Quest for the right Drug
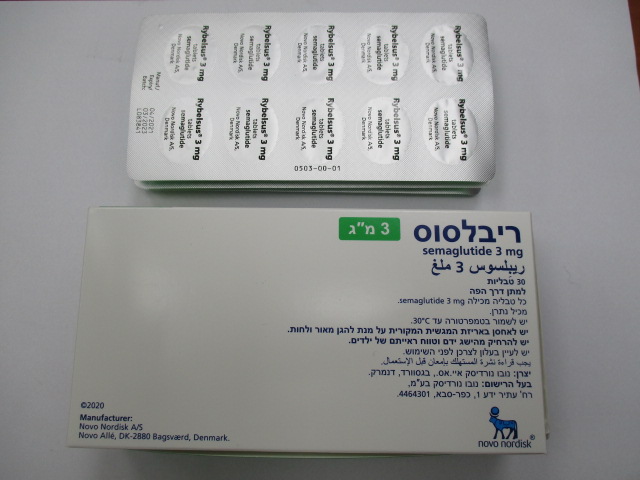
ריבלסוס 3 מ"ג RYBELSUS 3 MG (SEMAGLUTIDE)
תרופה במרשם
תרופה בסל
נרקוטיקה
ציטוטוקסיקה
צורת מתן:
פומי : PER OS
צורת מינון:
טבליה : TABLETS
עלון לרופא
מינוניםPosology התוויות
Indications תופעות לוואי
Adverse reactions התוויות נגד
Contraindications אינטראקציות
Interactions מינון יתר
Overdose הריון/הנקה
Pregnancy & Lactation אוכלוסיות מיוחדות
Special populations תכונות פרמקולוגיות
Pharmacological properties מידע רוקחי
Pharmaceutical particulars אזהרת שימוש
Special Warning עלון לרופא
Physicians Leaflet
Pharmacological properties : תכונות פרמקולוגיות
Pharmacodynamic Properties
5.1 Pharmacodynamic properties Pharmacotherapeutic group: Drugs used in diabetes, Glucagon-like peptide-1 (GLP-1) analogues, ATC code: A10BJ06 Mechanism of action Semaglutide is a GLP-1 analogue with 94% sequence homology to human GLP-1. Semaglutide acts as a GLP-1 receptor agonist that selectively binds to and activates the GLP-1 receptor, the target for native GLP-1. GLP-1 is a physiological hormone that has multiple actions in glucose and appetite regulation, and in the cardiovascular system. The glucose and appetite effects are specifically mediated via GLP-1 receptors in the pancreas and the brain. Semaglutide reduces blood glucose in a glucose-dependent manner by stimulating insulin secretion and lowering glucagon secretion when blood glucose is high. The mechanism of blood glucose lowering also involves a minor delay in gastric emptying in the early postprandial phase. During hypoglycaemia, semaglutide diminishes insulin secretion and does not impair glucagon secretion. The mechanism of semaglutide is independent of the route of administration. Semaglutide reduces body weight and body fat mass through lowered energy intake, involving an overall reduced appetite. In addition, semaglutide reduces the preference for high fat foods. GLP-1 receptors are expressed in the heart, vasculature, immune system and kidneys. Semaglutide has a beneficial effect on plasma lipids, lowers systolic blood pressure and reduces inflammation in clinical studies. In animal studies, semaglutide attenuates the development of atherosclerosis by preventing aortic plaque progression and reducing inflammation in the plaque. Pharmacodynamic effects The pharmacodynamic evaluations described below were performed with orally administered semaglutide after 12 weeks of treatment. Fasting and postprandial glucose Semaglutide reduces fasting and postprandial glucose concentrations. In patients with type 2 diabetes, treatment with semaglutide resulted in a relative reduction compared to placebo of 22% [13; 30] for fasting glucose and 29% [19; 37] for postprandial glucose. Glucagon secretion Semaglutide lowers the postprandial glucagon concentrations. In patients with type 2 diabetes, semaglutide resulted in the following relative reductions in glucagon compared to placebo: postprandial glucagon response of 29% [15; 41]. Gastric emptying Semaglutide causes a minor delay in early postprandial gastric emptying, with paracetamol exposure (AUC0-1h) 31% [13; 46] lower in the first hour after the meal, thereby reducing the rate at which glucose appears in the circulation postprandially. Fasting and postprandial lipids Semaglutide compared to placebo lowered fasting triglyceride and very-low-density lipoproteins (VLDL) cholesterol concentrations by 19% [8; 28] and 20% [5; 33], respectively. The postprandial triglyceride and VLDL