Quest for the right Drug
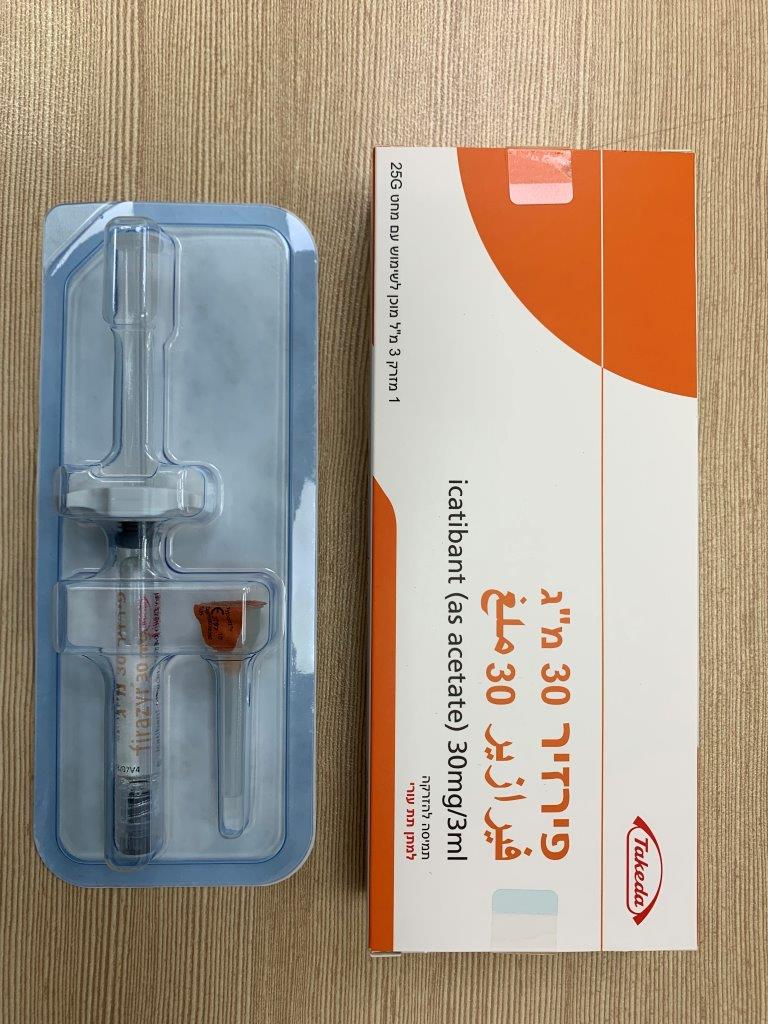
פירזיר 30 מ"ג FIRAZYR 30 MG (ICATIBANT AS ACETATE)
תרופה במרשם
תרופה בסל
נרקוטיקה
ציטוטוקסיקה
צורת מתן:
תת-עורי : S.C
צורת מינון:
תמיסה להזרקה : SOLUTION FOR INJECTION
עלון לרופא
מינוניםPosology התוויות
Indications תופעות לוואי
Adverse reactions התוויות נגד
Contraindications אינטראקציות
Interactions מינון יתר
Overdose הריון/הנקה
Pregnancy & Lactation אוכלוסיות מיוחדות
Special populations תכונות פרמקולוגיות
Pharmacological properties מידע רוקחי
Pharmaceutical particulars אזהרת שימוש
Special Warning עלון לרופא
Physicians Leaflet
Pharmacological properties : תכונות פרמקולוגיות
Pharmacodynamic Properties
5.1 Pharmacodynamic properties Pharmacotherapeutic group: Other haematological agents, drugs used to treat hereditary angioedema; ATC code: B06AC02. Mechanism of action HAE (an autosomal dominant disease) is caused by an absence or dysfunction of C1- esterase-inhibitor. HAE attacks are accompanied by an increased release of bradykinin, which is the key mediator in the development of the clinical symptoms. HAE manifests as intermittent attacks of subcutaneous and/or sub mucosal oedema involving the upper respiratory tract, the skin and the gastrointestinal tract. An attack usually lasts between 2 to 5 days. Icatibant is a selective competitive antagonist at the bradykinin type 2 (B2) receptor. It is a synthetic decapeptide with a structure similar to bradykinin, but with 5 non-proteinogenic amino acids. In HAE increased bradykinin concentrations are the key mediator in the development of the clinical symptoms. Pharmacodynamic effects In healthy young subjects, icatibant administered in doses of 0.8 mg/kg over 4 hours; 1.5 mg/kg/day or 0.15 mg/kg/day for 3 days, development of bradykinin-induced hypotension, vasodilatation and reflex tachycardia was prevented. Icatibant was shown to be a competitive antagonist when the bradykinin challenge dose was increased 4-fold. Clinical efficacy and safety Efficacy data were obtained from an initial open-label Phase II study and from three controlled Phase III studies. Phase III clinical studies (FAST-1 and FAST-2) were randomized, double-blind, controlled trials and had identical designs except for the comparator (one with oral tranexamic acid as the comparator and one placebo controlled). A total of 130 patients were randomized to receive either a 30 mg dose of icatibant (63 patients) or comparator (either tranexamic acid, - 38 or placebo - 29 patients). Subsequent episodes of HAE were treated in an open label extension. Patients with symptoms of laryngeal angioedema received open label treatment with icatibant. The primary efficacy endpoint was the time to onset of symptom relief using a visual analogue scale (VAS). Table 3 shows the efficacy results for these studies. FAST-3 was a randomized, placebo-controlled, parallel-group study of 98 adult patients with a median age of 36 years. Patients were randomized to receive either icatibant 30 mg or