Quest for the right Drug
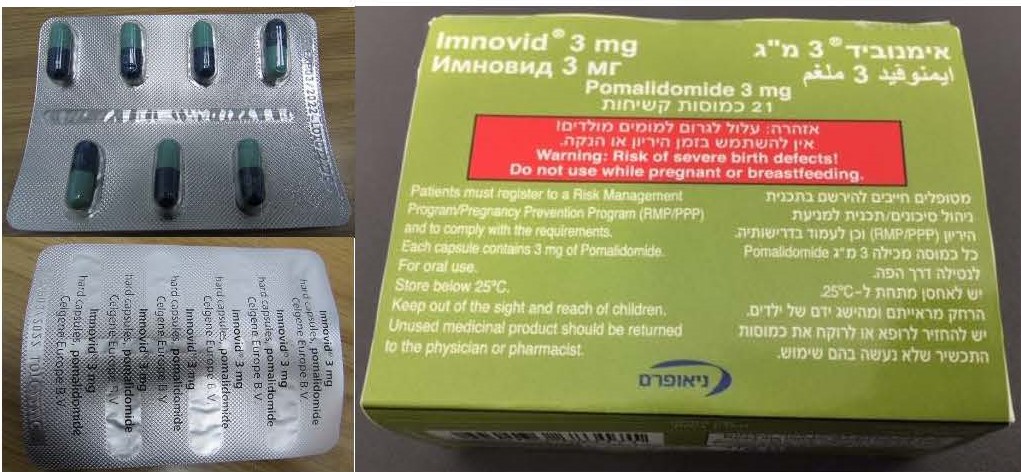
אימנוביד 3 מ"ג IMNOVID 3 MG (POMALIDOMIDE)
תרופה במרשם
תרופה בסל
נרקוטיקה
ציטוטוקסיקה
צורת מתן:
פומי : PER OS
צורת מינון:
קפסולה קשיחה : CAPSULE, HARD
עלון לרופא
מינוניםPosology התוויות
Indications תופעות לוואי
Adverse reactions התוויות נגד
Contraindications אינטראקציות
Interactions מינון יתר
Overdose הריון/הנקה
Pregnancy & Lactation אוכלוסיות מיוחדות
Special populations תכונות פרמקולוגיות
Pharmacological properties מידע רוקחי
Pharmaceutical particulars אזהרת שימוש
Special Warning עלון לרופא
Physicians Leaflet
Pharmacological properties : תכונות פרמקולוגיות
Pharmacodynamic Properties
5.1 Pharmacodynamic properties Pharmacotherapeutic group: Immunosuppressants, Other immunosuppressants, ATC code: L04AX06 Mechanism of action Pomalidomide has direct anti-myeloma tumoricidal activity, immunomodulatory activities and inhibits stromal cell support for multiple myeloma tumour cell growth. Specifically, pomalidomide inhibits proliferation and induces apoptosis of haematopoietic tumour cells. Additionally, pomalidomide inhibits the proliferation of lenalidomide-resistant multiple myeloma cell lines and synergises with dexamethasone in both lenalidomide-sensitive and lenalidomide-resistant cell lines to induce tumour cell apoptosis. Pomalidomide enhances T cell- and natural killer (NK) cell-mediated immunity and inhibits production of pro-inflammatory cytokines (e.g., TNF-α and IL-6) by monocytes. Pomalidomide also inhibits angiogenesis by blocking the migration and adhesion of endothelial cells. Pomalidomide binds directly to the protein cereblon (CRBN), which is part of an E3 ligase complex that includes deoxyribonucleic acid (DNA) damage-binding protein 1(DDB1), cullin 4 (CUL4), and regulator of cullins-1 (Roc1), and can inhibit the auto-ubiquitination of CRBN within the complex. E3 ubiquitin ligases are responsible for the poly-ubiquitination of a variety of substrate proteins, and may partially explain the pleiotropic cellular effects observed with pomalidomide treatment. In the presence of pomalidomide in vitro, substrate proteins Aiolos and Ikaros are targeted for ubiquitination and subsequent degradation leading to direct cytotoxic and immunomodulatory effects. In vivo, pomalidomide therapy led to reduction in the levels of Ikaros in patients with relapsed lenalidomide- refractory multiple myeloma. Clinical efficacy and safety Pomalidomide in combination with bortezomib and dexamethasone The efficacy and safety of pomalidomide in combination with bortezomib and low-dose dexamethasone (Pom+Btz+LD-Dex) was compared with bortezomib and low-dose dexamethasone (Btz+LD-Dex) in a Phase III multi-centre, randomised, open-label study (CC-4047-MM-007), in previously treated adult patients with multiple myeloma, who had received at least one prior regimen, including lenalidomide and have demonstrated disease progression on or after the last therapy. A total of 559 patients were enrolled and randomised in the study: 281 in the Pom+Btz+LD-Dex arm and 278 in the Btz+LD-Dex arm. 54% of patients were male with median age for the overall population of 68 years (min, max: 27, 89 years). Approximately 70% of patients were refractory to lenalidomide (71.2% in Pom+Btz+LD-Dex, 68.7 % in Btz+LD-Dex). Approximately 40% of patients were in 1st relapse and approximately 73% of patients received bortezomib as prior treatment. Patients in the Pom+Btz+LD-Dex arm were