Quest for the right Drug
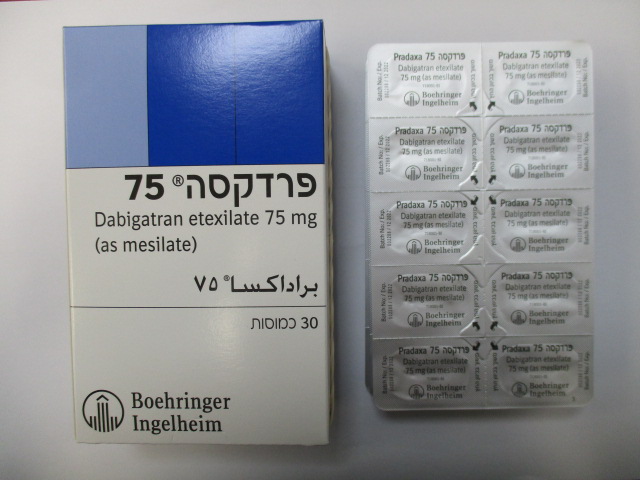
פרדקסה 75 PRADAXA 75 (DABIGATRAN ETEXILATE AS MESILATE)
תרופה במרשם
תרופה בסל
נרקוטיקה
ציטוטוקסיקה
צורת מתן:
פומי : PER OS
צורת מינון:
קפסולות : CAPSULES
עלון לרופא
מינוניםPosology התוויות
Indications תופעות לוואי
Adverse reactions התוויות נגד
Contraindications אינטראקציות
Interactions מינון יתר
Overdose הריון/הנקה
Pregnancy & Lactation אוכלוסיות מיוחדות
Special populations תכונות פרמקולוגיות
Pharmacological properties מידע רוקחי
Pharmaceutical particulars אזהרת שימוש
Special Warning עלון לרופא
Physicians Leaflet
Special Warning : אזהרת שימוש
4.4 Special warnings and precautions for use Increased risk of stroke with discontinuation of Pradaxa Discontinuing Pradaxa in the absence of adequate alternative anticoagulation increases the risk of thrombotic events. If Pradaxa must be discontinued for a reason other than pathological bleeding, consider coverage with another anticoagulant. Haemorrhagic risk Dabigatran etexilate should be used with caution in conditions with an increased risk of bleeding or with concomitant use of medicinal products affecting haemostasis by inhibition of platelet aggregation. Bleeding can occur at any site during therapy. An unexplained fall in haemoglobin and/or haematocrit or blood pressure should lead to a search for a bleeding site. For adult patients in situations of life-threatening or uncontrolled bleeding, when rapid reversal of the anticoagulation effect of dabigatran is required, the specific reversal agent (idarucizumab) is available. Haemodialysis can remove dabigatran. For adult patients, fresh whole blood or fresh frozen plasma, coagulation Pradaxa 75 Prescribing Information Boehringer Ingelheim January 2022 factor concentration (activated or non-activated), recombinant factor VIIa or platelet concentrates are other possible options (see also section 4.9). Use of platelet aggregation inhibitors such as clopidogrel and acetylsalicylic acid (ASA) or non steroidal antiinflammatory drugs (NSAID), as well as the presence of esophagitis, gastritis or gastroesophageal reflux increase the risk of GI bleeding. Risk factors Table 2 summarises factors which may increase the haemorrhagic risk. Table 2: Factors which may increase the haemorrhagic risk. Risk factor Pharmacodynamic and kinetic factors Age ≥75 years Factors increasing dabigatran plasma levels Major: • Moderate renal impairment in adult patients (30-50 mL/min CrCL) • Strong P-gp inhibitors (see section 4.3 and 4.5) • Mild to moderate P-gp inhibitor co-medication (e.g. amiodarone, verapamil, quinidine and ticagrelor; see section 4.5) Minor: • Low body weight (<50 kg) in adult patients Pharmacodynamic interactions (see section • ASA and other platelet aggregation inhibitors 4.5) such as clopidogrel • NSAID • SSRIs or SNRIs • Other medicinal products which may impair haemostasis Diseases / procedures with special • Congenital or acquired coagulation disorders haemorrhagic risks • Thrombocytopenia or functional platelet defects • Recent biopsy, major trauma • Bacterial endocarditis • Esophagitis, gastritis or gastroesophageal reflux Limited data is available in adult patients <50 kg (see section 5.2). Precautions and management of the haemorrhagic risk For the management of bleeding complications, see also section 4.9. Benefit-risk assessment The presence of lesions, conditions, procedures and/or pharmacological treatment (such as NSAIDs, antiplatelets, SSRIs and SNRIs, see section 4.5), which significantly increase the risk of major bleeding requires a careful benefit-risk assessment. This is especially relevant in specific patient groups at risk, such as Pradaxa 75 Prescribing Information Boehringer Ingelheim January 2022 elderly (age > 75), patients with impaired renal function (CrCl 30-50ml/min), patients on concomitant use of P-gp inhibitors or a combination of the above. Dabigatran etexilate should only be given if the benefit outweighs bleeding risks. Close clinical surveillance Close observation for signs of bleeding or anaemia is recommended throughout the treatment period, especially if risk factors are combined (see table 2 above). Particular caution should be exercised when dabigatran etexilate is co-administered with verapamil, amiodarone, quinidine or clarithromycin (P-gp inhibitors) and particularly in the occurrence of bleeding, notably in patients having a reduced renal function (see section 4.5). Close observation for signs of bleeding is recommended in patients concomitantly treated with NSAIDs (see section 4.5). Discontinuation of dabigatran etexilate Patients who develop acute renal failure must discontinue dabigatran etexilate (see also section 4.3). When severe bleedings occur, treatment must be discontinued, the source of bleeding investigated and use of the specific reversal agent (idarucizumab) may be considered in adult patients. Haemodialysis can remove dabigatran. Use of proton-pump inhibitors The administration of a proton-pump inhibitor (PPI) can be considered to prevent GI bleeding. Laboratory coagulation parameters Although this medicinal product does not in general require routine anticoagulant monitoring, the measurement of dabigatran related anticoagulation may be helpful to detect excessive high exposure to dabigatran in the presence of additional risk factors. Diluted thrombin time (dTT), ecarin clotting time (ECT) and activated partial thromboplastin time (aPTT) may provide useful information, but results should be interpreted with caution due to inter-test variability (see section 5.1).The International Normalised Ratio (INR) test is unreliable in patients on Pradaxa and false positive INR elevations have been reported. Therefore INR tests should not be performed.Table 3 shows coagulation test thresholds at trough that may be associated with an increased risk of bleeding (see section 5.1) Table 3: Coagulation test thresholds at trough for adult patients that may be associated with an increased risk of bleeding. Test (trough value) Threshold dTT [ng/mL] >67 ECT [x-fold upper limit of normal] No data aPTT [x-fold upper limit of normal] >1.3 INR Should not be performed Use of fibrinolytic medicinal products for the treatment of acute ischemic stroke Pradaxa 75 Prescribing Information Boehringer Ingelheim January 2022 The use of fibrinolytic medicinal products for the treatment of acute ischemic stroke may be considered if the patient presents with a dTT, ECT or aPTT not exceeding the upper limit of normal (ULN) according to the local reference range. Surgery and interventions Patients on dabigatran etexilate who undergo surgery or invasive procedures are at increased risk for bleeding. Therefore, surgical interventions may require the temporary discontinuation of dabigatran etexilate. Caution should be exercised when treatment is temporarily discontinued for interventions and anticoagulant monitoring is warranted. Clearance of dabigatran in patients with renal insufficiency may take longer (see section 5.2). This should be considered in advance of any procedures. In such cases a coagulation test (see sections 4.4 and 5.1) may help to determine whether haemostasis is still impaired. Emergency surgery or urgent procedures Dabigatran etexilate should be temporarily discontinued. When rapid reversal of the anticoagulation effect is required the specific reversal agent (idarucizumab) to dabigatran is available for adult patients. Reversing dabigatran therapy exposes patients to the thrombotic risk of their underlying disease. Dabigatran etexilate treatment can be re-initiated 24 hours after administration of idarucizumab, if the patient is clinically stable and adequate haemostasis has been achieved. Subacute surgery/interventions Dabigatran etexilate should be temporarily discontinued. A surgery / intervention should be delayed if possible until at least 12 hours after the last dose. If surgery cannot be delayed the risk of bleeding may be increased. This risk of bleeding should be weighed against the urgency of intervention. Elective surgery If possible, dabigatran etexilate should be discontinued at least 24 hours before invasive or surgical procedures. In patients at higher risk of bleeding or in major surgery where complete haemostasis may be