Quest for the right Drug
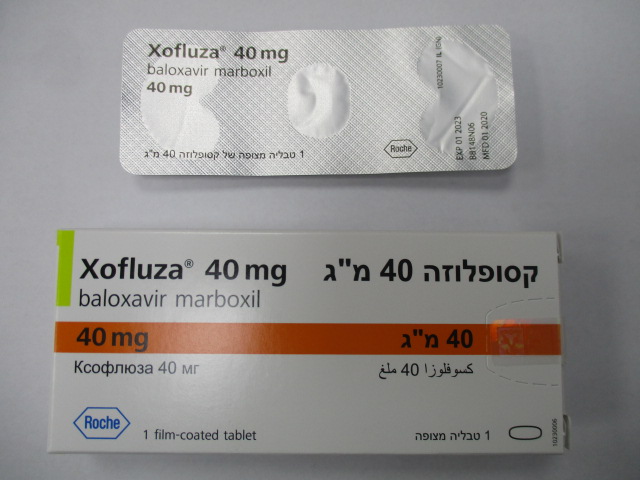
קסופלוזה 40 מ"ג XOFLUZA 40 MG (BALOXAVIR MARBOXIL)
תרופה במרשם
תרופה בסל
נרקוטיקה
ציטוטוקסיקה
צורת מתן:
פומי : PER OS
צורת מינון:
טבליות מצופות פילם : FILM COATED TABLETS
עלון לרופא
מינוניםPosology התוויות
Indications תופעות לוואי
Adverse reactions התוויות נגד
Contraindications אינטראקציות
Interactions מינון יתר
Overdose הריון/הנקה
Pregnancy & Lactation אוכלוסיות מיוחדות
Special populations תכונות פרמקולוגיות
Pharmacological properties מידע רוקחי
Pharmaceutical particulars אזהרת שימוש
Special Warning עלון לרופא
Physicians Leaflet
Pharmacological properties : תכונות פרמקולוגיות
Pharmacodynamic Properties
12.2 Pharmacodynamics Cardiac Electrophysiology At twice the expected exposure from recommended dosing, XOFLUZA did not prolong the QTc interval. Exposure-Response Relationships When XOFLUZA is dosed by weight, as recommended (40 mg in patients weighing 40–80 kg; 80 mg in patients weighing at least 80 kg), no difference in baloxavir exposure-response (time to alleviation of influenza symptoms in the otherwise healthy population or time to improvement of influenza symptoms in the high risk population) relationship has been observed.
Pharmacokinetic Properties
12.3 Pharmacokinetics Baloxavir marboxil is a prodrug that is almost completely converted to its active metabolite, baloxavir, following oral administration. Baloxavir pharmacokinetic parameters are presented for healthy adults and adolescents as the mean [% coefficient of variation (% CV)], unless otherwise specified, in Table 3. Absorption, distribution, metabolism, and elimination data for XOFLUZA is presented in Table 4. Table 3 Pharmacokinetic Parameters of Plasma Baloxavir in Adults and Adolescents (≥ 12 Years of Age) Pharmacokinetic Parameters of Plasma Baloxavir in Adults XOFLUZA dose XOFLUZA dose and Adolescentsa 40 mg 80 mg AUC (ng·hr/mL) 5520 (46.3%) 6930 (48.6%) Cmax (ng/mL) 68.9 (44.9%) 82.5 (43.0%) C24 (ng/mL) 50.9 (45.8%) 62.6 (45.9%) C72 (ng/mL) 24.2 (45.5%) 30.8 (47.0%) a Trial T0831 summary data, mean (%CV) Table 4 Baloxavir Absorption, Distribution, Metabolism, Elimination Data Absorption Tmax (hr)a 4 Effect of food (relative to fasting)b Cmax: ↓48%, AUC0-inf: ↓36% Distribution % bound to human serum proteinsc 92.9–93.9 Ratio of blood cell to blood 48.5%–54.4% Volume of distribution (V/F, L)d 1180 (20.8%) Elimination Clearance (CL/F, L/hr) 10.3 (22.5%) Apparent terminal elimination half-life (hr) 79.1 (22.4%) Metabolism Metabolic pathways Primary: UGT1A3 Secondary: CYP3A4 Excretion % of dose excretede Urine: 14.7 (total radioactivity); 3.3 (baloxavir) Feces: 80.1 (total radioactivity) a Median b Meal: approximately 400 to 500 kcal including 150 kcal from fat c in vitro d Geometric mean (geometric CV%) e Ratio of radioactivity to radio-labeled baloxavir marboxil dose in mass balance study No clinically significant differences in the pharmacokinetics of baloxavir were observed based on age, sex , presence of risk factors for complicated influenza, creatinine clearance (CrCl: 50 mL/min and above), or moderate hepatic impairment (Child-Pugh class B). The effect of severe renal or hepatic impairment on baloxavir pharmacokinetics has not been evaluated. Body Weight Baloxavir exposure decreases as body weight increases. No clinically significant difference in exposure was observed between body weight groups following the approved recommended dosage. Race/Ethnicity Based on a population pharmacokinetic analysis, baloxavir exposure is approximately 35% lower in non-Asians as compared to Asians; this difference is not considered clinically significant when the recommended dose was administered. Drug Interaction Studies Clinical Studies No clinically significant changes in the pharmacokinetics of baloxavir marboxil and its active metabolite, baloxavir, were observed when coadministered with itraconazole (combined strong CYP3A and P-gp inhibitor), probenecid (UGT inhibitor), or oseltamivir. No clinically significant changes in the pharmacokinetics