administered 4 mg pomalidomide orally on Days 1 to 14 of each 21-day cycle. Bortezomib (1.3 mg/m2/dose) was administered to patients in both study arms on Days 1, 4, 8 and 11 of a 21-day cycle for Cycles 1 to 8; and on Days 1 and 8 of a 21-day cycle for Cycles 9 and onwards. Low-dose dexamethasone (20 mg/day [≤ 75 years old] or 10 mg/day [> 75 years old]) was administered to patients in both study arms on Days 1, 2, 4, 5, 8, 9, 11 and 12 of a 21-day cycle for Cycles 1 to 8; and on Days 1, 2, 8 and 9 of each subsequent 21-day cycle from Cycles 9 onwards. Doses were reduced and treatment was temporarily interrupted or stopped as needed to manage toxicity (see section 4.2). The primary efficacy endpoint was Progression Free Survival (PFS) assessed by an Independent Response Adjudication Committee (IRAC) according to the IMWG criteria using the intent to treat population (ITT). After a median follow-up of 15.9 months, median PFS time was 11.20 months (95% CI: 9.66, 13.73) in the Pom+Btz+LD-Dex arm. In the Btz+LD-Dex arm, median PFS time was 7.1 months (95% CI: 5.88, 8.48). Summary of overall efficacy data are presented in Table 8 using a cut-off date of 26 Oct 2017. Kaplan- Meier curve for PFS for the ITT population is provided in Figure 1. Table 8. Summary of overall efficacy data Pom+Btz+LD-Dex Btz+LD-Dex (N = 281) (N = 278) PFS (months) Mediana time (95% CI) b 11.20 (9.66, 13.73) 7.10 (5.88, 8.48) HR c (95% CI), p-valued 0.61 (0.49, 0.77), <0.0001 ORR, n (%) 82.2 % 50.0% sCR 9 (3.2) 2 (0.7) CR 35 (12.5) 9 (3.2) VGPR 104 (37.0) 40 (14.4) PR 83 (29.5) 88 (31.7) OR (95% CI) e, p-valuef 5.02 (3.35, 7.52), <0.001 DoR (months) Mediana time (95% CI) b 13.7 (10.94, 18.10) 10.94 (8.11, 14.78) HRc (95% CI) 0.76 (0.56, 1.02) Btz = bortezomib; CI = Confidence interval; CR = Complete response; DoR = Duration of response; HR = Hazard Ratio; LD-Dex = low-dose dexamethasone; OR = Odds ratio; ORR = Overall response rate; PFS = Progression free survival; POM = pomalidomide; PR = Partial Response; sCR = Stringent complete response VGPR = Very good partial response. a The median is based on the Kaplan-Meier estimate. b 95% CI about the median. c Based on Cox proportional hazards model. d The p-value is based on a stratified log-rank test. e Odds ratio is for Pom+Btz+LD-Dex:Btz+LD-Dex. f The p-value is based on a CMH test, stratified by age (<=75 vs >75), Prior number of antimyeloma regimens (1 vs >1), and Beta-2 microglobulin at screening (< 3.5 mg/L versus ≥ 3.5 mg/L — ≤ 5.5 mg/L versus > 5.5 mg/L). The median duration of treatment was 8.8 months (12 treatment cycles) in the Pom+Btz+LD-Dex arm and 4.9 months (7 treament cycles) in the Btz+LD-Dex arm. The PFS advantage was more pronounced in patients who received only one prior line of therapy. In patients who received 1 prior antimyeloma line, median PFS time was 20.73 months (95% CI: 15.11, 27.99) in the Pom + Btz + LD-Dex arm and 11.63 months (95% CI: 7.52, 15.74) in the Btz + LD-Dex arm. A 46% risk reduction was observed with Pom + Btz + LD-Dex treatment (HR = 0.54, 95% CI: 0.36, 0.82). Figure 1. Progression Free Survival Based on IRAC Review of Response by IMWG Criteria (Stratified Log Rank Test) (ITT Population). Data cutoff: 26 Oct 2017 Final analysis for Overall Survival (OS), using a cut-off of 13 May 2022 (median follow-up period of 64.5 months), median OS time from Kaplan-Meier estimates was 35.6 months for the Pom + Btz + LD- Dex arm and 31.6 months for the Btz + LD-Dex arm; HR = 0.94, 95% CI: 0.77, 1.15, with an overall event rate of 70.0%. The OS analysis was not adjusted to account for subsequent therapies received. Pomalidomide in combination with dexamethasone The efficacy and safety of pomalidomide in combination with dexamethasone were evaluated in a Phase III multi-centre, randomised, open-label study (CC-4047-MM-003), where pomalidomide plus low-dose dexamethasone therapy (Pom+LD-Dex) was compared to high-dose dexamethasone alone (HD-Dex) in previously treated adult patients with relapsed and refractory multiple myeloma, who have received at least two prior treatment regimens, including both lenalidomide and bortezomib, and have demonstrated disease progression on the last therapy. A total of 455 patients were enrolled in the study: 302 in the Pom+LD-Dex arm and 153 in the HD-Dex arm. The majority of patients were male (59%) and white (79%); the median age for the overall population was 64 years (min, max: 35, 87 years). Patients in the Pom+LD-Dex arm were administered 4 mg pomalidomide orally on days 1 to 21 of each 28-day cycle. LD-Dex (40 mg) was administered once per day on days 1, 8, 15 and 22 of a 28-day cycle. For the HD-Dex arm, dexamethasone (40 mg) was administered once per day on days 1 through 4, 9 through 12, and 17 through 20 of a 28-day cycle. Patients > 75 years of age started treatment with 20 mg dexamethasone. Treatment continued until patients had disease progression. The primary efficacy endpoint was progression free survival by International Myeloma Working Group (IMWG criteria). For the intention to treat (ITT) population, median PFS time by Independent Review Adjudication Committee (IRAC) review based on IMWG criteria was 15.7 weeks (95% CI: 13.0, 20.1) in the Pom + LD-Dex arm; the estimated 26-week event-free survival rate was 35.99% (±3.46%). In the HD-Dex arm, median PFS time was 8.0 weeks (95% CI: 7.0, 9.0); the estimated 26-week event-free survival rate was 12.15% (±3.63%). PFS was evaluated in several relevant subgroups: gender, race, ECOG performance status, stratification factors (age, disease population, prior anti-myeloma therapies [2, > 2]), selected parameters of prognostic significance (baseline beta-2 microglobulin level, baseline albumin levels, baseline renal impairment, and cytogenetic risk), and exposure and refractoriness to prior anti-myeloma therapies. Regardless of the subgroup evaluated, PFS was generally consistent with that observed in the ITT population for both treatment groups. PFS is summarised in Table 9 for the ITT population. Kaplan-Meier curve for PFS for the ITT population is provided in Figure 2. Table 9. Progression Free Survival Time by IRAC Review Based on IMWG Criteria (Stratified Log Rank Test) (ITT Population) Pom+LD-Dex HD-Dex (N=302) (N=153) Progression free survival (PFS), N 302 (100.0) 153 (100.0) Censored, n (%) 138 ( 45.7) 50 ( 32.7) Progressed/Died, n (%) 164 ( 54.3) 103 ( 67.3) Progression Free Survival Time(weeks) Mediana 15.7 8.0 Two sided 95% CIb [ 13.0, 20.1] [ 7.0, 9.0] Hazard Ratio (Pom+LD-Dex:HD-Dex) 2-Sided 0.45 [0.35,0.59] 95% CI c Log-Rank Test Two sided P-Value d <0.001 Note: CI=Confidence interval; IRAC=Independent Review Adjudication Committee; NE = Not Estimable. a The median is based on Kaplan-Meier estimate. b 95% confidence interval about the median progression free survival time. c Based on Cox proportional hazards model comparing the hazard functions associated