cholesterol response to a high fat meal was reduced by 24% [9; 36] and 21% [7; 32], respectively. ApoB48 was reduced both in fasting and postprandial state by 25% [2; 42] and 30% [15; 43], respectively. Clinical efficacy and safety The efficacy and safety of Rybelsus have been evaluated in eight global randomised controlled phase 3a trials. In seven trials, the primary objective was the assessment of the glycaemic efficacy; in one trial, the primary objective was the assessment of cardiovascular outcomes. The trials included 8,842 randomised patients with type 2 diabetes (5,169 treated with semaglutide), including 1,165 patients with moderate renal impairment. Patients had an average age of 61 years (range 18 to 92 years), with 40% of patients ≥ 65 years of age and 8% ≥ 75 years of age. The efficacy of semaglutide was compared with placebo or active controls (sitagliptin, empagliflozin and liraglutide). The efficacy of semaglutide was not impacted by baseline age, gender, race, ethnicity, body weight, BMI, diabetes duration, upper gastrointestinal disease and level of renal function. PIONEER 1 – Monotherapy In a 26-week double-blind trial, 703 patients with type 2 diabetes inadequately controlled with diet and exercise were randomised to semaglutide 3 mg, semaglutide 7 mg, semaglutide 14 mg or placebo once daily. Table 2 Results of a 26-week monotherapy trial comparing semaglutide with placebo (PIONEER 1) Semaglutide Semaglutide Placebo 7 mg 14 mg Full analysis set (N) 175 175 178 HbA1c (%) Baseline 8.0 8.0 7.9 Change from baseline1 −1.2 −1.4 −0.3 Difference from placebo1 [95% CI] −0.9 [−1.1; −0.6]* −1.1 [−1.3; −0.9]* - Patients (%) achieving HbA1c <7.0% 69 § 77 § 31 FPG (mmol/L) Baseline 9.0 8.8 8.9 Change from baseline1 −1.5 −1.8 −0.2 Difference from placebo1 [95% CI] −1.4 [−1.9; −0.8]§ −1.6 [−2.1; −1.2]§ - Body weight (kg) Baseline 89.0 88.1 88.6 Change from baseline1 −2.3 −3.7 −1.4 Difference from placebo1 [95% CI] −0.9 [−1.9; 0.1] −2.3 [−3.1; −1.5]* - 1Irrespective of treatment discontinuation or initiation of rescue medication (pattern mixture model using multiple imputation). * p<0.001 (unadjusted 2-sided) for superiority, controlled for multiplicity. § p<0.05, not controlled for multiplicity; for ‘Patients achieving HbA1c <7.0%’, the p-value is for the odds ratio. PIONEER 2 – Semaglutide vs. empagliflozin, both in combination with metformin In a 52-week open-label trial, 822 patients with type 2 diabetes were randomised to semaglutide 14 mg once daily or empagliflozin 25 mg once daily, both in combination with metformin. Table 3 Results of a 52-week trial comparing semaglutide with empagliflozin (PIONEER 2) Semaglutide Empagliflozin 14 mg 25 mg Full analysis set (N) 411 410 Week 26 HbA1c (%) Baseline 8.1 8.1 Change from baseline1 −1.3 −0.9 Difference from empagliflozin1 [95% CI] −0.4 [−0.6; −0.3]* - Patients (%) achieving HbA1c <7.0% 67§ 40 FPG (mmol/L) Baseline 9.5 9.7 Change from baseline1 −2.0 −2.0 Difference from empagliflozin1 [95% CI] 0.0 [−0.2; 0.3] - Body weight (kg) Baseline 91.9 91.3 Change from baseline1 −3.8 −3.7 Difference from empagliflozin1 [95% CI] −0.1 [−0.7; 0.5] - Week 52 HbA1c (%) Change from baseline1 −1.3 −0.9 Difference from empagliflozin1 [95% CI] −0.4 [−0.5; −0.3]§ - Patients (%) achieving HbA1c <7.0% 66§ 43 Body weight (kg) Change from baseline1 −3.8 −3.6 Difference from empagliflozin1 [95% CI] −0.2 [−0.9; 0.5] - 1Irrespective of treatment discontinuation or initiaton of rescue medicaton (pattern mixture model using multiple imputation). * p<0.001 (unadjusted 2-sided) for superiority, controlled for multiplicity. § p<0.05, not controlled for multiplicity; for ‘Patients achieving HbA1c <7.0%’, the p-value is for the odds ratio. PIONEER 3 – Semaglutide vs. sitagliptin, both in combination with metformin or metformin with sulfonylurea In a 78-week, double-blind, double-dummy trial, 1,864 patients with type 2 diabetes were randomised to semaglutide 3 mg, semaglutide 7 mg, semaglutide 14 mg or sitagliptin 100 mg once daily, all in combination with metformin alone or metformin and sulfonylurea. Reductions in HbA1c and body weight were sustained throughout the trial duration of 78 weeks. Table 4 Results of a 78-week trial comparing semaglutide with sitagliptin (PIONEER 3) Semaglutide Semaglutide Sitagliptin 7 mg 14 mg 100 mg Full analysis set (N) 465 465 467 Week 26 HbA1c (%) Baseline 8.4 8.3 8.3 Change from baseline1 −1.0 −1.3 −0.8 Difference from sitagliptin1 [95% CI] −0.3 [−0.4; −0.1]* −0.5 [−0.6; −0.4]* - Patients (%) achieving HbA1c <7.0% 44§ 56§ 32 FPG (mmol/L) Baseline 9.4 9.3 9.5 Change from baseline1 −1.2 −1.7 −0.9 Difference from sitagliptin1 [95% CI] −0.3 [−0.6; 0.0]§ −0.8 [−1.1; −0.5]§ - Body weight (kg) Baseline 91.3 91.2 90.9 Change from baseline1 −2.2 −3.1 −0.6 Difference from sitagliptin1 [95% CI] −1.6 [−2.0; −1.1]* −2.5 [−3.0; −2.0]* - Week 78 HbA1c (%) Change from baseline1 −0.8 −1.1 −0.7 Difference from sitagliptin1 [95% CI] −0.1 [−0.3; 0.0] −0.4 [−0.6; −0.3]§ - Patients (%) achieving HbA1c <7.0% 39§ 45§ 29 Body weight (kg) Change from baseline1 −2.7 −3.2 −1.0 Difference from sitagliptin1 [95% CI] −1.7 [−2.3; −1.0]§ −2.1 [−2.8; −1.5]§ - 1Irrespective of treatment discontinuation or initiation of rescue medication (pattern mixture model using multiple imputation). * p<0.001 (unadjusted 2-sided) for superiority, controlled for multiplicity. § p<0.05, not controlled for multiplicity; for ‘Patients achieving HbA1c <7.0%’, the p-value is for the odds ratio. PIONEER 4 – Semaglutide vs. liraglutide and placebo, all in combination with metformin or metformin with an SGLT2 inhibitor In a 52-week double-blind, double-dummy trial, 711 patients with type 2 diabetes were randomised to semaglutide 14 mg, liraglutide 1.8 mg subcutaneous injection or placebo once daily, all in combination with metformin or metformin and an SGLT2 inhibitor. Table 5 Results of a 52-week trial comparing semaglutide with liraglutide and placebo (PIONEER 4) Semaglutide Liraglutide Placebo 14 mg 1.8 mg Full analysis set (N) 285 284 142 Week 26 HbA1c (%) Baseline 8.0 8.0 7.9 Change from baseline1 −1.2 −1.1 −0.2 Difference from liraglutide1 [95% CI] −0.1 [−0.3; 0.0] - - Difference from placebo1 [95% CI] −1.1 [−1.2; −0.9]* - - Patients (%) achieving HbA1c <7.0% 68§,a 62 14 FPG (mmol/L) Baseline 9.3 9.3 9.2 Change from baseline1 −2.0 −1.9 −0.4 Difference from liraglutide1 [95% CI] −0.1 [−0.4; 0.1] - - Difference from placebo1 [95% CI] −1.6 [−2.0; −1.3]§ - - Body weight (kg) Baseline 92.9 95.5 93.2 Change from baseline1 −4.4 −3.1 −0.5 Difference from liraglutide1 [95% CI] −1.2 [−1.9; −0.6]* - - Difference from placebo1 [95% CI] −3.8 [−4.7; −3.0]* - - Week 52 HbA1c (%) Change from baseline1 −1.2 −0.9 −0.2 Difference from liraglutide1 [95% CI] −0.3 [−0.5; −0.1]§ - - Difference from placebo1 [95% CI] −1.0 [−1.2; −0.8]§ - - Patients (%) achieving HbA1c <7.0% 61§,a 55 15 Body weight (kg) Change from baseline1 −4.3 −3.0 −1.0 Difference from