placebo by subcutaneous injection. A subset of patients in this study experienced acute HAE attacks while receiving androgens, antifibrinolytic agents or Cl inhibitors. The primary endpoint was time to onset of symptom relief assessed using a 3-item composite visual analog score (VAS-3) consisting of assessments of skin swelling, skin pain, and abdominal pain. Table 3 shows the efficacy results for FAST-3. In these studies, patients on icatibant had a faster median time to onset of symptom relief (2.0, 2.5 and 2.0 hours, respectively) compared to tranexamic acid (12.0 hours) and placebo (4.6 and 19.8 hours). The treatment effect of icatibant was confirmed by secondary efficacy endpoints. In an integrated analysis of these controlled Phase III studies, the time to onset of symptom relief and time to onset of primary symptom relief were similar regardless of age group, sex, race, weight or whether or not the patient used androgens or antifibrinolytic agents. Response was also consistent across repeated attacks in the controlled Phase III trials. A total of 237 patients were treated with 1,386 doses of 30 mg icatibant for 1,278 attacks of acute HAE. In the first 15 Firazyr treated attacks (1,114 doses for 1,030 attacks), the median times to onset of symptom relief were similar across attacks (2.0 to 2.5 hours). 92.4% of these attacks of HAE were treated with a single dose of Firazyr. Table 3. Efficacy results for FAST-1 and FAST-2 Controlled Clinical Study of FIRAZYR vs Tranexamic acid or Placebo: Efficacy Results FAST-2 FAST-1 Tranexamic Icatibant Icatibant Placebo acid Number of Number of subjects in ITT 36 38 subjects in ITT 27 29 Population Population Controlled Clinical Study of FIRAZYR vs Tranexamic acid or Placebo: Efficacy Results FAST-2 FAST-1 Tranexamic Icatibant Icatibant Placebo acid Baseline Baseline 63.7 61.5 69.3 67.7 VAS(mm) VAS(mm) Change from Change from baseline to -41.6 -14.6 baseline to -44.8 -23.5 4 hours 4 hours Difference Difference between -27.8 (-39.4, -16.2) between -23.3 (-37.1, -9.4) p = 0.002 treatments (95% p < 0.001 treatments (95% CI, p-value) CI, p-value) Change from Change from baseline to -54.0 -30.3 baseline to -54.2 -42.4 12 hours 12 hours Difference Difference between -24.1 (-33.6, -14.6) between -15.2 (-28.6, -1.7) p = 0.028 treatments (95% p < 0.001 treatments (95% CI, p-value) CI, p-value) Median time to Median time to onset of onset of symptom relief symptom relief (hours) (hours) All episodes All episodes 2.0 12.0 2.5 4.6 (N = 74) (N = 56) Response rate Response rate (%, CI) at 4 hours (%, CI) at 4 hours after start of after start of treatment treatment All episodes 80.0 30.6 All episodes 66.7 46.4 (N = 74) (63.1, 91.6) (16.3, 48.1) (N = 56) (46.0, 83.5) (27.5, 66.1) Median time to Median time to onset of onset of symptom relief: symptom relief: all symptoms all symptoms (hours): 1.6 3.5 (hours): 2.0 3.3 Abdominal 2.6 18.1 Abdominal 3.1 10.2 pain 1.5 12.0 pain 1.6 9.0 Skin swelling Skin swelling Skin pain Skin