with treatment groups, stratified by age (≤75 vs >75),diseases population (refractory to both lenalidomide and bortezomib vs not refractory to both active substances), and prior number of anti myeloma therapy (=2 vs >2). d The p-value is based on a stratified log-rank test with the same stratification factors as the above Cox model. Data cutoff: 07 Sep 2012 Figure 2. Progression Free Survival Based on IRAC Review of Response by IMWG Criteria (Stratified Log Rank Test) (ITT Population) 1.0 HD-DEX POM+LD-DEX 0.8 0.6 Propotion of Patients 0.4 0.2 POM+LD-DEX vs HD-DEX Logrank p-value = < 0.001 (2-sided) HR (95% CI) 0.45 (0.35, 0.59) Events: POM+LD-DEX=164/302 HD-DEX=103/153 0.0 0 13 26 39 52 65 Progression Free Survival (weeks) Data cutoff: 07 Sep 2012 Overall Survival was the key secondary study endpoint. A total of 226 (74.8%) of the Pom + LD-Dex patients and 95 (62.1%) of the HD-Dex patients were alive as of the cutoff date (07 Sep 2012). Median OS time from Kaplan-Meier estimates has not been reached for the Pom + LD-Dex, but would be expected to be at least 48 weeks, which is the lower boundary of the 95% CI. Median OS time for the HD-Dex arm was 34 weeks (95% CI: 23.4, 39.9). The 1-year event free rate was 52.6% (± 5.72%) for the Pom + LD- Dex arm and 28.4% (± 7.51%) for the HD-Dex arm. The difference in OS between the two treatment arms was statistically significant (p < 0.001). Overall survival is summarised in Table 10 for the ITT population. Kaplan-Meier curve for OS for the ITT population is provided in Figure 3. Based on the results of both PFS and OS endpoints, the Data Monitoring Committee established for this study recommended that the study be completed and patients in the HD-Dex arm be crossed over to the Pom + LD-Dex arm. Table 10. Overall Survival: ITT Population Pom+LD-Dex HD-Dex Statistics (N=302) (N=153) N 302 (100.0) 153 (100.0) Censored n (%) 226 ( 74.8) 95 ( 62.1) Died n (%) 76 ( 25.2) 58 ( 37.9) Survival Time (weeks) Mediana NE 34.0 Two sided 95% CIb [ 48.1, NE] [ 23.4, 39.9] Hazard Ratio (Pom+LD-Dex:HD-Dex) [Two sided 0.53[ 0.37, 0.74] 95% CIc] Log-Rank Test Two sided P-Valued <0.001 Note: CI=Confidence interval. NE = Not Estimable. a The median is based on Kaplan-Meier estimate. b 95% confidence interval about the median overall survival time. c Based on Cox proportional hazards model comparing the hazard functions associated with treatment groups. d The p-value is based on an unstratified log-rank test. Data cutoff: 07 Sep 2012 Figure 3. Kaplan-Meier Curve of Overall Survival (ITT Population) 1.0 HD -DEX POM+LD -DEX 0.8 0.6 Propotion of Patients 0.4 POM+LD-DEX vs HD-DEX Logrank p-value = < 0.001 (2-sided) 0.2 HR (95% CI) 0.53 (0.37, 0.74) KM median: POM+LD-DEX=NE [48.1, NE] KM median: HD-DEX = 34.0[23.4, 39.9] Events: POM+LD-DEX=75/284 HD-DEX=56/139 0.0 0 13 26 39 52 65 Overall Survival (week) cutoff: 07 Sep 2012
Pharmacokinetic Properties
5.2 Pharmacokinetic properties Absorption Pomalidomide is absorbed with a maximum plasma concentration (Cmax) occurring between 2 and 3 hours and is at least 73% absorbed following administration of single oral dose. The systemic exposure (AUC) of pomalidomide increases in an approximately linear and dose proportional manner. Following multiple doses, pomalidomide has an accumulation ratio of 27 to 31% on AUC. Coadministration with a high-fat and high-calorie meal slows the rate of absorption, decreasing mean plasma Cmax by approximately 27%, but