Quest for the right Drug
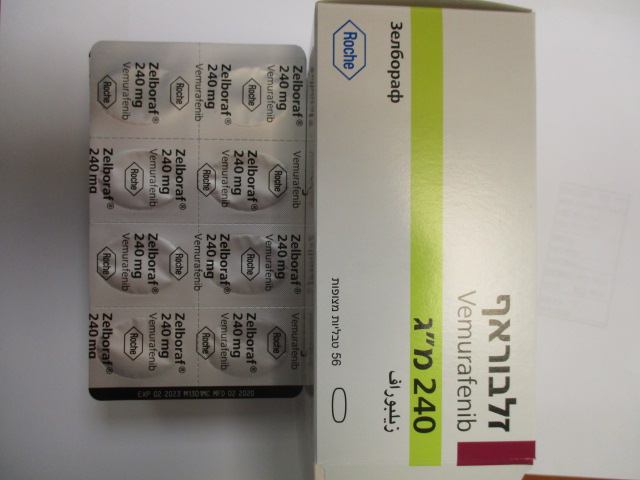
זלבוראף ZELBORAF (VEMURAFENIB)
תרופה במרשם
תרופה בסל
נרקוטיקה
ציטוטוקסיקה
צורת מתן:
פומי : PER OS
צורת מינון:
טבליות מצופות פילם : FILM COATED TABLETS
עלון לרופא
מינוניםPosology התוויות
Indications תופעות לוואי
Adverse reactions התוויות נגד
Contraindications אינטראקציות
Interactions מינון יתר
Overdose הריון/הנקה
Pregnancy & Lactation אוכלוסיות מיוחדות
Special populations תכונות פרמקולוגיות
Pharmacological properties מידע רוקחי
Pharmaceutical particulars אזהרת שימוש
Special Warning עלון לרופא
Physicians Leaflet
Special Warning : אזהרת שימוש
4.4 Special warnings and precautions for use Before taking vemurafenib, patients must have BRAF V600 mutation-positive tumour status confirmed by a validated test. The efficacy and safety of vemurafenib in patients with tumours expressing rare BRAF V600 mutations other than V600E and V600K have not been convincingly established (see section 5.1). Vemurafenib should not be used in patients with wild type BRAF malignant melanoma. Hypersensitivity reaction Serious hypersensitivity reactions, including anaphylaxis have been reported in association with vemurafenib (see sections 4.3 and 4.8). Severe hypersensitivity reactions may include Stevens-Johnson syndrome, generalised rash, erythema or hypotension. In patients who experience severe hypersensitivity reactions, vemurafenib treatment should be permanently discontinued. Dermatologic reactions Severe dermatologic reactions have been reported in patients receiving vemurafenib, including rare cases of Stevens-Johnson syndrome and toxic epidermal necrolysis in the pivotal clinical trial. Drug reaction with eosinophilia and systemic symptoms (DRESS) has been reported in association with vemurafenib in the post-marketing setting (see section 4.8). In patients who experience a severe dermatologic reaction, vemurafenib treatment should be permanently discontinued. Potentiation of radiation toxicity Cases of radiation recall and radiation sensitization have been reported in patients treated with radiation either prior, during, or subsequent to vemurafenib treatment. Most cases were cutaneous in nature but some cases involving visceral organs had fatal outcomes (see sections 4.5 and 4.8). Vemurafenib should be used with caution when given concomitantly or sequentially with radiation treatment. QT prolongation Exposure-dependent QT prolongation was observed in an uncontrolled, open-label phase II study in previously treated patients with metastatic melanoma (see section 4.8). QT prolongation may lead to an increased risk of ventricular arrhythmias including Torsade de Pointes. Treatment with vemurafenib is not recommended in patients with uncorrectable electrolyte abnormalities (including magnesium), long QT syndrome or who are taking medicinal products known to prolong the QT interval. Electrocardiogram (ECG) and electrolytes (including magnesium) must be monitored in all patients before treatment with vemurafenib, after one month of treatment and after dose modification. Further monitoring is recommended in particular in patients with moderate to severe hepatic impairment monthly during the first 3 months of treatment followed by every 3 months thereafter or more often as clinically indicated. Initiation of treatment with vemurafenib is not recommended in patients with QTc>500 milliseconds (ms). If during treatment the QTc exceeds 500 ms, vemurafenib treatment should be temporarily interrupted, electrolyte abnormalities (including magnesium) should be corrected, and cardiac risk factors for QT prolongation (e.g. congestive heart failure, bradyarrhythmias) should be controlled. Re-initiation of treatment should occur once the QTc decreases below 500 ms and at a lower dose as described in table 2. Permanent discontinuation of vemurafenib treatment is recommended if the QTc increase meets values of both >500 ms and >60 ms change from pre-treatment values. Ophthalmologic reactions Serious ophthalmologic reactions, including uveitis, iritis and retinal vein occlusion, have been reported. Monitor patients routinely for ophthalmologic reactions. Cutaneous Squamous Cell Carcinoma (cuSCC) Cases of cuSCC (which include those classified as keratoacanthoma or mixed keratoacanthoma subtype) have been reported in patients treated with vemurafenib (see section 4.8). It is recommended that all patients receive a dermatologic evaluation prior to initiation of therapy and be monitored routinely