Quest for the right Drug
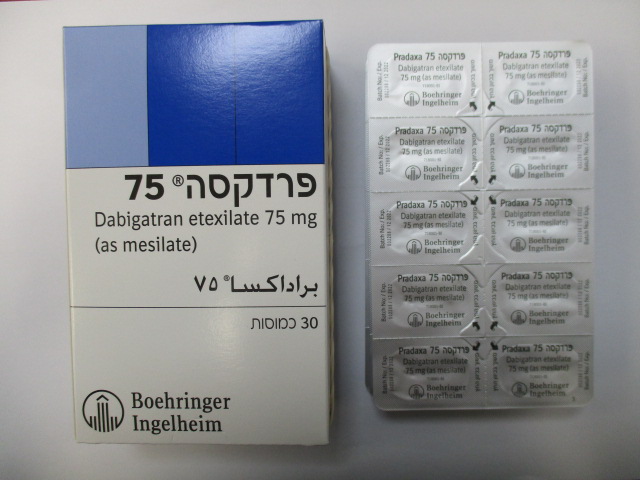
פרדקסה 75 PRADAXA 75 (DABIGATRAN ETEXILATE AS MESILATE)
תרופה במרשם
תרופה בסל
נרקוטיקה
ציטוטוקסיקה
צורת מתן:
פומי : PER OS
צורת מינון:
קפסולות : CAPSULES
עלון לרופא
מינוניםPosology התוויות
Indications תופעות לוואי
Adverse reactions התוויות נגד
Contraindications אינטראקציות
Interactions מינון יתר
Overdose הריון/הנקה
Pregnancy & Lactation אוכלוסיות מיוחדות
Special populations תכונות פרמקולוגיות
Pharmacological properties מידע רוקחי
Pharmaceutical particulars אזהרת שימוש
Special Warning עלון לרופא
Physicians Leaflet
Pharmacological properties : תכונות פרמקולוגיות
Pharmacodynamic Properties
5.1 Pharmacodynamic properties Pharmacotherapeutic group: antithrombotic agents, direct thrombin inhibitors, ATC code: B01AE07. Mechanism of action Dabigatran etexilate is a small molecule prodrug which does not exhibit any pharmacological activity. After oral administration, dabigatran etexilate is rapidly absorbed and converted to dabigatran by esterase-catalysed hydrolysis in plasma and in the liver. Dabigatran is a potent, competitive, reversible direct thrombin inhibitor and is the main active principle in plasma. Since thrombin (serine protease) enables the conversion of fibrinogen into fibrin during the coagulation cascade, its inhibition prevents the development of thrombus. Dabigatran inhibits free thrombin, fibrin-bound thrombin and thrombin-induced platelet aggregation. Pradaxa 75 Prescribing Information Boehringer Ingelheim January 2022 Pharmacodynamic effects In vivo and ex vivo animal studies have demonstrated antithrombotic efficacy and anticoagulant activity of dabigatran after intravenous administration and of dabigatran etexilate after oral administration in various animal models of thrombosis. There is a clear correlation between plasma dabigatran concentration and degree of anticoagulant effect based on phase II studies. Dabigatran prolongs the thrombin time (TT), ECT, and aPTT. The calibrated quantitative diluted TT (dTT) test provides an estimation of dabigatran plasma concentration that can be compared to the expected dabigatran plasma concentrations. When the calibrated dTT assay delivers a dabigatran plasma concentration result at or below the limit of quantification, an additional coagulation assay such as TT, ECT or aPTT should be considered. The ECT can provide a direct measure of the activity of direct thrombin inhibitors. The aPTT test is widely available and provides an approximate indication of the anticoagulation intensity achieved with dabigatran. However, the aPTT test has limited sensitivity and is not suitable for precise quantification of anticoagulant effect, especially at high plasma concentrations of dabigatran. Although high aPTT values should be interpreted with caution, a high aPTT value indicates that the patient is anticoagulated. In general, it can be assumed that these measures of anti-coagulant activity may reflect dabigatran levels and can provide guidance for the assessment of bleeding risk, i.e. exceeding the 90th percentile of dabigatran trough levels or a coagulation assay such as aPTT measured at trough (for aPTT thresholds see section 4.4, table 3) is considered to be associated with an increased risk of bleeding. Primary