has minimal effect on the overall extent of absorption with an 8% decrease in mean AUC. Therefore, pomalidomide can be administered without regard to food intake. Distribution Pomalidomide has a mean apparent volume of distribution (Vd/F) between 62 and 138 L at steady state. Pomalidomide is distributed in semen of healthy subjects at a concentration of approximately 67% of plasma level at 4 hours post-dose (approximately Tmax) after 4 days of once daily dosing at 2 mg. In vitro binding of pomalidomide enantiomers to proteins in human plasma ranges from 12% to 44% and is not concentration dependent. Biotransformation Pomalidomide is the major circulating component (approximately 70% of plasma radioactivity) in vivo in healthy subjects who received a single oral dose of [14C] -pomalidomide (2 mg). No metabolites were present at >10% relative to parent or total radioactivity in plasma. The predominant metabolic pathways of excreted radioactivity are hydroxylation with subsequent glucuronidation, or hydrolysis. In vitro, CYP1A2 and CYP3A4 were identified as the primary enzymes involved in the CYP-mediated hydroxylation of pomalidomide, with additional minor contributions from CYP2C19 and CYP2D6. Pomalidomide is also a substrate of P-glycoprotein in vitro. Co-administration of pomalidomide with the strong CYP3A4/5 and P-gp inhibitor ketoconazole, or the strong CYP3A4/5 inducer carbamazepine, had no clinically relevant effect on exposure to pomalidomide. Co-administration of the strong CYP1A2 inhibitor fluvoxamine with pomalidomide in the presence of ketoconazole, increased mean exposure to pomalidomide by 107% with a 90% confidence interval [91% to 124%] compared to pomalidomide plus ketoconazole. In a second study to evaluate the contribution of a CYP1A2 inhibitor alone to metabolism changes, co-administration of fluvoxamine alone with pomalidomide increased mean exposure to pomalidomide by 125% with a 90% confidence interval [98% to 157%] compared to pomalidomide alone. If strong inhibitors of CYP1A2 (e.g. ciprofloxacin, enoxacin and fluvoxamine) are co-administered with pomalidomide, reduce the dose of pomalidomide to 50%. Administration of pomalidomide in smokers, with smoking tobacco known to induce the CYP1A2 isoform, had no clinically relevant effect on exposure to pomalidomide compared to that exposure to pomalidomide observed in non-smokers. Based on in vitro data, pomalidomide is not an inhibitor or inducer of cytochrome P-450 isoenzymes and does not inhibit any drug transporters that were studied. Clinically relevant interactions are not anticipated when pomalidomide is coadministered with substrates of these pathways. Elimination Pomalidomide is eliminated with a median plasma half-life of approximately 9.5 hours in healthy subjects and approximately 7.5 hours in patients with multiple myeloma. Pomalidomide has a mean total body clearance (CL/F) of approximately 7-10 L/hr. Following a single oral administration of [14C]-pomalidomide (2 mg) to healthy subjects, approximately 73% and 15% of the radioactive dose was eliminated in urine and faeces, respectively, with approximately 2% and 8% of the dosed radiocarbon eliminated as pomalidomide in urine and faeces. Pomalidomide is extensively metabolised prior to excretion, with the resulting metabolites eliminated primarily in the urine. The 3 predominant metabolites in urine (formed via hydrolysis or hydroxylation with subsequent glucuronidation) account