while on therapy. Any suspicious skin lesions should be excised, sent for dermatopathologic evaluation and treated as per local standard of care. The prescriber should examine the patient monthly during and up to six months after treatment for cuSCC. In patients who develop cuSCC, it is recommended to continue the treatment without dose adjustment. Monitoring should continue for 6 months following discontinuation of vemurafenib or until initiation of another anti-neoplastic therapy. Patients should be instructed to inform their physicians upon the occurrence of any skin changes. Non-Cutaneous Squamous Cell Carcinoma (non-cuSCC) Cases of non-cuSCC have been reported in clinical trials where patients received vemurafenib. Patients should undergo a head and neck examination, consisting of at least a visual inspection of oral mucosa and lymph node palpation prior to initiation of treatment and every 3 months during treatment. In addition, patients should undergo a chest Computerised Tomography (CT) scan, prior to treatment and every 6 months during treatment. Anal examinations and pelvic examinations (for women) are recommended before and at the end of treatment or when considered clinically indicated. Following discontinuation of vemurafenib, monitoring for non-cuSCC should continue for up to 6 months or until initiation of another anti-neoplastic therapy. Abnormal findings should be managed according to clinical practices. New primary melanoma New primary melanomas have been reported in clinical trials. Cases were managed with excision and patients continued treatment without dose adjustment. Monitoring for skin lesions should occur as outlined above for cutaneous squamous cell carcinoma. Other malignancies Based on mechanism of action, vemurafenib may cause progression of cancers associated with RAS mutations (see section 4.8). Carefully consider benefits and risks before administering vemurafenib to patients with a prior or concurrent cancer associated with RAS mutation. Pancreatitis Pancreatitis has been reported in vemurafenib-treated subjects. Unexplained abdominal pain should be promptly investigated (including measurement of serum amylase and lipase). Patients should be closely monitored when re-starting vemurafenib after an episode of pancreatitis. Liver injury Liver injury, including cases of severe liver injury, has been reported with vemurafenib (see section 4.8). Liver enzymes (transaminases and alkaline phosphatase) and bilirubin should be measured before initiation of treatment and monitored monthly during treatment, or as clinically indicated. Laboratory abnormalities should be managed with dose reduction, treatment interruption or with treatment discontinuation (see sections 4.2 and 4.8). Renal toxicity Renal toxicity, ranging from serum creatinine elevations to acute interstitial nephritis and acute tubular necrosis, has been reported with vemurafenib. Serum creatinine should be measured before initiation of treatment and monitored during treatment as clinically indicated (see sections 4.2 and 4.8). Hepatic impairment No adjustment to the starting dose is needed for patients with hepatic impairment. Patients with mild hepatic impairment due to liver metastases without hyperbilirubinaemia may be monitored according to the general recommendations. There are only very limited data available in patients with moderate to severe hepatic impairment. Patients with moderate to severe hepatic impairment may have increased exposure (see section 5.2). Thus close monitoring is warranted especially after the first few weeks of treatment as accumulation may occur over an extended period of time (several weeks). In addition ECG monitoring every month during the first three months is recommended. Renal impairment No adjustment to the starting dose is needed for patients with mild or moderate renal impairment. There are only limited data available in patients with severe renal impairment (see section 5.2). Vemurafenib should be used with caution in patients with severe renal impairment and patients should be closely monitored. Photosensitivity Mild to severe photosensitivity was reported in patients who received vemurafenib in clinical studies (see section 4.8). All patients should be advised to avoid sun exposure while taking vemurafenib. While taking the medicinal product, patients should be advised to wear protective clothing and use a broad spectrum Ultraviolet A (UVA)/Ultraviolet B (UVB) sunscreen and lip