Quest for the right Drug
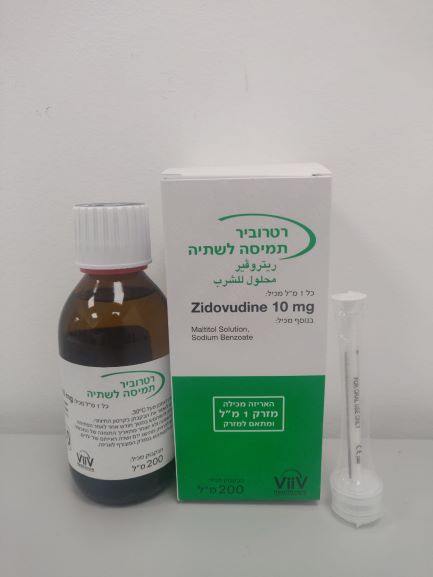
רטרוביר תמיסה לשתיה RETROVIR ORAL SOLUTION (ZIDOVUDINE)
תרופה במרשם
תרופה בסל
נרקוטיקה
ציטוטוקסיקה
צורת מתן:
פומי : PER OS
צורת מינון:
תמיסה : SOLUTION
עלון לרופא
מינוניםPosology התוויות
Indications תופעות לוואי
Adverse reactions התוויות נגד
Contraindications אינטראקציות
Interactions מינון יתר
Overdose הריון/הנקה
Pregnancy & Lactation אוכלוסיות מיוחדות
Special populations תכונות פרמקולוגיות
Pharmacological properties מידע רוקחי
Pharmaceutical particulars אזהרת שימוש
Special Warning עלון לרופא
Physicians Leaflet
Special Warning : אזהרת שימוש
4.4 Special warnings and precautions for use Retrovir is not a cure for HIV infection or AIDS. Patients receiving Retrovir or any other antiretroviral therapy may continue to develop opportunistic infections and other complications of HIV infection. The concomitant use of rifampicin or stavudine with zidovudine should be avoided (see section 4.5). Haematological Adverse Reactions: Anaemia (usually not observed before six weeks of Retrovir therapy but occasionally occurring earlier), neutropenia (usually not observed before four weeks’ therapy but sometimes occurring earlier) and leucopenia (usually secondary to neutropenia) can be expected to occur in patients receiving Retrovir; These occurred more frequently at higher dosages (1200-1500 mg/day) and in patients with poor bone marrow reserve prior to treatment, particularly with advanced HIV disease (see section 4.8). Haematological parameters should be carefully monitored. For patients with advanced symptomatic HIV disease it is generally recommended that blood tests are performed at least every two weeks for the first three months of therapy and at least monthly thereafter. Depending on the overall condition of the patient, blood tests may be performed less often, for example every 1 to 3 months. If the haemoglobin level falls to between 7.5 g/dl (4.65 mmol/l) and 9 g/dl (5.59 mmol/l) or the neutrophil count falls to between 0.75 x 109/l and 1.0 x 109/l, the daily dosage may be reduced until there is evidence of marrow recovery; alternatively, recovery may be enhanced by brief (2-4 weeks) interruption of Retrovir therapy. Marrow recovery is usually observed within 2 weeks after which time Retrovir therapy at a reduced dosage may be reinstituted. In patients with significant anaemia, dosage adjustments do not necessarily eliminate the need for transfusions (see section 4.3). Lactic acidosis: lactic acidosis usually associated with hepatomegaly and hepatic steatosis has been reported with the use of zidovudine. Early symptoms (symptomatic hyperlactatemia) include benign digestive symptoms (nausea, vomiting and abdominal pain), non-specific malaise, loss of appetite, weight loss, respiratory symptoms (rapid and/or deep breathing) or neurological symptoms (including motor weakness). Lactic acidosis has a high mortality and may be associated with pancreatitis, liver failure, or renal failure. Lactic acidosis generally occurred after a few or several months of treatment. Treatment with zidovudine should be discontinued in the setting of symptomatic hyperlactatemia and metabolic/lactic acidosis, progressive hepatomegaly, or rapidly elevating aminotransferase levels. Caution should be exercised when administering zidovudine to any patient (particularly obese women) with hepatomegaly, hepatitis or other known risk factors for liver disease and hepatic steatosis (including certain medicinal products and alcohol). Patients co-infected with hepatitis C and treated with alpha interferon and ribavirin may constitute a special risk. Patients at increased risk should be followed closely. Mitochondrial dysfunction following exposure in utero: Nucleoside and nucleotide analogues may impact mitochondrial function to a variable degree, which is most pronounced with stavudine, didanosine and zidovudine. There have been reports of mitochondrial dysfunction in HIV-negative infants exposed in utero and/or post-natally to nucleoside analogues; these have predominantly concerned treatment with regimens containing zidovudine. The main adverse reactions reported are haematological disorders (anaemia, neutropenia) and metabolic disorders (hyperlactatemia, hyperlipasaemia). These events have often been transitory. Late- onset neurological disorders have been reported rarely (hypertonia, convulsion, abnormal behaviour). Whether such neurological disorders are transient or permanent is currently unknown. These findings should be considered for any child exposed in utero to nucleoside and nucleotide analogues, who presents with severe clinical findings of unknown etiology, particularly neurologic findings. These findings do not affect current recommendations to use antiretroviral therapy in pregnant women to prevent vertical transmission of HIV. Lipoatrophy: Treatment with zidovudine has been associated with loss of subcutaneous fat, which has been linked to mitochondrial toxicity. The incidence and severity of lipoatrophy are related to cumulative exposure. This fat loss, which is most evident in the face, limbs and buttocks, may not be reversible when switching to a zidovudine-free regimen. Patients should be regularly assessed for signs of lipoatrophy during therapy with zidovudine