחדות הראיה או ירידה של פחות מ-25% בעובי הרשתית המרכזית או העדר ספיגה או הצטברות של נוזל חדש בהשוואה לממצאים טרם הזרקת Bevacizumab. | 16/01/2019 | עיניים | CNV משני לקוצר ראיה (מיופיה) | |
| פגיעה בראיה על רקע בצקת מקולרית סוכרתית (Diabetic macular edema - DME) בחולים שמיצו טיפול ב-Bevacizumab. במהלך מחלתו חולה יהיה זכאי לקבל טיפול באחת מהתרופות – Aflibercept, Dexamethasone implant, Ranibizumab | 11/01/2018 | עיניים | Diabetic macular edemea | |
| פגיעה בראיה על רקע בצקת מקולרית סוכרתית (Diabetic macular edema - DME) בחולים שמיצו טיפול ב-Bevacizumab. במהלך מחלתו חולה יהיה זכאי לקבל טיפול באחת מהתרופות – Aflibercept, Dexamethasone implant, Faricimab, Ranibizumab. | 01/02/2023 | עיניים | DME, Diabetic macular edema |
שימוש לפי פנקס קופ''ח כללית 1994
לא צוין
תאריך הכללה מקורי בסל
11/01/2018
הגבלות
תרופה מוגבלת לרישום ע'י רופא מומחה או הגבלה אחרת
מידע נוסף
עלון מידע לצרכן
06.01.19 - עלון לצרכן 18.04.22 - עלון לצרכן עברית 18.04.22 - עלון לצרכן עברית 11.10.22 - עלון לצרכן אנגלית 11.10.22 - עלון לצרכן אנגלית 11.10.22 - עלון לצרכן אנגלית 11.10.22 - עלון לצרכן עברית 11.10.22 - עלון לצרכן עברית 11.10.22 - עלון לצרכן ערבית 11.10.22 - עלון לצרכן ערבית 03.01.23 - עלון לצרכן עברית 03.01.23 - עלון לצרכן עברית 08.03.23 - עלון לצרכן אנגלית 08.03.23 - עלון לצרכן אנגלית 08.06.23 - עלון לצרכן עברית 08.06.23 - עלון לצרכן עברית 08.03.23 - עלון לצרכן ערבית 08.03.23 - עלון לצרכן ערבית 19.07.23 - עלון לצרכן אנגלית 19.07.23 - עלון לצרכן אנגלית 20.07.23 - עלון לצרכן ערבית 21.08.23 - עלון לצרכן ערבית 16.02.12 - החמרה לעלון 19.07.20 - החמרה לעלון 18.04.22 - החמרה לעלון 03.01.23 - החמרה לעלוןלתרופה במאגר משרד הבריאות
לוסנטיס