Quest for the right Drug
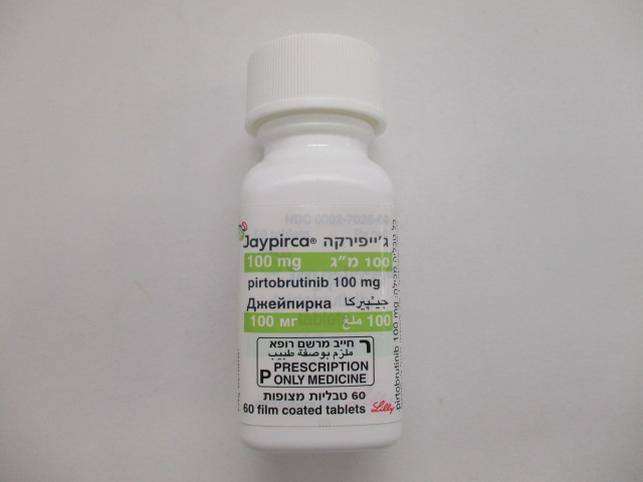
ג'ייפירקה 100 מ"ג JAYPIRCA 100 MG (PIRTOBRUTINIB)
תרופה במרשם
תרופה בסל
נרקוטיקה
ציטוטוקסיקה
צורת מתן:
פומי : PER OS
צורת מינון:
טבליות מצופות פילם : FILM COATED TABLETS
עלון לרופא
מינוניםPosology התוויות
Indications תופעות לוואי
Adverse reactions התוויות נגד
Contraindications אינטראקציות
Interactions מינון יתר
Overdose הריון/הנקה
Pregnancy & Lactation אוכלוסיות מיוחדות
Special populations תכונות פרמקולוגיות
Pharmacological properties מידע רוקחי
Pharmaceutical particulars אזהרת שימוש
Special Warning עלון לרופא
Physicians Leaflet
Pharmacological properties : תכונות פרמקולוגיות
Pharmacodynamic Properties
12.2 Pharmacodynamics At the recommended dosage of 200 mg once daily, pirtobrutinib trough concentrations exceeded the BTK IC96. BTK occupancy is maintained throughout the dosing interval, regardless of the intrinsic rate of BTK turnover. Cardiac Electrophysiology The effect of a single 900 mg dose of pirtobrutinib (equivalent to approximately 2 times higher than the concentrations achieved at steady state at the recommended dosage of 200 mg once daily) on the QTc interval was evaluated in a placebo-controlled and positive-controlled study in 30 healthy subjects. Pirtobrutinib had no clinically meaningful effect on the change in QTcF interval (i.e., > 10 ms) and there was no relationship between pirtobrutinib exposure and change in QTc interval.
Pharmacokinetic Properties
12.3 Pharmacokinetics The pharmacokinetics of pirtobrutinib were characterized in healthy subjects and in patients with cancer. Pirtobrutinib exposure (AUC) and Cmax increases proportionally following single oral doses ranging from 300 mg to 800 mg (1.5 to 4 times the approved recommended dosage) and once daily doses ranging from 25 – 300 mg (0.125 to 1.5 times the recommended dosage). Steady state was achieved within 5 days of once daily dosing, and the mean (CV%) accumulation ratio was 1.63 (26.7%) based on AUC after administration of 200 mg dosages. Following administration of the recommended dosage, the geometric mean (CV%) steady-state AUC and Cmax of pirtobrutinib were 90300 h*ng/mL (40%) and 6380 ng/mL (26%), respectively. The geometric mean (CV%) AUC0-24 and Cmax of pirtobrutinib on Cycle 1 Day 8 were 81800 h*ng/mL (66.6%) and 3670 ng/mL (89.5%), respectively. Absorption The absolute bioavailability of pirtobrutinib after a single oral 200 mg dose is 85.5% (range 75.9% to 90.9%). The median time (range) to reach peak plasma concentration (tmax) is approximately 2 hours (0.833 to 4.15 hours). Effect of Food No clinically significant differences in the pharmacokinetics of pirtobrutinib were observed following administration of a high-fat, high-calorie meal (approximately 800 to 1000 calories with 150 calories from protein, 250 calories from carbohydrate, and 500 to 600 calories from fat) to healthy subjects. A high-fat meal decreased the Cmax of pirtobrutinib by 23% and delayed tmax by 1 hour. There was no effect on pirtobrutinib AUC. Distribution The mean apparent central volume of distribution of pirtobrutinib is 34.1 L. Human protein binding of pirtobrutinib is 96% and is independent of concentration in vitro. Mean blood-to-plasma ratio is 0.79. Elimination The effective half-life of pirtobrutinib is approximately 19 hours and the mean (CV%) apparent clearance is 2.05 L/h (37.2%). Metabolism Pirtobrutinib is primarily metabolized by CYP3A4 and direct glucuronidation by UGT1A8 and UGT1A9, in vitro. Excretion Following a single radiolabeled dose of pirtobrutinib 200 mg to healthy subjects, 37% of the dose was recovered in feces (18% unchanged) and 57% in urine (10% unchanged). Specific Populations There were no clinically significant differences in the pharmacokinetics of pirtobrutinib based on age (range 22 – 95 years), sex, race/ethnicity (White 84%, Asian 7%), body weight (range 35.7 – 152 kg), mild (total bilirubin ≤ upper limit of normal (ULN) and aspartate aminotransferase (AST) > ULN or total