balm (Sun Protection Factor ≥ 30) when outdoors to help protect against sunburn. For photosensitivity grade 2 (intolerable) or greater, dose modifications are recommended (see section 4.2). Dupuytren’s contracture and plantar fascial fibromatosis Dupuytren’s contracture and plantar fascial fibromatosis have been reported with vemurafenib. The majority of cases were mild to moderate, but severe, disabling cases of Dupuytren’s contracture have also been reported (see section 4.8). Events should be managed with dose reduction with treatment interruption or with treatment discontinuation (see section 4.2). Effects of vemurafenib on other medicinal products Vemurafenib may increase the plasma exposure of medicinal products predominantly metabolised by CYP1A2 and decrease the plasma exposure of medicines predominantly metabolised by CYP3A4. Concomitant use of vemurafenib with agents metabolized by CYP1A2 and CYP3A4 with narrow therapeutic windows is not recommended. Dose adjustments for medicinal products predominantly metabolised via CYP1A2 or CYP3A4 should be considered based on their therapeutic windows before concomitantly treating with vemurafenib (see sections 4.5 and 4.6). Exercise caution and consider additional INR (International Normalised Ratio) monitoring when vemurafenib is used concomitantly with warfarin. Vemurafenib may increase the plasma exposure of medicinal products that are P-gp substrates. Caution should be exercised when dosing vemurafenib concurrently with P-gp substrates. Dose reduction and/or additional drug level monitoring for P-gp substrate medicinal products with narrow therapeutic index (NTI) (e.g. digoxin, dabigatran etexilate, aliskiren) may be considered if these medicinal products are used concomitantly with vemurafenib (see section 4.5). Effect of other medicinal products on vemurafenib Concomitant administration of strong inducers of CYP3A4, P-gp and glucuronidation (e.g. rifampicin, rifabutin, carbamazepine, phenytoin or St John’s Wort [hypericin]) might lead to decreased exposure of vemurafenib and should be avoided when possible (see section 4.5). Alternative treatment with less inducing potential should be considered to maintain the efficacy of vemurafenib. Caution should be used when administering Vemurafenib with strong CYP3A4/PgP inhibitors. Patients should be carefully monitored for safety and dose modifications applied if clinically indicated (see Table 1 in section 4.2). Concurrent administration with ipilimumab In a Phase I trial, asymptomatic grade 3 increases in transaminases (ALT/AST >5 x ULN) and bilirubin (total bilirubin >3x ULN) were reported with concurrent administration of ipilimumab (3 mg/kg) and vemurafenib (960 mg BID or 720 mg BID). Based on these preliminary data, the concurrent administration of ipilimumab and vemurafenib is not recommended.
Effects on Driving
4.7 Effects on ability to drive and use machines Vemurafenib has minor influence on the ability to drive and use machines. Patients should be made aware of the potential fatigue or eye problems that could be a reason for not driving.

פרטי מסגרת הכללה בסל
א. התרופה תינתן לטיפול בחולי מלנומה מתקדמת (גרורתית או שאיננה נתיחה) המבטאים מוטציה ב-BRAF. ב. במהלך מחלתו יהיה החולה זכאי לטיפול בתרופה אחת בלבד מהתרופות המפורטות להלן – Encorafenib, Dabrafenib, Vemurafenibלעניין זה מלנומה בשלב מתקדם (לא נתיח או גרורתי) לא תוגדר כאותה מחלה כמו מלנומה בשלב בר הסרה בניתוח.ג. מתן התרופה האמורה ייעשה לפי מרשם של מומחה באונקולוגיה.
מסגרת הכללה בסל
התוויות הכלולות במסגרת הסל
| התוויה | תאריך הכללה | תחום קליני | Class Effect | מצב מחלה |
|---|---|---|---|---|
| התרופה תינתן לטיפול בחולי מלנומה מתקדמת (גרורתית או שאיננה נתיחה) המבטאים מוטציה ב-BRAF. |
שימוש לפי פנקס קופ''ח כללית 1994
לא צוין
תאריך הכללה מקורי בסל
10/01/2012
הגבלות
תרופה מוגבלת לרישום ע'י רופא מומחה או הגבלה אחרת
מידע נוסף
עלון מידע לצרכן
21.08.14 - עלון לצרכן 22.04.18 - עלון לצרכן 01.05.18 - עלון לצרכן 11.02.20 - עלון לצרכן אנגלית 11.02.20 - עלון לצרכן עברית 11.02.20 - עלון לצרכן ערבית 08.08.23 - עלון לצרכן עברית 11.09.23 - עלון לצרכן אנגלית 11.09.23 - עלון לצרכן ערבית 09.04.24 - עלון לצרכן עברית 23.05.24 - עלון לצרכן אנגלית 23.05.24 - עלון לצרכן ערבית 30.05.13 - החמרה לעלון 18.07.13 - החמרה לעלון 12.02.14 - החמרה לעלון 20.03.14 - החמרה לעלון 19.10.15 - החמרה לעלון 13.12.15 - החמרה לעלון 13.07.16 - החמרה לעלון 24.05.17 - החמרה לעלון 15.11.18 - החמרה לעלון 09.01.20 - החמרה לעלון 08.08.23 - החמרה לעלון 09.04.24 - החמרה לעלוןלתרופה במאגר משרד הבריאות
זלבוראף