pain Median time to Median time to almost complete almost complete symptom relief symptom relief (hours) (hours) All episodes All episodes 10.0 51.0 8.5 19.4 (N = 74) (N = 56) Median time to Median time to regression of regression of symptoms, by symptoms, by patient (hours) patient (hours) All episodes All episodes 0.8 7.9 0.8 16.9 (N = 74) (N = 56) Controlled Clinical Study of FIRAZYR vs Tranexamic acid or Placebo: Efficacy Results FAST-2 FAST-1 Tranexamic Icatibant Icatibant Placebo acid Median time to Median time to overall patient overall patient improvement, by improvement, by physician (hours) physician (hours) All episodes All episodes 1.5 6.9 1.0 5.7 (N = 74) (N = 56) Table 4. Efficacy results for FAST-3 Efficacy Results: FAST-3; Controlled Phase -- ITT population Endpoint Statistic Firazyr Placebo p-value (n = 43) (n=45) Primary Endpoint Time to Onset of Symptom Median 2.0 19.8 <0.001 Relief-- Composite VAS (hrs) Other Endpoints Time to Onset of Primary Median 1.5 18.5 < 0.001 Symptom Relief (hrs) Change in Composite VAS Mean -19.74 -7.49 < 0.001 Score at 2 hrs after treatment Change in Composite Mean -0.53 -0.22 < 0.001 Subject-Assessed Symptom Score at 2 hours Change in Composite Mean -0.44 -0.19 < 0.001 Investigator-Assessed Symptom Score at 2 hours Time to Almost Complete Median 8.0 36.0 0.012 Symptom Relief (hrs) Time to Subject-Assessed Median 0.8 3.5 < 0.001 Initial Symptom Improvement (hrs) Time to Investigator- Median 0.8 3.4 < 0.001 Assessed Initial Visual Symptom Improvement (hrs) A total of 66 patients with attacks of HAE affecting the larynx were treated in these controlled Phase III clinical trials. The results were similar to patients with non-laryngeal attacks of HAE with respect to time to onset of symptom relief. Paediatric population An open label, non-randomised single-arm study (HGT-FIR-086) was performed with a total of 32 patients. All patients received at least one dose of icatibant (0.4mg/kg body weight up to a maximum dose of 30 mg) and the majority of patients were followed up for a minimum of 6 months. Eleven patients were of prepubertal status and 21 patients were either pubertal or postpubertal. The efficacy population consisted of 22 patients who had been treated with icatibant (11 prepubertal and 11 pubertal/postpubertal) for HAE attack. The primary efficacy endpoint was the time to onset of symptom relief (TOSR) measured using a composite investigator-reported symptom score. Time to symptom relief was defined as the duration of time (in hours) taken for improvement of symptoms to occur by a magnitude of 20%. Overall the median time to onset of symptom relief was 1.0 hour (95% confidence interval, 1.0-1.1 hours). At 1 and 2 hours post treatment, approximately 50% and 90% of patients experienced onset of symptom relief, respectively. Overall, the median time to minimal symptoms (earliest time post treatment when all symptoms were either mild or absent) was 1.1 hours (95% confidence interval, 1.0-2.0 hours).