liraglutide1 [95% CI] −1.3 [−2.1; −0.5]§ - - Difference from placebo1 [95% CI] −3.3 [−4.3; −2.4]§ - - 1Irrespective of treatment discontinuation or initiation of rescue medication (pattern mixture model using multiple imputation). * p<0.001 (unadjusted 2-sided) for superiority, controlled for multiplicity. § p<0.05, not controlled for multiplicity; for ‘Patients achieving HbA1c <7.0%’, the p-value is for the odds ratio. a vs placebo. PIONEER 5 – Semaglutide vs. placebo, both in combination with basal insulin alone, metformin and basal insulin or metformin and/or sulfonylurea, in patients with moderate renal impairment In a 26-week double-blind trial, 324 patients with type 2 diabetes and moderate renal impairment (eGFR 30-59 ml/min/1.73 m2) were randomised to semaglutide 14 mg or placebo once daily. Trial product was added to the patient’s stable pre-trial antidiabetic regimen. Table 6 Results of a 26-week trial comparing semaglutide with placebo in patients with type 2 diabetes and moderate renal impairment (PIONEER 5) Semaglutide Placebo 14 mg Full analysis set (N) 163 161 HbA1c (%) Baseline 8.0 7.9 Change from baseline1 −1.0 −0.2 Difference from placebo1 [95% CI] −0.8 [−1.0; −0.6]* - Patients (%) achieving HbA1c <7.0% 58§ 23 FPG (mmol/L) Baseline 9.1 9.1 Change from baseline1 −1.5 −0.4 Difference from placebo1 [95% CI] −1.2 [−1.7; −0.6]§ - Body weight (kg) Baseline 91.3 90.4 Change from baseline1 −3.4 −0.9 Difference from placebo1 [95% CI] −2.5 [−3.2; −1.8]* - 1 Irrespective of treatment discontinuation or initiation of rescue medication (pattern mixture model using multiple imputation). * p<0.001 (unadjusted 2-sided) for superiority, controlled for multiplicity. § p<0.05, not controlled for multiplicity; for ‘Patients achieving HbA1c <7.0%’, the p-value is for the odds ratio. PIONEER 7 – Semaglutide vs. sitagliptin, both in combination with metformin, SGLT2 inhibitors, sulfonylurea or thiazolidinediones. Flexible-dose-adjustment trial In a 52-week open-label trial, 504 patients with type 2 diabetes were randomised to semaglutide (flexible dose adjustment of 3 mg, 7 mg, and 14 mg once daily) or sitagliptin 100 mg once daily, all in combination with 1-2 oral glucose-lowering medicinal products (metformin, SGLT2 inhibitors, sulfonylurea or thiazolidinediones). The dose of semaglutide was adjusted every 8 weeks based on patient’s glycaemic response and tolerability. The sitagliptin 100 mg dose was fixed. The efficacy and safety of semaglutide were evaluated at week 52. At week 52, the proportion of patients on treatment with semaglutide 3 mg, 7 mg and 14 mg was approximately 10%, 30% and 60%, respectively. Table 7 Results of a 52-week flexible-dose-adjustment trial comparing semaglutide with sitagliptin (PIONEER 7) Semaglutide Sitagliptin Flexible dose 100 mg Full analysis set (N) 253 251 HbA1c (%) Baseline 8.3 8.3 Patients (%) achieving HbA1c <7.0%1 58* 25 Body weight (kg) Baseline 88.9 88.4 Change from baseline1 −2.6 −0.7 Difference from sitagliptin1 [95% CI] −1.9 [−2.6; −1.2]* - 1 Irrespective of treatment discontinuation (16.6% of the patients with semaglutide flexible dose and 9.2% with sitagliptin, where 8.7% and 4.0%, respectively, were due to AEs) or initiation of rescue medication (pattern mixture model using multiple imputation). * p<0.001 (unadjusted 2-sided) for superiority, controlled for multiplicity (for ‘Patients achieving HbA1c <7.0%’, the p-value is for the odds ratio). PIONEER 8 – Semaglutide vs. placebo, both