and zidovudine- containing products (Combivir and Trizivir). Therapy should be switched to an alternative regimen if there is suspicion of lipoatrophy development. Weight and metabolic parameters: An increase in weight and in levels of blood lipids and glucose may occur during antiretroviral therapy. Such changes may in part be linked to disease control and life style. For lipids, there is in some cases evidence for a treatment effect, while for weight gain there is no strong evidence relating this to any particular treatment. For monitoring of blood lipids and glucose reference is made to established HIV treatment guidelines. Lipid disorders should be managed as clinically appropriate. Liver disease: Zidovudine clearance in patients with mild hepatic impairment without cirrhosis [Child-Pugh scores of 5-6] is similar to that seen in healthy subjects, therefore no zidovudine dose adjustment is required. In patients with moderate to severe liver disease [Child-Pugh scores of 7-15], specific dosage recommendations cannot be made due to the large variability in zidovudine exposure observed, therefore zidovudine use in this group of patients is not recommended. Patients with chronic hepatitis B or C and treated with combination antiretroviral therapy are at an increased risk of severe and potentially fatal hepatic adverse events. In case of concomitant antiviral therapy for hepatitis B or C, please also refer to the relevant product information for these medicinal products. Patients with pre-existing liver dysfunction, including chronic active hepatitis, have an increased frequency of liver function abnormalities during combination antiretroviral therapy and should be monitored according to standard practice. If there is evidence of worsening liver disease in such patients, interruption or discontinuation of treatment must be considered (see section 4.2). Immune Reactivation Syndrome: In HIV-infected patients with severe immune deficiency at the time of institution of combination antiretroviral therapy (CART), an inflammatory reaction to asymptomatic or residual opportunistic pathogens may arise and cause serious clinical conditions, or aggravation of symptoms. Typically, such reactions have been observed within the first few weeks or months of initiation of CART. Relevant examples are cytomegalovirus retinitis, generalized and/or focal mycobacterial infections and Pneumocystis jirovecii pneumonia. Any inflammatory symptoms should be evaluated and treatment instituted when necessary. Autoimmune disorders (such as Graves’ disease and autoimmune hepatitis) have also been reported to occur in the setting of immune reactivation; however, the reported time to onset is more variable and can occur many months after initiation of treatment. Patients should be cautioned about the concomitant use of self-administered medications (see section 4.5). Use in Elderly and in Patients with Renal or Hepatic Impairment: see section 4.2. Osteonecrosis: Although the etiology is considered to be multifactorial (including corticosteroid use, alcohol consumption, severe immunosuppression, higher body mass index), cases of osteonecrosis have been reported particularly in patients with advanced HIV- disease and/or long-term exposure to combination antiretroviral therapy (CART). Patients should be advised to seek medical advice if they experience joint aches and pain, joint stiffness or difficulty in movement. Patients co-infected with hepatitis C virus: The concomitant use of ribavirin with zidovudine is not recommended due to an increased risk of anaemia (see section 4.5). Excipients: Maltitol: Patients with rare hereditary problems of fructose intolerance should not take this medicine. Sodium benzoate: Increase in bilirubinaemia following its displacement from albumin may increase neonatal jaundice which may develop into kernicterus (non-conjugated bilirubin deposits on the brain tissue). Sodium: This medicinal product contains less than 1 mmol sodium (23 mg) per dosage unit, that is to say essentially ‘sodium-free’. Propylene glycol: Co-administration with any substrate for alcohol dehydrogenase such as ethanol may induce serious adverse effects in neonates
Effects on Driving
4.7 Effects on ability to drive and use machines There have been no studies to investigate the effect of Retrovir on driving performance or the ability to operate machinery. Furthermore, a detrimental effect on such activities cannot be predicted from the pharmacology of the drug. Nevertheless, the clinical status of the patient and the adverse reaction profile of Retrovir should be borne in mind when considering the patient’s ability to drive or operate machinery.

שימוש לפי פנקס קופ''ח כללית 1994
לא צוין
תאריך הכללה מקורי בסל
01/01/1995
הגבלות
תרופה מוגבלת לרישום ע'י רופא מומחה או הגבלה אחרת
מידע נוסף
עלון מידע לצרכן
13.03.18 - עלון לצרכן 17.01.19 - עלון לצרכן 30.05.22 - עלון לצרכן אנגלית 30.05.22 - עלון לצרכן עברית 30.05.22 - עלון לצרכן ערבית 02.11.22 - עלון לצרכן עברית 27.02.23 - עלון לצרכן אנגלית 27.02.23 - עלון לצרכן עברית 27.02.23 - עלון לצרכן ערבית 20.01.14 - החמרה לעלון 25.03.14 - החמרה לעלון 22.08.17 - החמרה לעלון 07.02.19 - החמרה לעלון 10.03.19 - החמרה לעלון 01.03.22 - החמרה לעלון 23.12.15 - החמרה לעלוןלתרופה במאגר משרד הבריאות
רטרוביר תמיסה לשתיה