of the following drugs were observed when coadministered with baloxavir marboxil: midazolam (CYP3A4 substrate), digoxin (P-gp substrate), rosuvastatin (BCRP substrate), or oseltamivir. Animal Studies Polyvalent Cations: In monkeys, a 48% to 63% decrease in baloxavir exposure was observed when XOFLUZA was coadministered with calcium, aluminum, magnesium, or iron. No study has been conducted in humans. In Vitro Studies Cytochrome P450 (CYP) Enzymes: Both baloxavir marboxil and baloxavir do not inhibit CYP1A2, CYP2B6, CYP2C8, CYP2C9, CYP2C19, or CYP2D6 and do not induce CYP1A2, CYP2B6, or CYP3A4. Uridine diphosphate (UDP)-glucuronosyl transferase (UGT) Enzymes: Both baloxavir marboxil and baloxavir do not inhibit UGT1A1, UGT1A3, UGT1A4, UGT1A6, UGT1A9, UGT2B7, or UGT2B15. Transporter Systems: Both baloxavir marboxil and baloxavir are substrates of P-glycoprotein (P-gp). Baloxavir does not inhibit organic anion-transporting polypeptides (OATP) 1B1, OATP1B3, organic cation transporter (OCT) 1, OCT2, organic anion transporter (OAT) 1, OAT3, multidrug and toxin extrusion (MATE) 1, or MATE2K. 12.4 Microbiology Mechanism of Action Baloxavir marboxil is a prodrug that is converted by hydrolysis to baloxavir, the active form that exerts anti- influenza virus activity. Baloxavir inhibits the endonuclease activity of the polymerase acidic (PA) protein, an influenza virus-specific enzyme in the viral RNA polymerase complex required for viral gene transcription, resulting in inhibition of influenza virus replication. The 50% inhibitory concentration (IC50) values of baloxavir ranged from 1.4 to 3.1 nM (n=4) for influenza A viruses and 4.5 to 8.9 nM (n=3) for influenza B viruses in a PA endonuclease assay. Viruses with reduced susceptibility to baloxavir have amino acid substitutions in the PA protein. Antiviral Activity The antiviral activity of baloxavir against laboratory strains and clinical isolates of influenza A and B viruses was determined in an MDCK cell-based plaque reduction assay. The median 50% effective concentration (EC50) values of baloxavir were 0.73 nM (n=31; range: 0.20–1.85 nM) for subtype A/H1N1 strains, 0.83 nM (n=33; range: 0.35–2.63 nM) for subtype A/H3N2 strains, and 5.97 nM (n=30; range: 2.67–14.23 nM) for type B strains. In an MDCK cell-based virus titer reduction assay, the 90% effective concentration (EC90) values of baloxavir against avian subtypes A/H5N1 and A/H7N9 were in the range of 0.80 to 3.16 nM. The relationship between antiviral activity in cell culture and clinical response to treatment in humans has not been established. Resistance Cell Culture Influenza A virus isolates with reduced susceptibility to baloxavir were selected by serial passage of virus in cell culture in the presence of increasing concentrations of baloxavir. Reduced susceptibility of influenza A virus to baloxavir was conferred by amino acid substitutions I38T (A/H1N1 and A/H3N2), E198K (A/H1N1) and E199G (A/H3N2) in the PA protein of the viral RNA polymerase complex. An E18G (A/H1N1) substitution in the PA protein, selected by a baloxavir analog, also conferred reduced susceptibility to baloxavir. Clinical Studies Treatment-emergent substitutions were identified in influenza A and B viruses in clinical studies. Substitutions associated with a >3-fold reduction in susceptibility to baloxavir are shown in Table 5. Table 5 Treatment-Emergent Amino Acid Substitutions in PA Associated with Reduced Susceptibility to Baloxavir Identified in Clinical Specimens Influenza Type/Subtype A/H1N1 A/H3N2 B Amino Acid Substitution E23G/K/R, A37T, E23G/K, A37T, I38M/T, T20K, I38T I38F/N/S/T E199G Clinical studies in adult and adolescent subjects ≥ 12 years of age: In adult and adolescent subjects who had a confirmed influenza virus infection, the overall frequencies of treatment-emergent amino acid substitutions associated with reduced susceptibility to baloxavir were 5% (6/134), 11% (53/485), and 1% (2/224) in influenza A/H1N1, A/H3N2, and B virus infections, respectively, in pooled data