in combination with insulin with or without metformin In a 52-week double-blind trial, 731 patients with type 2 diabetes inadequately controlled on insulin (basal, basal/bolus or premixed) with or without metformin were randomised to semaglutide 3 mg, semaglutide 7 mg, semaglutide 14 mg or placebo once daily. Table 8 Results of a 52-week trial comparing semaglutide with placebo in combination with insulin (PIONEER 8) Semaglutide Semaglutide Placebo 7 mg 14 mg Full analysis set (N) 182 181 184 Week 26 (insulin dose capped to baseline level) HbA1c (%) Baseline 8.2 8.2 8.2 Change from baseline1 −0.9 −1.3 −0.1 Difference from placebo1 [95% CI] −0.9 [−1.1; −0.7]* −1.2 [−1.4; −1.0]* - Patients (%) achieving HbA1c <7.0% 43§ 58§ 7 FPG (mmol/L) Baseline 8.5 8.3 8.3 Change from baseline1 −1.1 −1.3 0.3 Difference from placebo1 [95% CI] −1.4 [−1.9; −0.8]§ −1.6 [−2.2; −1.1]§ - Body weight (kg) Baseline 87.1 84.6 86.0 Change from baseline1 −2.4 −3.7 −0.4 Difference from placebo1 [95% CI] −2.0 [−3.0; −1.0]* −3.3 [−4.2; −2.3]* - Week 52 (uncapped insulin dose)+ HbA1c (%) Change from baseline1 −0.8 −1.2 -0.2 Difference from placebo1 [95% CI] −0.6 [−0.8; −0.4]§ −0.9 [−1.1; −0.7]§ - Patients (%) achieving HbA1c <7.0% 40§ 54§ 9 Body weight (kg) Change from baseline1 −2.0 −3.7 0.5 Difference from placebo1 [95% CI] −2.5 [−3.6; −1.4]§ −4.3 [−5.3; −3.2]§ - 1 Irrespective of treatment discontinuation or initiation of rescue medication (pattern mixture model using multiple imputation). * p<0.001 (unadjusted 2-sided) for superiority, controlled for multiplicity. § p<0.05, not controlled for multiplicity; for ‘Patients achieving HbA1c <7.0%’, the p-value is for the odds ratio. + The total daily insulin dose was statistically significantly lower with semaglutide than with placebo at week 52. Cardiovascular evaluation In a double-blind trial (PIONEER 6), 3,183 patients with type 2 diabetes at high cardiovascular risk were randomised to Rybelsus 14 mg once daily or placebo in addition to standard-of-care. The median observation period was 16 months. The primary endpoint was time from randomisation to first occurrence of a major adverse cardiovascular event (MACE): cardiovascular death, non-fatal myocardial infarction or non-fatal stroke. Patients eligible to enter the trial were: 50 years of age or older and with established cardiovascular disease and/or chronic kidney disease, or 60 years of age or older and with cardiovascular risk factors only. In total, 1,797 patients (56.5%) had established cardiovascular disease without chronic kidney disease, 354 (11.1%) had chronic kidney disease only and 544 (17.1%) had both cardiovascular disease and kidney disease. 488 patients (15.3%) had cardiovascular risk factors only. The mean age at baseline was 66 years, and 68% of the patients were men. The mean duration of diabetes was 14.9 years and the mean BMI was 32.3 kg/m2. Medical history included stroke (11.7%) and myocardial infarction (36.1%). The total number of first MACE was 137: 61 (3.8%) with semaglutide and 76 (4.8%) with placebo. The analysis of time to first MACE resulted in a HR of 0.79 [0.57; 1.11]95% CI. Proportion of subjects (%) HR: 0.79 95% CI 0.57; 1.11 Number of subjects at risk Rybelsus Placebo Time from randomisation (week) Rybelsus Placebo Cumulative incidence plot of primary outcome (a composite of cardiovascular death, nonfatal myocardial infarction, or nonfatal stroke) with non-cardiovascular death as competing risk. Abbreviations: CI: Confidence interval, HR: Hazard ratio Figure 1 Cumulative incidence of first occurrence of MACE in PIONEER 6 The treatment effect for the primary composite endpoint and its components in the PIONEER 6 trial is shown in Figure 2. Hazard Ratio Rybelsus Placebo (95% CI) N (%) N (%) 1591 1592 FAS (100) (100) 0.79 61 76 Primary endpoint – MACE (0.57-1.11) (3.8) (4.8) Components of MACE 0.49 15 30 Cardiovascular death (1.9) (0.27-0.92) (0.9) 0.74 12 16 Non-fatal stroke (0.35-1.57) (0.8) (1.0) 1.18 37 31 Non-fatal myocardial infarction (0.73-1.90) (2.3) (1.9) Other secondary endpoints 0.51 23 45 All cause death (2.8) (0.31-0.84) (1.4) 0.2 1 5 Favours Rybelsus Favours placebo Figure 2 Treatment effect for the primary composite endpoint, its components and all cause death (PIONEER 6) Body weight By end-of-treatment, 27-45% of the patients had achieved a weight loss of ≥5% and 6-16% had achieved a weight loss of ≥10% with semaglutide, compared with 12-39% and 2-8%, respectively, with the active comparators. Blood pressure Treatment with semaglutide had reduced systolic blood pressure by 2-7 mmHg.
Pharmacokinetic Properties
5.2 Pharmacokinetic properties Absorption Orally administered semaglutide has a low absolute bioavailability and a variable absorption. Daily administration according to the recommended posology in combination with a long half-life reduces day-to-day fluctuation of the exposure. The pharmacokinetics of semaglutide have been extensively characterised in healthy subjects and patients with type 2 diabetes. Following oral administration, maximum plasma concentration of semaglutide occurred approximately 1 hour post dose. Steady-state exposure was reached after 4– 5 weeks of once-daily administration. In patients with type 2 diabetes, the average steady-state concentrations were approximately 6.7 nmol/L and 14.6 nmol/L with semaglutide 7 mg and 14 mg, respectively; with 90% of subjects treated with semaglutide 7 mg having an average concentration between 1.7 and 22.7 nmol/L and 90% of subjects treated with semaglutide 14 mg having an average concentration between 3.7 and 41.3 nmol/L. Systemic exposure of semaglutide increased in a dose-proportional manner. Based on in vitro data, salcaprozate sodium facilitates absorption of semaglutide. The absorption of semaglutide predominantly occurs in the stomach. The estimated bioavailability of semaglutide is approximately 1% following oral administration. The between-subject variability in absorption was high (coefficient of variation was approximately 100%). The estimation of the within-subject variability in bioavailability was not reliable. Absorption of semaglutide is decreased if taken with food or large volumes of water. A longer post-dose fasting period results in higher absorption. Distribution The estimated absolute volume of distribution is approximately 8 L in subjects with type 2 diabetes. Semaglutide is extensively bound to plasma proteins (>99%). Biotransformation Semaglutide is metabolised through proteolytic cleavage of the peptide backbone and sequential beta-oxidation of the fatty acid sidechain. The enzyme neutral endopeptidase (NEP) is expected to be involved in the metabolism of semaglutide. Elimination The primary excretion routes of semaglutide-related material are via the urine and faeces. Approximately 3% of the absorbed dose is excreted as intact semaglutide via the urine. With an elimination half-life of approximately 1 week, semaglutide