Quest for the right Drug
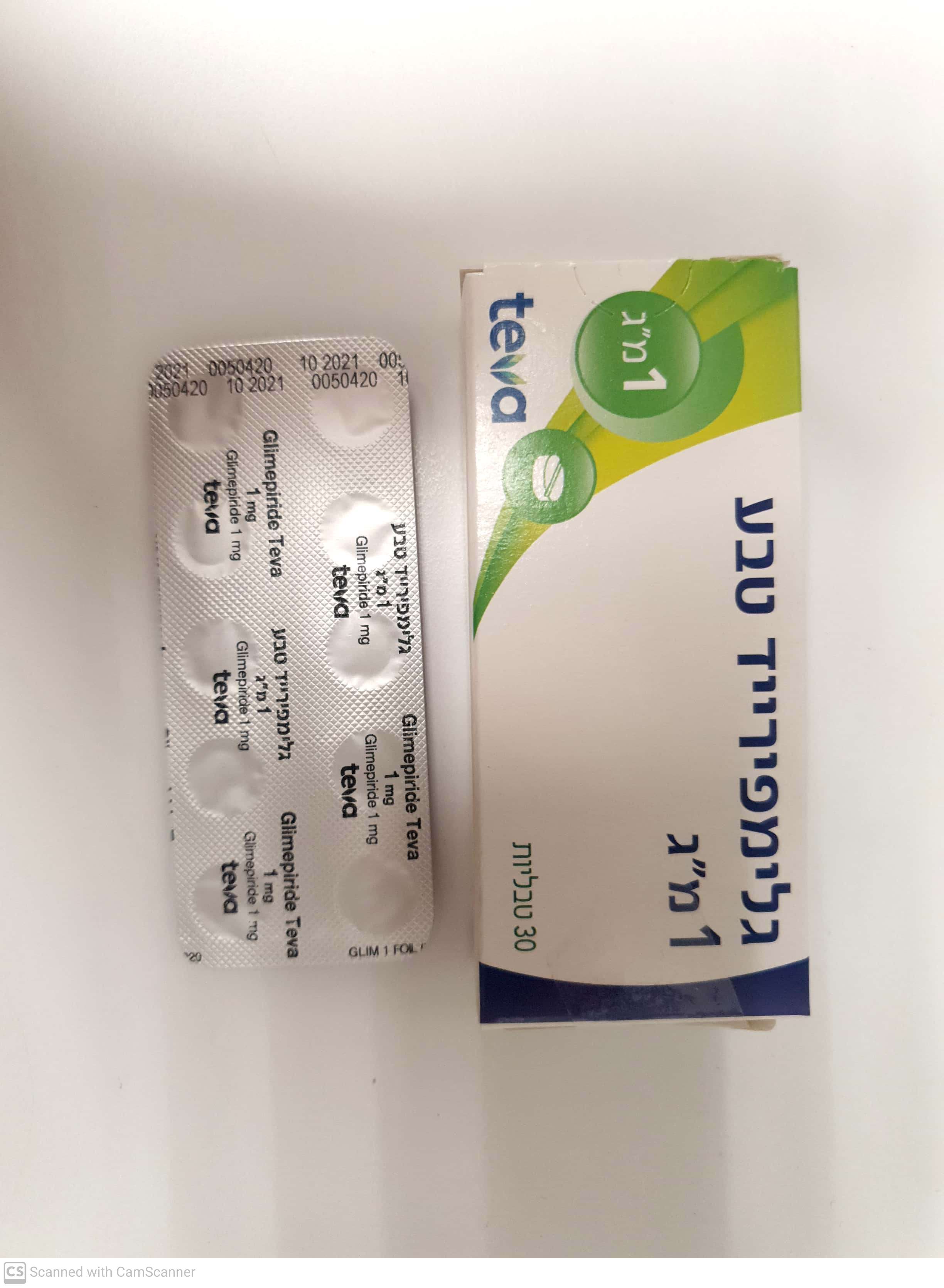
גלימפירייד טבע ® 1 מ"ג GLIMEPIRIDE TEVA ® 1 MG (GLIMEPIRIDE)
תרופה במרשם
תרופה בסל
נרקוטיקה
ציטוטוקסיקה
צורת מתן:
פומי : PER OS
צורת מינון:
טבליה : TABLETS
עלון לרופא
מינוניםPosology התוויות
Indications תופעות לוואי
Adverse reactions התוויות נגד
Contraindications אינטראקציות
Interactions מינון יתר
Overdose הריון/הנקה
Pregnancy & Lactation אוכלוסיות מיוחדות
Special populations תכונות פרמקולוגיות
Pharmacological properties מידע רוקחי
Pharmaceutical particulars אזהרת שימוש
Special Warning עלון לרופא
Physicians Leaflet
Pharmacological properties : תכונות פרמקולוגיות
Pharmacodynamic Properties
5.1 Pharmacodynamic properties Pharmacotherapeutic group: Blood glucose lowering drugs, excl. insulins: Sulfonylureas. ATC code: A10B B12 Glimepiride is an orally active hypoglycemic substance belonging to the sulfonylurea group. It may be used in non-insulin dependent diabetes mellitus. Mechanism of action Glimepiride acts mainly by stimulating insulin release from pancreatic beta cells. As with other sulfonylureas this effect is based on an increase of responsiveness of the pancreatic beta cells to the physiological glucose stimulus. In addition, glimepiride seems to have pronounced extrapancreatic effects also postulated for other sulfonylureas. Insulin release Sulfonylureas regulate insulin secretion by closing the ATP-sensitive potassium channel in the beta cell membrane. Closing the potassium channel induces depolarisation of the beta cell and results – by opening of calcium channels - in an increased influx of calcium into the cell. This leads to insulin release through exocytosis. Glimepiride binds with a high exchange rate to a beta cell membrane protein which is associated with the ATP-sensitive potassium channel but which is different from the usual sulfonylurea binding site. Extrapancreatic activity The extrapancreatic effects are for example an improvement of the sensitivity of the peripheral tissue for insulin and a decrease of the insulin uptake by the liver. The uptake of glucose from blood into peripheral muscle and fat tissues occurs via special transport proteins, located in the cell’s membrane. The transport of glucose in these tissues is the rate-limiting step in the use of glucose. Glimepiride increases very rapidly the number of active glucose transport molecules in the plasma membranes of muscle and fat cells, resulting in stimulated glucose uptake. Glimepiride increases the activity of the glycosyl-phosphatidylinositol-specific phospholipase C which may be correlated with the drug-induced lipogenesis and glycogenesis in isolated fat and muscle cells. Glimepiride inhibits the glucose production in the liver by increasing the intracellular concentration of fructose-2,6- bisphosphate, which in its turn inhibits the gluconeogenesis. General In healthy persons, the minimum effective oral dose is approximately 0.6 mg. The effect of glimepiride is dose-dependent and reproducible. The physiological response to acute physical exercise, reduction of insulin secretion, is still present under glimepiride. There was no significant difference in effect regardless of whether the medicinal product was given 30 minutes or immediately before a meal. In diabetic patients, good metabolic control over 24 hours can be achieved with a single daily dose. Although the hydroxy metabolite of glimepiride caused a small but significant