required consider stopping dabigatran etexilate 2-4 days before surgery. Table 4 summarises discontinuation rules before invasive or surgical procedures for adult patients. Table 4: Discontinuation rules before invasive or surgical procedures for adult patients Renal function Estimated half-life Dabigatran etexilate should be stopped before elective (CrCL in (hours) surgery mL/min) High risk of bleeding or Standard risk major surgery ≥80 ~ 13 2 days before 24 hours before ≥50-<80 ~ 15 2-3 days before 1-2 days before ≥30-<50 ~ 18 4 days before 2-3 days before (>48 hours) Pradaxa 75 Prescribing Information Boehringer Ingelheim January 2022 Spinal anaesthesia/epidural anaesthesia/lumbar puncture Procedures such as spinal anaesthesia may require complete haemostatic function. The risk of spinal or epidural haematoma may be increased in cases of traumatic or repeated puncture and by the prolonged use of epidural catheters. After removal of a catheter, an interval of at least 2 hours should elapse before the administration of the first dose of dabigatran etexilate. These patients require frequent observation for neurological signs and symptoms of spinal or epidural haematoma. Postoperative phase Dabigatran etexilate should be restarted after the invasive procedure or surgical intervention as soon as possible provided the clinical situation allows and adequate haemostasis has been established. Patients at risk for bleeding or patients at risk of overexposure, notably patients with reduced renal function (see also table 2), should be treated with caution (see sections 4.4 and 5.1). Patients at high surgical mortality risk and with intrinsic risk factors for thromboembolic events There are limited efficacy and safety data for dabigatran etexilate available in these patients and therefore they should be treated with caution. Hip fracture surgery There is no data on the use of dabigatran etexilate in patients undergoing hip fracture surgery. Therefore treatment is not recommended. Hepatic impairment Patients with elevated liver enzymes >2 ULN were excluded in the main trials . No treatment experience is available for this subpopulation of patients, and therefore the use of dabigatran etexilate is not recommended in this population. Hepatic impairment or liver disease expected to have any impact on survival is contraindicated (see section 4.3). Interaction with P-gp inducers Concomitant administration of P-gp inducers is expected to result in decreased dabigatran plasma concentrations, and should be avoided (see sections 4.5 and 5.2). Patients with antiphospholipid syndrome Direct acting Oral Anticoagulants (DOACs) including dabigatran etexilate are not recommended for patients with a history of thrombosis who are diagnosed with antiphospholipid syndrome. In particular for patients that are triple positive (for lupus anticoagulant, anticardiolipin antibodies, and anti–beta 2-glycoprotein I antibodies), treatment with DOACs could be associated with increased rates of recurrent thrombotic events compared with vitamin K antagonist therapy. Pradaxa 75 Prescribing Information Boehringer Ingelheim January 2022
Effects on Driving
4.7 Effects on ability to drive and use machines Dabigatran etexilate has no or negligible influence on the ability to drive and use machines.

פרטי מסגרת הכללה בסל
התרופה תינתן לטיפול במקרים האלה: 1. מניעת תרומבואמבוליזם לאחר ניתוח להחלפת מפרק הירך; 2. מניעת תרומבואמבוליזם לאחר ניתוח להחלפת הברך; 3.מניעת שבץ ותסחיף סיסטמי בחולים עם פרפור עליות המטופלים ב-warfarin וחוו CVA או TIA עם ביטוי קליני (שטופל או אובחן בבית חולים) במהלך השנה האחרונה; 4. מניעת שבץ ותסחיף סיסטמי בחולים עם פרפור עליות המטופלים ב-Warfarin ושתועד אצלם INR גבוה מ-5 לפחות פעמיים במהלך השנה האחרונה באירועים נפרדים; 5. מניעת שבץ ותסחיף סיסטמי בחולים עם פרפור עליות ללא מחלה מסתמית ו-CHA2DS2 VASc score בערך 2 ומעלה.6. טיפול קצר טווח למניעת שבץ ותסחיף סיסטמי בחולים עם פרפור עליות בלא מחלה מסתמית ו-CHADS2 score בערך 0 או 1 אחרי היפוך קצב ופעולות של אבלציות בפרפור.7. טיפול ומניעה שניונית של פקקת הורידים העמוקים (Deep vein thrombosis – DVT).8. טיפול ומניעה שניונית של תסחיף ריאתי (Pulmonary embolism - PE).