for approximately 23%, 17%, and 12%, respectively, of the dose in the urine. CYP dependent metabolites account for approximately 43% of the total excreted radioactivity, while non- CYP dependent hydrolytic metabolites account for 25%, and excretion of unchanged pomalidomide accounted for 10% (2% in urine and 8% in faeces). Population Pharmacokinetics (PK) Based on population PK analysis using a two-compartment model, healthy subjects and MM patients had comparable apparent clearance (CL/F) and apparent central volume of distribution (V2/F). In peripheral tissues, pomalidomide was preferentially taken up by tumours with apparent peripheral distribution clearance (Q/F) and apparent peripheral volume of distribution (V3/F) 3.7-fold and 8-fold higher, respectively, than that of healthy subjects. Elderly Based on population pharmacokinetic analyses in healthy subjects and multiple myeloma patients, no significant influence of age (19-83 years) on oral clearance of pomalidomide was observed. In clinical studies, no dose adjustment was required in elderly (> 65 years) patients exposed to pomalidomide. (see section 4.2). Renal impairment Population pharmacokinetic analyses showed that the pomalidomide pharmacokinetic parameters were not remarkably affected in renally impaired patients (defined by creatinine clearance or estimated glomerular filtration rate [eGFR]) compared to patients with normal renal function (CrCl ≥60mL/minute). Mean normalised AUC exposure to pomalidomide was 98.2% with a 90% confidence interval [77.4% to 120.6%] in moderate renal impairment patients (eGFR ≥30 to ≤45 mL/minute/1.73m2) compared to patients with normal renal function. Mean normalised AUC exposure to pomalidomide was 100.2% with a 90% confidence interval [79.7% to 127.0%] in severe renal impairment patients not requiring dialysis (CrCl <30 or eGFR <30 mL/minute/1.73 m2) compared to patients with normal renal function. Mean normalised AUC exposure to pomalidomide increased by 35.8% with a 90% CI [7.5% to 70.0%] in severe renal impairment patients requiring dialysis (CrCl <30mL/minute requiring dialysis) compared to patients with normal renal function. The mean changes in exposure to pomalidomide in each of these renal impairment groups are not of a magnitude that requires dose adjustments. Hepatic impairment The pharmacokinetic parameters were modestly changed in hepatically impaired patients (defined by Child-Pugh criteria) compared to healthy subjects. Mean exposure to pomalidomide increased by 51% with a 90% confidence interval [9% to 110%] in mildly hepatically impaired patients compared to healthy subjects. Mean exposure to pomalidomide increased by 58% with a 90% confidence interval [13% to 119%] in moderately hepatically impaired patients compared to healthy subjects. Mean exposure to pomalidomide increased by 72% with a 90% confidence interval [24% to 138%] in severely hepatically impaired patients compared to healthy subjects. The mean increases in exposure to pomalidomide in each of these impairment groups are not of a magnitude for which adjustments in schedule or dose are required (see section 4.2).

פרטי מסגרת הכללה בסל
1. התרופה האמורה תינתן לטיפול במיאלומה נפוצה ובהתקיים כל אלה: א. לטיפול בחולה שמחלתו עמידה או נשנית לאחר מיצוי טיפול בקו טיפול קודם אחד לפות.ב. התרופות Carfilzomib, Pomalidomide לא יינתנו בשילוב אחת עם השנייה.2. מתן התרופה האמורה ייעשה לפי מרשם של מומחה באונקולוגיה או רופא מומחה בהמטולוגיה.