decrease in serum glucose in healthy persons, it accounts for only a minor part of the total drug effect. Combination therapy with metformin Improved metabolic control for concomitant glimepiride therapy compared to metformin alone in patients not adequately controlled with the maximum dose of metformin has been shown in one study. Combination therapy with insulin Data for combination therapy with insulin are limited. In patients not adequately controlled with the maximum dose of glimepiride, concomitant insulin therapy can be initiated. In two studies, the combination achieved the same improvement in metabolic control as insulin alone. However, a lower average dose of insulin was required in combination therapy.
Pharmacokinetic Properties
5.2 Pharmacokinetic properties Absorption The bioavailability of glimepiride after oral administration is complete. Food intake has no relevant influence on absorption, only absorption rate is slightly diminished. Maximum serum concentrations (Cmax) are reached approx. 2.5 hours after oral intake (mean 0.3 μg/ml during multiple dosing of 4 mg daily) and there is a linear relationship between dose and both Cmax and AUC (area under the time/concentration curve). Distribution Glimepiride has a very low distribution volume (approx. 8.8 litres) which is roughly equal to the albumin distribution space, high protein binding (>99%), and a low clearance (approx. 48 ml/min). In animals, glimepiride is excreted in milk. Glimepiride is transferred to the placenta. Passage of the blood brain barrier is low. Biotransformation and elimination Mean dominant serum half-life, which is of relevance for the serum concentrations under multiple-dose conditions, is about 5 to 8 hours. After high doses, slightly longer half-lives were noted. After a single dose of radiolabelled glimepiride, 58% of the radioactivity was recovered in the urine, and 35% in the feces. No unchanged substance was detected in the urine. Two metabolites – most probably resulting from hepatic metabolism (major enzyme is CYP2C9) - were identified both in urine and feces: the hydroxy derivative and the carboxy derivative. After oral administration of glimepiride, the terminal half- lives of these metabolites were 3 to 6 and 5 to 6 hours respectively. Comparison of single and multiple once-daily dosing revealed no significant differences in pharmacokinetics, and the intraindividual variability was very low. There was no relevant accumulation. Special populations Pharmacokinetics were similar in males and females, as well as in young and elderly (above 65 years) patients. In patients with low creatinine clearance, there was a tendency for glimepiride clearance to increase and for average serum concentrations to decrease, most probably resulting from a more rapid elimination because of lower protein binding. Renal elimination of the two metabolites was impaired. Overall, no additional risk of accumulation is to be assumed in such patients. Pharmacokinetics in five non-diabetic patients after bile duct surgery were similar to those in healthy persons.

פרטי מסגרת הכללה בסל
התרופה תינתן לטיפול בסוכרת סוג 2.
מסגרת הכללה בסל
התוויות הכלולות במסגרת הסל
| התוויה | תאריך הכללה | תחום קליני | Class Effect | מצב מחלה |
|---|---|---|---|---|
| התרופה תינתן לטיפול בסוכרת סוג 2. |
שימוש לפי פנקס קופ''ח כללית 1994
לא צוין
תאריך הכללה מקורי בסל
15/01/2015
הגבלות
תרופה מוגבלת לרישום ע'י רופא מומחה או הגבלה אחרת
מידע נוסף