will be present in the circulation for about 5 weeks after the last dose. The clearance of semaglutide in patients with type 2 diabetes is approximately 0.04 L/h. Switching between oral and subcutaneous administration The effect of switching between oral and subcutaneous semaglutide cannot easily be predicted because of the high pharmacokinetic variability of oral semaglutide. Exposure after oral semaglutide 14 mg once daily is comparable to subcutaneous semaglutide 0.5 mg once weekly. An oral dose equivalent to 1 mg of subcutaneous semaglutide has not been established. Special populations Elderly Age had no effect on the pharmacokinetics of semaglutide based on data from clinical trials, which studied patients up to 92 years of age. Gender Gender had no clinically meaningful effects on the pharmacokinetics of semaglutide. Race and ethnicity Race (White, Black or African-American, Asian) and ethnicity (Hispanic or Latino, not Hispanic or Latino) had no effect on the pharmacokinetics of semaglutide. Body weight Body weight had an effect on the exposure of semaglutide. Higher body weight was associated with lower exposure. Semaglutide provided adequate systemic exposure over the body weight range of 40-188 kg evaluated in the clinical trials. Renal impairment Renal impairment did not impact the pharmacokinetics of semaglutide in a clinically relevant manner. The pharmacokinetics of semaglutide were evaluated in patients with mild, moderate or severe renal impairment and patients with end-stage renal disease on dialysis compared with subjects with normal renal function in a study with 10 consecutive days of once-daily doses of semaglutide. This was also shown for subjects with type 2 diabetes and renal impairment based on data from phase 3a studies. Hepatic impairment Hepatic impairment did not impact the pharmacokinetics of semaglutide in a clinically relevant manner. The pharmacokinetics of semaglutide were evaluated in patients with mild, moderate or severe hepatic impairment compared with subjects with normal hepatic function in a study with 10 consecutive days of once-daily doses of semaglutide. Upper GI tract disease Upper GI tract disease (chronic gastritis and/or gastroesophageal reflux disease) did not impact the pharmacokinetics of semaglutide in a clinically relevant manner. The pharmacokinetics were evaluated in patients with type 2 diabetes with or without upper GI tract disease dosed for 10 consecutive days with once-daily doses of semaglutide. This was also shown for subjects with type 2 diabetes and upper GI tract disease based on data from phase 3a studies. Paediatric population Semaglutide has not been studied in paediatric patients and is not indicated in this population.

שימוש לפי פנקס קופ''ח כללית 1994
לא צוין
תאריך הכללה מקורי בסל
לא צוין
הגבלות
לא צוין
מידע נוסף
עלון מידע לצרכן
01.08.21 - עלון לצרכן אנגלית 01.08.21 - עלון לצרכן עברית 01.08.21 - עלון לצרכן ערבית 11.10.22 - עלון לצרכן אנגלית 18.09.22 - עלון לצרכן עברית 11.10.22 - עלון לצרכן ערבית 08.09.23 - עלון לצרכן אנגלית 07.09.23 - עלון לצרכן עברית 08.09.23 - עלון לצרכן ערבית 13.11.23 - עלון לצרכן עברית 23.01.24 - עלון לצרכן אנגלית 23.01.24 - עלון לצרכן ערבית 22.05.24 - עלון לצרכן עברית 02.08.24 - עלון לצרכן עברית 16.08.24 - עלון לצרכן אנגלית 16.08.24 - עלון לצרכן ערבית 15.11.24 - עלון לצרכן עברית 27.04.21 - החמרה לעלון 18.09.22 - החמרה לעלון 07.09.23 - החמרה לעלון 12.05.24 - החמרה לעלון 16.11.24 - החמרה לעלוןלתרופה במאגר משרד הבריאות
ריבלסוס 3 מ"ג