מסגרת הכללה בסל
התוויות הכלולות במסגרת הסל
| התוויה | תאריך הכללה | תחום קליני | Class Effect | מצב מחלה |
|---|---|---|---|---|
| טיפול ומניעה שניונית של פקקת הורידים העמוקים (Deep vein thrombosis – DVT). | 11/01/2018 | המטולוגיה | DABIGATRAN ETEXILATE, RIVAROXABAN, EDOXABAN, APIXABAN | |
| טיפול קצר טווח למניעת שבץ ותסחיף סיסטמי בחולים עם פרפור עליות בלא מחלה מסתמית ו-CHADS2 score בערך 0 או 1 אחרי היפוך קצב ופעולות של אבלציות בפרפור | 11/01/2018 | המטולוגיה | DABIGATRAN ETEXILATE, RIVAROXABAN, EDOXABAN, APIXABAN | |
| . מניעת שבץ ותסחיף סיסטמי בחולים עם פרפור עליות בלא מחלה מסתמית ו-CHA2DS2 score בערך 2 ומעלה. | 21/01/2016 | המטולוגיה | DABIGATRAN ETEXILATE, RIVAROXABAN, EDOXABAN, APIXABAN | |
| מניעת שבץ ותסחיף סיסטמי בחולים עם פרפור עליות בלא מחלה מסתמית ו-CHA2DS2 VASc score בערך 2 ומעלה. | 16/01/2019 | המטולוגיה | DABIGATRAN ETEXILATE, RIVAROXABAN, EDOXABAN, APIXABAN | |
| טיפול ומניעה שניונית של תסחיף ריאתי (Pulmonary embolism - PE). | 11/01/2018 | המטולוגיה | DABIGATRAN ETEXILATE, RIVAROXABAN, EDOXABAN, APIXABAN | |
| . מניעת שבץ ותסחיף סיסטמי בחולים עם פרפור עליות בלא מחלה מסתמית ו-CHA2DS2 score בערך 3 ומעלה. | 12/01/2014 | המטולוגיה | DABIGATRAN ETEXILATE, RIVAROXABAN, EDOXABAN, APIXABAN | |
| . מניעת שבץ ותסחיף סיסטמי בחולים עם פרפור עליות בלא מחלה מסתמית ו-CHA2DS2 score בערך 4 ומעלה. | 10/01/2012 | המטולוגיה | DABIGATRAN ETEXILATE, RIVAROXABAN, EDOXABAN, APIXABAN | |
| מניעת שבץ ותסחיף סיסטמי בחולים עם פרפור עליות המטופלים ב-Warfarin ושתועד אצלם INR גבוה מ-5 לפחות פעמיים במהלך השנה האחרונה באירועים נפרדים. | 23/01/2011 | המטולוגיה | DABIGATRAN ETEXILATE, RIVAROXABAN, EDOXABAN, APIXABAN | |
| מניעת שבץ ותסחיף סיסטמי בחולים עם פרפור עליות המטופלים ב-warfarin וחוו CVA או TIA עם ביטוי קליני (שטופל או אובחן בבית חולים) במהלך השנה האחרונה. | 23/01/2011 | המטולוגיה | DABIGATRAN ETEXILATE, RIVAROXABAN, APIXABAN | |
| מניעת תרומבואמבוליזם לאחר ניתוח להחלפת הברך. | 03/01/2010 | אורתופדיה | DABIGATRAN ETEXILATE, RIVAROXABAN, APIXABAN | |
| מניעת תרומבואמבוליזם לאחר ניתוח להחלפת מפרק הירך | 03/01/2010 | אורתופדיה | DABIGATRAN ETEXILATE, RIVAROXABAN, APIXABAN |
שימוש לפי פנקס קופ''ח כללית 1994
לא צוין
תאריך הכללה מקורי בסל
03/01/2010
הגבלות
תרופה מוגבלת לרישום ע'י רופא מומחה או הגבלה אחרת
מידע נוסף
עלון מידע לרופא
28.02.22 - עלון לרופאעלון מידע לצרכן
10.11.13 - עלון לצרכן 03.10.19 - עלון לצרכן עברית 03.10.19 - עלון לצרכן ערבית 03.10.19 - עלון לצרכן ערבית 03.10.19 - עלון לצרכן 05.08.20 - עלון לצרכן אנגלית 02.06.19 - עלון לצרכן עברית 05.08.20 - עלון לצרכן עברית 05.08.20 - עלון לצרכן ערבית 30.11.11 - החמרה לעלון 26.07.12 - החמרה לעלון 25.12.12 - החמרה לעלון 12.07.15 - החמרה לעלון 17.01.17 - החמרה לעלון 02.06.19 - החמרה לעלון 01.09.19 - החמרה לעלון 05.08.20 - החמרה לעלון 05.08.20 - החמרה לעלון 28.02.22 - החמרה לעלוןלתרופה במאגר משרד הבריאות
פרדקסה 75