Pharmacokinetic Properties
5.2 Pharmacokinetic properties The pharmacokinetics of icatibant has been characterized by studies using both intravenous and subcutaneous administration to healthy volunteers and patients. The pharmacokinetic profile of icatibant in patients with HAE is similar to that in healthy volunteers. Absorption Following subcutaneous administration, the absolute bioavailability of icatibant is 97%. The time to maximum concentration is approximately 30 minutes. Distribution Icatibant volume of distribution (Vss) is about 20-25 L. Plasma protein binding is 44%. Biotransformation Icatibant is extensively metabolized by proteolytic enzymes to inactive metabolites that are primarily excreted in the urine. In vitro studies have confirmed that icatibant is not degraded by oxidative metabolic pathways and is not an inhibitor of major cytochrome P450 (CYP) isoenzymes (CYP 1A2, 2A6, 2B6, 2C8, 2C9, 2C19, 2D6, 2E1, and 3A4) and is not an inducer of CYP 1A2 and 3A4. Elimination Icatibant is mainly eliminated by metabolism with less than 10% of the dose eliminated in the urine as unchanged drug. Clearance is about 15-20 l/h and independent of dose. The terminal plasma half-life is about 1-2 hours. Special populations Elderly Data suggest an age-related decline in clearance resulting in about 50-60% higher exposure in older people (75-80 years) compared to patients aged 40 years. Gender Data suggest that there is no difference in the clearance between females and males after correcting for body weight. Hepatic and Renal Impairment Limited data suggest that icatibant exposure is not influenced by hepatic or renal impairment. Race Information on individual race effect is limited. Available exposure data suggest no difference in the clearance between non-White (n=40) and White (n=132) subjects. Paediatric population The pharmacokinetics of icatibant were characterized in paediatric HAE patients in study HGT-FIR- 086 (see section 5.1). Following a single subcutaneous administration (0.4 mg/kg up to a maximum of 30 mg), the time to maximum concentration is approximately 30 minutes and the terminal half-life is about 2 hours. There are no observed differences in the exposure to icatibant between HAE patients with and without an attack. Population pharmacokinetic modelling using both adult and paediatric data showed that clearance of icatibant is related to body weight with lower clearance values noted for lower body weights in the paediatric HAE population. Based on modelling for weight banded dosing, the predicted exposure to icatibant in the paediatric HAE population (see section 4.2) is lower than the observed exposure in studies conducted with adult HAE patients.

פרטי מסגרת הכללה בסל
התרופה תינתן לטיפול סימפטומטי בהתקפים חריפים של אנגיואדמה תורשתית בחולים עם חסר ב-C1 esterase inhibitor בהתאם למפורט להלן: א. החולה מצוי בטיפול ומעקב של מרפאה לאימונולוגיה קלינית; ב. החולה סובל מהתקפים חוזרים של כאבי בטן חזקים או התקפים חוזרים של היצרות לרינקס; ג. הטיפול יינתן באישור מומחה באלרגיה ואימונולוגיה המטפל בחולה במסגרת מרפאה לאימונולוגיה קלינית. ד. לא יינתנו לחולה באותו התקף שתי התרופות – CONESTAT ALFA, ICATIBANT, C1 ESTERASE INHIBITOR, HUMAN.
מסגרת הכללה בסל
התוויות הכלולות במסגרת הסל
| התוויה | תאריך הכללה | תחום קליני | Class Effect | מצב מחלה |
|---|---|---|---|---|
| התרופה תינתן לטיפול סימפטומטי בהתקפים חריפים של אנגיואדמה תורשתית בחולים עם חסר ב-C1 esterase inhibitor |
שימוש לפי פנקס קופ''ח כללית 1994
לא צוין
תאריך הכללה מקורי בסל
03/01/2010
הגבלות
תרופה מוגבלת לרישום ע'י רופא מומחה או הגבלה אחרת
מידע נוסף