prevention of VTE in orthopaedic surgery Steady state (after day 3) geometric mean dabigatran peak plasma concentration, measured around 2 hours after 220 mg dabigatran etexilate administration, was 70.8 ng/mL, with a range of 35.2-162 ng/mL (25th-75th percentile range). The dabigatran geometric mean trough concentration, measured at the end of the dosing interval (i.e. 24 hours after a 220 mg dabigatran dose), was on average 22.0 ng/mL, with a range of 13.0-35.7 ng/mL (25th-75th percentile range). In a dedicated study exclusively in patients with moderate renal impairment (creatinine clearance, CrCL 30- 50 mL/min) treated with dabigatran etexilate 150 mg QD, the dabigatran geometric mean trough concentration, measured at the end of the dosing interval, was on average 47.5 ng/mL, with a range of 29.6 - 72.2 ng/mL (25th- 75th percentile range). In patients treated for prevention of VTEs after hip or knee replacement surgery with 220 mg dabigatran etexilate once daily, • the 90th percentile of dabigatran plasma concentrations was 67 ng/mL, measured at trough (20-28 hours after the previous dose) (see section 4.4 and 4.9), • the 90th percentile of aPTT at trough (20-28 hours after the previous dose) was 51 seconds, which would be 1.3-fold upper limit of normal. The ECT was not measured in patients treated for prevention of VTEs after hip or knee replacement surgery with 220 mg dabigatran etexilate once daily. Pradaxa 75 Prescribing Information Boehringer Ingelheim January 2022 Clinical efficacy and safety Ethnic origin No clinically relevant ethnic differences among Caucasians, African-American, Hispanic, Japanese or Chinese patients were observed. Clinical trials in Venous Thromboembolism (VTE) prophylaxis following major joint replacement surgery In 2 large randomised, parallel group, double-blind, dose-confirmatory trials, patients undergoing elective major orthopaedic surgery (one for knee replacement surgery and one for hip replacement surgery) received 75 mg or 110 mg dabigatran etexilate within 1-4 hours of surgery followed by 150 mg or 220 mg once daily thereafter, haemostasis having been secured, or enoxaparin 40 mg on the day prior to surgery and daily thereafter. In the RE-MODEL trial (knee replacement) treatment was for 6-10 days and in the RE-NOVATE trial (hip replacement) for 28-35 days. Totals of 2,076 patients (knee) and 3,494 (hip) were treated respectively. Composite of total VTE (including pulmonary embolism (PE), proximal and distal deep vein thrombosis (DVT), whatever symptomatic or asymptomatic detected by routine venography) and all-cause mortality constituted the primary end-point for both studies. Composite of major VTE (including PE and proximal DVT, whatever symptomatic or asymptomatic detected by routine venography) and VTE-related mortality constituted a secondary end-point and is considered of better clinical relevance. Results of both studies showed that the antithrombotic effect of 220 mg and 150 mg dabigatran etexilate were statistically non-inferior to that of enoxaparin on total VTE and all-cause mortality. The point estimate for incidence of major VTE and VTE related mortality for the 150 mg dose was slightly worse than enoxaparin (table 10). Better results were seen with the 220 mg dose