bilirubin > 1 to 1.5 × ULN and any AST), moderate (total bilirubin > 1.5 to 3 × ULN and any AST), or severe (total bilirubin > 3 × ULN and any AST) hepatic impairment. The effect of other races/ethnicities on the pharmacokinetics of pirtobrutinib is unknown. Patients with Renal Impairment Following a single 200 mg oral dose, the AUC of pirtobrutinib in subjects with severe renal impairment (eGFR 15-29 mL/min) increased by 62% and mean unbound AUC increased by 68% compared to healthy subjects with normal renal function. There were no clinically significant differences in the pharmacokinetics of pirtobrutinib in subjects with mild (eGFR 60-89 mL/min) or moderate renal impairment (eGFR 30-59 mL/min). The effect of renal impairment requiring dialysis on the pharmacokinetics of pirtobrutinib is unknown. Drug Interaction Studies Clinical Studies and Model-Informed Approaches Strong CYP3A Inhibitors: Co-administration of a single 200 mg dose of pirtobrutinib with itraconazole (strong CYP3A inhibitor) increased AUC of pirtobrutinib by 49%. Moderate CYP3A Inhibitors: Verapamil and diltiazem (moderate CYP3A inhibitors) are predicted to increase the AUC of pirtobrutinib by 30% and 20%, respectively. Strong CYP3A inducers: Coadministration of a single 200 mg dose of pirtobrutinib with rifampin (strong CYP3A inducer) decreased the AUC of pirtobrutinib by 71%. Moderate CYP3A Inducers: Efavirenz and bosentan (moderate CYP3A inducers) are predicted to decrease the AUC of pirtobrutinib by 49% and 27%, respectively. Gastric Reducing Agents: No clinically significant differences in pirtobrutinib pharmacokinetics were observed when co-administered with omeprazole (a proton pump inhibitor). P-glycoprotein (P-gp) inhibitors: No clinically significant differences in pirtobrutinib pharmacokinetics were observed when co-administered with itraconazole (P-gp inhibitor). CYP3A Substrates: Pirtobrutinib increased the AUC and Cmax of orally administered midazolam (sensitive CYP3A substrate) by 70% and 58%, respectively. Pirtobrutinib did not have a clinically meaningful effect on the exposure of intravenously administered midazolam. CYP2C8 Substrates: Pirtobrutinib increased the AUC and Cmax of repaglinide (sensitive CYP2C8 substrate) by 130% and 98%, respectively. CYP2C19 Substrates: Pirtobrutinib increased the AUC and Cmax of omeprazole (sensitive CYP2C19 substrate) by 56% and 49%, respectively. P-gp Substrates: A single 200 mg dose of pirtobrutinib increased the AUC and Cmax of digoxin (sensitive P-gp substrate) by 17% and 51%, respectively. Multiple doses of pirtobrutinib (200 mg daily) further increased the AUC and Cmax of digoxin (sensitive P-gp substrate) up to 35% and 55%, respectively. BCRP Substrates: Multiple doses of pirtobrutinib (200 mg daily) increased the AUC and Cmax of rosuvastatin (sensitive BCRP substrate) by 140% and 146%, respectively. CYP1A2 and CYP2C9 Substrates: Pirtobrutinib did not have a clinically meaningful effect on the exposures of caffeine (sensitive CYP1A2 substrate) or S-warfarin (moderate sensitive CYP2C9 substrate). In Vitro Studies Cytochrome P450 (CYP) Enzymes: Pirtobrutinib inhibits CYP2C8, CYP2C9, CYP3A, CYP1A2, CYP2B6, CYP2C19, and CYP2D6. Pirtobrutinib induces CYP3A4, CYP3A5, CYP2B6, and CYP2C19. Transporter Systems: Pirtobrutinib inhibits P-gp and BCRP, but not OAT1, OAT3, OCT1, OCT2, OATP1B1, OATP1B3, MATE1, or MATE2-K. Pirtobrutinib is not a substrate of the hepatic transporters. Pirtobrutinib is a substrate of P-gp and BCRP, but not OCT1, OATP1B1, OATP1B3, or BSEP.

שימוש לפי פנקס קופ''ח כללית 1994
לא צוין
תאריך הכללה מקורי בסל
לא צוין
הגבלות
לא צוין
מידע נוסף
עלון מידע לצרכן
30.01.24 - עלון לצרכן עברית 14.02.24 - עלון לצרכן עברית 21.03.24 - עלון לצרכן אנגלית 21.03.24 - עלון לצרכן ערבית 20.06.24 - עלון לצרכן עברית 02.08.24 - עלון לצרכן אנגלית 11.08.24 - עלון לצרכן ערבית 10.10.24 - עלון לצרכן עברית 11.11.24 - עלון לצרכן אנגלית 11.11.24 - עלון לצרכן ערבית 20.06.24 - החמרה לעלוןלתרופה במאגר משרד הבריאות
ג'ייפירקה 100 מ"ג