from Trials T0821, T0831, and T0832 [see Clinical Studies (14)]. In Trial T0834, of 303 subjects ≥ 12 years of age who received XOFLUZA post-exposure prophylaxis, 32 were viral RNA-positive post-baseline, including 17 subjects who were evaluated for resistance. Of these 17 subjects, influenza virus with substitutions associated with reduced susceptibility to baloxavir was identified in 4/4 subjects who developed clinical influenza (as described for the primary endpoint) and 6/13 other subjects evaluated who did not meet the primary endpoint definition for clinical influenza [see Clinical Studies (14)]. Surveillance Studies Amino acid substitutions associated with reduced susceptibility to baloxavir have also been identified in surveillance studies or in cell culture studies evaluating the impact of resistance substitutions identified in one influenza virus type/subtype on baloxavir susceptibility when introduced into other influenza virus types/subtypes (Table 6). Table 6 Amino Acid Substitutions in PA Associated with Reduced Susceptibility to Baloxavir Identified in Surveillance and in Cell Culture Resistance Studies Influenza Type/Subtype A/H1N1 A/H3N2 B Amino Acid Substitution A36V†, I38L†/M‡ E23R‡, A36V‡, I38F‡/M‡/N‡/S‡ I38F‡/N‡/S‡ † Identifiedin human surveillance isolates, antiviral treatment unknown ‡ Known substitution associated with reduced susceptibility to baloxavir identified in clinical specimens or surveillance isolates but evaluated in the indicated alternative type/subtype by reverse genetics None of the treatment-emergent substitutions associated with reduced susceptibility to baloxavir were identified in virus from pretreatment respiratory specimens in the clinical studies. Treatment-emergent resistance has been associated with influenza virus rebound and prolonged virus shedding; however, the impact of prolonged shedding on clinical outcomes and virus transmission potential is currently unknown. The frequency of baloxavir resistance and the prevalence of such resistant virus may vary seasonally and geographically. Prescribers should consider available information from the U.S. CDC and/or a local health department on current influenza virus drug susceptibility patterns and treatment effects when deciding whether to use XOFLUZA. Cross-Resistance Cross-resistance between baloxavir and neuraminidase (NA) inhibitors, or between baloxavir and M2 proton pump inhibitors (adamantanes), is not expected because these drugs target different viral proteins. The NA inhibitor oseltamivir is active against viruses with reduced susceptibility to baloxavir, including A/H1N1 virus with PA substitutions E23K or I38F/T; A/H3N2 virus with PA substitutions E23G/K, A37T, I38M/T, or E199G; and type B virus with the PA substitution I38T. Influenza virus may carry amino acid substitutions in PA that reduce susceptibility to baloxavir and at the same time carry resistance-associated substitutions for NA inhibitors and M2 proton pump inhibitors. Baloxavir is active against NA inhibitor-resistant strains, including A/H1N1 and A/H5N1 viruses with the NA substitution H275Y (A/H1N1 numbering), A/H3N2 virus with the NA substitutions E119V or R292K, A/H7N9 virus with the NA substitution R292K (A/H3N2 numbering), and type B virus with the NA substitutions R152K or D198E (A/H3N2 numbering). The clinical relevance of phenotypic cross-resistance evaluations has not been established. Immune Response Interaction studies with influenza vaccines and baloxavir marboxil have not been conducted.

שימוש לפי פנקס קופ''ח כללית 1994
לא צוין
תאריך הכללה מקורי בסל
לא צוין
הגבלות
לא צוין
מידע נוסף
עלון מידע לצרכן
26.03.20 - עלון לצרכן אנגלית 14.09.20 - עלון לצרכן עברית 14.09.20 - עלון לצרכן ערבית 05.12.22 - עלון לצרכן עברית 11.05.23 - עלון לצרכן אנגלית 01.03.23 - עלון לצרכן עברית 11.05.23 - עלון לצרכן ערבית 13.07.23 - עלון לצרכן עברית 12.09.23 - עלון לצרכן אנגלית 14.09.23 - עלון לצרכן עברית 11.09.23 - עלון לצרכן ערבית 25.02.20 - החמרה לעלון 01.03.23 - החמרה לעלוןלתרופה במאגר משרד הבריאות
קסופלוזה 40 מ"ג