where the point estimate of Major VTE was slightly better than enoxaparin (table 10). The clinical studies have been conducted in a patient population with a mean age > 65 years. There were no differences in the phase 3 clinical studies for efficacy and safety data between men and women. In the studied patient population of RE-MODEL and RE-NOVATE (5,539 patients treated), 51 % suffered from concomitant hypertension, 9 % from concomitant diabetes, 9 % from concomitant coronary artery disease and 20 % had a history of venous insufficiency. None of these diseases showed an impact on the effects of dabigatran on VTE-prevention or bleeding rates. Data for the major VTE and VTE-related mortality endpoint were homogeneous with regards to the primary efficacy endpoint and are shown in table 10. Data for the total VTE and all cause mortality endpoint are shown in table 11. Data for adjudicated major bleeding endpoints are shown in table 12 below. Pradaxa 75 Prescribing Information Boehringer Ingelheim January 2022 Table 10:Analysis of major VTE and VTE-related mortality during the treatment period in the RE-MODEL and the RE-NOVATE orthopaedic surgery studies Trial Dabigatran etexilate Dabigatran etexilate Enoxaparin 220 mg 150 mg 40 mg RE-NOVATE (hip) N 909 888 917 Incidences (%) 28 (3.1) 38 (4.3) 36 (3.9) Risk ratio over 0.78 1.09 enoxaparin 95 % CI 0.48, 1.27 0.70, 1.70 RE-MODEL (knee) N 506 527 511 Incidences (%) 13 (2.6) 20 (3.8) 18 (3.5) Risk ratio over 0.73 1.08 enoxaparin 95 % CI 0.36, 1.47 0.58, 2.01 Table 11: Analysis of total VTE and all cause mortality during the treatment period in the RE-NOVATE and the RE-MODEL orthopaedic surgery studies Trial Dabigatran etexilate Dabigatran etexilate Enoxaparin 220 mg 150 mg 40 mg RE-NOVATE (hip) N 880 874 897 Incidences (%) 53 (6.0) 75 (8.6) 60 (6.7) Risk ratio over 0.9 1.28 enoxaparin 95 % CI (0.63, 1.29) (0.93, 1.78) RE-MODEL (knee) N 503 526 512 Incidences (%) 183 (36.4) 213 (40.5) 193 (37.7) Risk ratio over 0.97 1.07 enoxaparin 95 % CI (0.82, 1.13) (0.92, 1.25) Pradaxa 75 Prescribing Information Boehringer Ingelheim January 2022 Table 12:Major bleeding events by treatment in the individual RE-MODEL and the RE-NOVATE studies Trial Dabigatran etexilate Dabigatran etexilate Enoxaparin 220 mg 150 mg 40 mg RE-NOVATE (hip) Treated patients N 1,146 1,163 1,154 Number of MBE 23 (2.0) 15 (1.3) 18 (1.6) N(%) RE-MODEL (knee) Treated patients N 679 703 694 Number of MBE 10 (1.5) 9 (1.3) 9 (1.3) N(%) Clinical trials for the prevention of thromboembolism in patients with prosthetic heart valves A phase II study examined dabigatran etexilate and warfarin in a total of 252 patients with recent mechanical valve replacement surgery (i.e. within the current hospital stay) and in patients who received a mechanical heart valve replacement more than three months ago. More thromboembolic events (mainly strokes and symptomatic/asymptomatic prosthetic valve thrombosis) and more bleeding events were observed with dabigatran etexilate than with warfarin. In the early post-operative patients, major bleeding manifested predominantly as haemorrhagic pericardial effusions, specifically in patients who started dabigatran etexilate early (i.e. on Day 3) after heart valve replacement surgery (see section 4.3).