מסגרת הכללה בסל
התוויות הכלולות במסגרת הסל
| התוויה | תאריך הכללה | תחום קליני | Class Effect | מצב מחלה |
|---|---|---|---|---|
| 1. התרופה האמורה תינתן לטיפול במיאלומה נפוצה ובהתקיים כל אלה: א. לטיפול בחולה שמחלתו עמידה או נשנית לאחר מיצוי טיפול בקו טיפול קודם אחד לפות. ב. התרופות Carfilzomib, Pomalidomide לא יינתנו בשילוב אחת עם השנייה. 2. מתן התרופה האמורה ייעשה לפי מרשם של מומחה באונקולוגיה או רופא מומחה בהמטולוגיה. | 01/02/2023 | המטולוגיה | מיאלומה נפוצה, Multiple myeloma | |
| 1. התרופה האמורה תינתן לטיפול במיאלומה נפוצה ובהתקיים כל אלה: א. לטיפול בחולה שמחלתו עמידה או נשנית לאחר מיצוי טיפול בשני קווי טיפול קודמים. ב. התרופות Carfilzomib, Pomalidomide לא יינתנו בשילוב אחת עם השנייה. 2. מתן התרופה האמורה ייעשה לפי מרשם של מומחה באונקולוגיה או רופא מומחה בהמטולוגיה. | 03/02/2022 | המטולוגיה | מיאלומה נפוצה, Multiple myeloma | |
| 1. התרופה האמורה תינתן לטיפול במיאלומה נפוצה ובהתקיים כל אלה: א. לטיפול בחולה שמחלתו עמידה או נשנית לאחר מיצוי טיפול בכל אחד מאלה – Thalidomide, Bortezomib, Lenalidomide, אלא אם כן לחולה הייתה הורית נגד לאחד מהטיפולים האמורים. ב. במהלך מחלתו יהיה החולה זכאי לטיפול בתרופה אחת בלבד מהתרופות המפורטות להלן – Carfilzomib, Pomalidomide, וזאת למעט בחולה אשר לא השיג תגובה מינימלית לאחר ניסיון טיפולי של 2 מחזורי טיפול באחת מהתרופות. ג. התרופות Carfilzomib, Pomalidomide לא יינתנו בשילוב אחת עם השנייה. 2. מתן התרופה האמורה ייעשה לפי מרשם של מומחה באונקולוגיה או רופא מומחה בהמטולוגיה. | 12/01/2014 | המטולוגיה | מיאלומה נפוצה, Multiple myeloma |
שימוש לפי פנקס קופ''ח כללית 1994
לא צוין
תאריך הכללה מקורי בסל
12/01/2014
הגבלות
תרופה מוגבלת לרישום ע'י רופא מומחה או הגבלה אחרת
מידע נוסף
עלון מידע לצרכן
01.06.22 - עלון לצרכן אנגלית 01.06.22 - עלון לצרכן עברית 01.06.22 - עלון לצרכן ערבית 22.02.24 - עלון לצרכן עברית 22.02.24 - עלון לצרכן אנגלית 22.02.24 - עלון לצרכן עברית 22.02.24 - עלון לצרכן אנגלית 22.02.24 - עלון לצרכן עברית 22.02.24 - עלון לצרכן עברית 22.02.24 - עלון לצרכן עברית 22.02.24 - עלון לצרכן עברית 22.02.24 - עלון לצרכן עברית 22.02.24 - עלון לצרכן עברית 23.02.24 - עלון לצרכן עברית 22.02.24 - עלון לצרכן עברית 04.06.24 - עלון לצרכן אנגלית 04.06.24 - עלון לצרכן ערבית 16.02.15 - החמרה לעלון 03.03.16 - החמרה לעלון 13.06.16 - החמרה לעלון 20.11.16 - החמרה לעלון 15.11.18 - החמרה לעלון 18.04.21 - החמרה לעלון 13.03.22 - החמרה לעלון 22.02.24 - החמרה לעלוןלתרופה במאגר משרד הבריאות
אימנוביד 3 מ"ג