Pharmacokinetic Properties
5.2 Pharmacokinetic properties After oral administration, dabigatran etexilate is rapidly and completely converted to dabigatran, which is the active form in plasma. The cleavage of the prodrug dabigatran etexilate by esterase-catalysed hydrolysis to the active principle dabigatran is the predominant metabolic reaction. The absolute bioavailability of dabigatran following oral administration of Pradaxa was approximately 6.5 %. After oral administration of Pradaxa in healthy volunteers, the pharmacokinetic profile of dabigatran in plasma is characterised by a rapid increase in plasma concentrations with Cmax attained within 0.5 and 2.0 hours post administration. Absorption A study evaluating post-operative absorption of dabigatran etexilate, 1-3 hours following surgery, demonstrated relatively slow absorption compared with that in healthy volunteers, showing a smooth plasma concentration-time profile without high peak plasma concentrations. Peak plasma concentrations are reached at 6 hours following administration in a postoperative period due to contributing factors such as anaesthesia, gastrointestinal paresis, and surgical effects independent of the oral medicinal product formulation. It was demonstrated in a further study that slow and delayed absorption is usually only present on the day of surgery. On subsequent days absorption of dabigatran is rapid with peak plasma concentrations attained 2 hours after medicinal product administration. Food does not affect the bioavailability of dabigatran etexilate but delays the time to peak plasma concentrations by 2 hours. Cmax and AUC were dose proportional. Pradaxa 75 Prescribing Information Boehringer Ingelheim January 2022 The oral bioavailability may be increased by 75 % after a single dose and 37 % at steady state compared to the reference capsule formulation when the pellets are taken without the Hydroxypropylmethylcellulose (HPMC) capsule shell. Hence, the integrity of the HPMC capsules should always be preserved in clinical use to avoid unintentionally increased bioavailability of dabigatran etexilate (see section 4.2). Distribution Low (34-35 %) concentration independent binding of dabigatran to human plasma proteins was observed. The volume of distribution of dabigatran of 60–70 L exceeded the volume of total body water indicating moderate tissue distribution of dabigatran. Biotransformation Metabolism and excretion of dabigatran were studied following a single intravenous dose of radiolabeled dabigatran in healthy male subjects. After an intravenous dose, the dabigatran-derived radioactivity was eliminated primarily in the urine (85 %). Faecal excretion accounted for 6 % of the administered dose. Recovery of the total radioactivity ranged from 88-94 % of the administered dose by 168 hours post dose. Dabigatran is subject to conjugation forming pharmacologically active acylglucuronides. Four positional isomers, 1-O, 2-O, 3-O, 4-O-acylglucuronide exist, each accounts for less than 10 % of total dabigatran in plasma. Traces of other metabolites were only detectable with highly sensitive analytical methods. Dabigatran is eliminated primarily in the unchanged form in the urine, at a rate of approximately 100 mL/min corresponding to the glomerular filtration rate. Elimination Plasma concentrations of dabigatran showed a biexponential decline with a mean terminal half-life of 11 hours in healthy elderly subjects. After multiple doses a terminal half-life of about 12-14 hours was observed. The half-life was independent of dose. Half-life is prolonged if renal function is impaired as shown in table 13. Special populations Renal insufficiency In phase I studies the exposure (AUC) of dabigatran after the oral administration of dabigatran etexilate is approximately 2.7-fold higher in adult volunteers with moderate renal insufficiency (CrCL between 30 and 50 mL/min) than in those without renal insufficiency. In a small number of adult volunteers with severe renal insufficiency (CrCL 10-30 mL/min), the exposure (AUC) to dabigatran was approximately 6 times higher and the half-life approximately 2 times longer than that observed in a population without renal insufficiency (see sections 4.2, 4.3 and 4.4). Pradaxa 75 Prescribing Information Boehringer Ingelheim January 2022 Table 13: Half-life of total dabigatran in healthy subjects and subjects with impaired renal function. glomerular filtration rate gMean (gCV%; range) (CrCL,) half-life [mL/min] [h] ≥80 13.4 (25.7 %; 11.0-21.6) ≥50-<80 15.3 (42.7 %;11.7-34.1) ≥30-<50 18.4 (18.5 %;13.3-23.0) <30 27.2(15.3 %; 21.6-35.0) Additionally, dabigatran exposure (at trough and peak) was assessed in a prospective open label randomised pharmacokinetic study in NVAF patients with severe renal impairment (defined as creatinine clearance [CrCl] 15-30 mL/min) receiving dabigatran etexilate 75 mg twice daily. This regimen resulted in a geometric mean trough concentration of 155 ng/ml (gCV of 76.9 %), measured immediately before administration of the next dose and in a geometric mean peak concentration of 202 ng/ml (gCV of 70.6 %) measured two hours after the administration of the last dose. Clearance of dabigatran by haemodialysis was investigated in 7 adult patients with end-stage renal disease (ESRD) without atrial fibrillation. Dialysis was conducted with 700 mL/min dialysate flow rate, four hour duration and a blood flow rate of either 200 mL/min or 350-390 mL/min. This resulted in a removal of 50 % to 60 % of dabigatran concentrations, respectively. The amount of substance cleared by dialysis is proportional to the blood flow rate up to a blood flow rate of 300 mL/min. The anticoagulant activity of dabigatran decreased with decreasing plasma concentrations and the PK/PD relationship was not affected by the procedure. Elderly patients Specific pharmacokinetic phase I studies with elderly subjects showed an increase of 40 to 60 % in the AUC and of more than 25 % in Cmax compared to young subjects. The effect by age on exposure to dabigatran was confirmed in the RE-LY study with an about 31 % higher trough concentration for subjects ≥ 75 years and by about 22 % lower trough level for subjects <65 years compared to subjects between 65 and 75 years (see sections 4.2 and 4.4). Hepatic impairment No change in dabigatran exposure was seen in 12 adult subjects with moderate hepatic insufficiency (Child Pugh B) compared to 12 controls (see sections 4.2 and 4.4). Body weight The dabigatran trough concentrations were about 20 % lower in adult patients with a body weight >100 kg compared with 50-100 kg. The majority (80.8 %) of the subjects were in the ≥50 kg and <100 kg category with no clear difference detected (see sections 4.2 and 4.4). Limited clinical data in adult patients <50 kg are available. Gender Active substance exposure in the primary VTE prevention studies was about 40 % to 50 % higher in female patients and no dose adjustment is recommended. Ethnic origin No clinically relevant inter-ethnic differences among Caucasian, African-American, Hispanic, Japanese or Chinese patients were observed regarding dabigatran pharmacokinetics and pharmacodynamics. Pradaxa 75 Prescribing Information Boehringer Ingelheim January 2022 Pharmacokinetic interactions In vitro interaction studies did not show any inhibition or induction of the principal isoenzymes of cytochrome P450. This has been confirmed by in vivo studies with healthy volunteers, who did not show any interaction between this treatment and the following active substances: atorvastatin (CYP3A4), digoxin (P-gp transporter interaction) and diclofenac (CYP2C9).

פרטי מסגרת הכללה בסל
התרופה תינתן לטיפול במקרים האלה: 1. מניעת תרומבואמבוליזם לאחר ניתוח להחלפת מפרק הירך; 2. מניעת תרומבואמבוליזם לאחר ניתוח להחלפת הברך; 3.מניעת שבץ ותסחיף סיסטמי בחולים עם פרפור עליות המטופלים ב-warfarin וחוו CVA או TIA עם ביטוי קליני (שטופל או אובחן בבית חולים) במהלך השנה האחרונה; 4. מניעת שבץ ותסחיף סיסטמי בחולים עם פרפור עליות המטופלים ב-Warfarin ושתועד אצלם INR גבוה מ-5 לפחות פעמיים במהלך השנה האחרונה באירועים נפרדים; 5. מניעת שבץ ותסחיף סיסטמי בחולים עם פרפור עליות ללא מחלה מסתמית ו-CHA2DS2 VASc score בערך 2 ומעלה.6. טיפול קצר טווח למניעת שבץ ותסחיף סיסטמי בחולים עם פרפור עליות בלא מחלה מסתמית ו-CHADS2 score בערך 0 או 1 אחרי היפוך קצב ופעולות של אבלציות בפרפור.7. טיפול ומניעה שניונית של פקקת הורידים העמוקים (Deep vein thrombosis – DVT).8. טיפול ומניעה שניונית של תסחיף ריאתי (Pulmonary embolism - PE).
מסגרת הכללה בסל
התוויות הכלולות במסגרת הסל
| התוויה | תאריך הכללה | תחום קליני | Class Effect | מצב מחלה |
|---|---|---|---|---|
| מניעת שבץ ותסחיף סיסטמי בחולים עם פרפור עליות בלא מחלה מסתמית ו-CHA2DS2 VASc score בערך 2 ומעלה. | 16/01/2019 | המטולוגיה | DABIGATRAN ETEXILATE, RIVAROXABAN, EDOXABAN, APIXABAN | |
| טיפול ומניעה שניונית של תסחיף ריאתי (Pulmonary embolism - PE). | 11/01/2018 | המטולוגיה | DABIGATRAN ETEXILATE, RIVAROXABAN, EDOXABAN, APIXABAN | |
| טיפול ומניעה שניונית של פקקת הורידים העמוקים (Deep vein thrombosis – DVT). | 11/01/2018 | המטולוגיה | DABIGATRAN ETEXILATE, RIVAROXABAN, EDOXABAN, APIXABAN | |
| טיפול קצר טווח למניעת שבץ ותסחיף סיסטמי בחולים עם פרפור עליות בלא מחלה מסתמית ו-CHADS2 score בערך 0 או 1 אחרי היפוך קצב ופעולות של אבלציות בפרפור | 11/01/2018 | המטולוגיה | DABIGATRAN ETEXILATE, RIVAROXABAN, EDOXABAN, APIXABAN | |
| . מניעת שבץ ותסחיף סיסטמי בחולים עם פרפור עליות בלא מחלה מסתמית ו-CHA2DS2 score בערך 2 ומעלה. | 21/01/2016 | המטולוגיה | DABIGATRAN ETEXILATE, RIVAROXABAN, EDOXABAN, APIXABAN | |
| . מניעת שבץ ותסחיף סיסטמי בחולים עם פרפור עליות בלא מחלה מסתמית ו-CHA2DS2 score בערך 3 ומעלה. | 12/01/2014 | המטולוגיה | DABIGATRAN ETEXILATE, RIVAROXABAN, EDOXABAN, APIXABAN | |
| . מניעת שבץ ותסחיף סיסטמי בחולים עם פרפור עליות בלא מחלה מסתמית ו-CHA2DS2 score בערך 4 ומעלה. | 10/01/2012 | המטולוגיה | DABIGATRAN ETEXILATE, RIVAROXABAN, EDOXABAN, APIXABAN | |
| מניעת שבץ ותסחיף סיסטמי בחולים עם פרפור עליות המטופלים ב-Warfarin ושתועד אצלם INR גבוה מ-5 לפחות פעמיים במהלך השנה האחרונה באירועים נפרדים. | 23/01/2011 | המטולוגיה | DABIGATRAN ETEXILATE, RIVAROXABAN, EDOXABAN, APIXABAN | |
| מניעת שבץ ותסחיף סיסטמי בחולים עם פרפור עליות המטופלים ב-warfarin וחוו CVA או TIA עם ביטוי קליני (שטופל או אובחן בבית חולים) במהלך השנה האחרונה. | 23/01/2011 | המטולוגיה | DABIGATRAN ETEXILATE, RIVAROXABAN, APIXABAN | |
| מניעת תרומבואמבוליזם לאחר ניתוח להחלפת הברך. | 03/01/2010 | אורתופדיה | DABIGATRAN ETEXILATE, RIVAROXABAN, APIXABAN | |
| מניעת תרומבואמבוליזם לאחר ניתוח להחלפת מפרק הירך | 03/01/2010 | אורתופדיה | DABIGATRAN ETEXILATE, RIVAROXABAN, APIXABAN |
שימוש לפי פנקס קופ''ח כללית 1994
לא צוין
תאריך הכללה מקורי בסל
03/01/2010
הגבלות
תרופה מוגבלת לרישום ע'י רופא מומחה או הגבלה אחרת
מידע נוסף
עלון מידע לרופא
28.02.22 - עלון לרופאעלון מידע לצרכן
10.11.13 - עלון לצרכן 03.10.19 - עלון לצרכן עברית 03.10.19 - עלון לצרכן ערבית 03.10.19 - עלון לצרכן ערבית 03.10.19 - עלון לצרכן 05.08.20 - עלון לצרכן אנגלית 02.06.19 - עלון לצרכן עברית 05.08.20 - עלון לצרכן עברית 05.08.20 - עלון לצרכן ערבית 30.11.11 - החמרה לעלון 26.07.12 - החמרה לעלון 25.12.12 - החמרה לעלון 12.07.15 - החמרה לעלון 17.01.17 - החמרה לעלון 02.06.19 - החמרה לעלון 01.09.19 - החמרה לעלון 05.08.20 - החמרה לעלון 05.08.20 - החמרה לעלון 28.02.22 - החמרה לעלוןלתרופה במאגר משרד הבריאות
פרדקסה 75