Quest for the right Drug
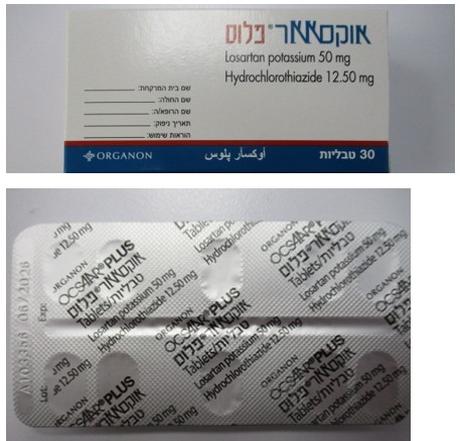
אוקסאאר פלוס OCSAAR PLUS (HYDROCHLOROTHIAZIDE, LOSARTAN POTASSIUM)
תרופה במרשם
תרופה בסל
נרקוטיקה
ציטוטוקסיקה
צורת מתן:
פומי : PER OS
צורת מינון:
טבליה : TABLETS
עלון לרופא
מינוניםPosology התוויות
Indications תופעות לוואי
Adverse reactions התוויות נגד
Contraindications אינטראקציות
Interactions מינון יתר
Overdose הריון/הנקה
Pregnancy & Lactation אוכלוסיות מיוחדות
Special populations תכונות פרמקולוגיות
Pharmacological properties מידע רוקחי
Pharmaceutical particulars אזהרת שימוש
Special Warning עלון לרופא
Physicians Leaflet
Pharmacological properties : תכונות פרמקולוגיות
Pharmacodynamic Properties
5.1 Pharmacodynamic properties Pharmacotherapeutic group: Angiotensin II antagonists and diuretics, ATC code: C09DA01 Losartan-Hydrochlorothiazide The components of OCSAAR PLUS have been shown to have an additive effect on blood pressure reduction, reducing blood pressure to a greater degree than either component alone. This effect is thought to be a result of the complimentary actions of both components. Further, as a result of its diuretic effect, hydrochlorothiazide increases plasma renin activity, increases aldosterone secretion, decreases serum potassium, and increases the levels of angiotensin II. Administration of losartan blocks all the physiologically relevant actions of angiotensin II and through inhibition of aldosterone could tend to attenuate the potassium loss associated with the diuretic. Losartan has been shown to have a mild and transient uricosuric effect. Hydrochlorothiazide has been shown to cause modest increases in uric acid; the combination of losartan and hydrochlorothiazide tends to attenuate the diuretic-induced hyperuricemia. The antihypertensive effect of OCSAAR PLUS is sustained for a 24-hour period. In clinical studies of at least one year's duration, the antihypertensive effect was maintained with continued therapy. Despite the significant decrease in blood pressure, administration of OCSAAR PLUS had no clinically significant effect on heart rate. In clinical trials, after 12 weeks of therapy with losartan 50 mg/hydrochlorothiazide 12.5 mg, trough sitting diastolic blood pressure was reduced by an average of up to 13.2 mmHg. OCSAAR PLUS is effective in reducing blood pressure in males and females, blacks and non-blacks and in younger (<65 years) and older (≥65 years) patients and is effective in all degrees of hypertension. Losartan Losartan is a synthetically produced oral angiotensin-II receptor (type AT1) antagonist. Angiotensin II, a potent vasoconstrictor, is the primary active hormone of the renin-angiotensin system and an important determinant of the pathophysiology of hypertension. Angiotensin II binds to the AT1 receptor found in many tissues (e.g. vascular smooth muscle, adrenal gland, kidneys and the heart) and elicits several important biological actions, including vasoconstriction and the release of aldosterone. Angiotensin II also stimulates smooth-muscle cell proliferation. Losartan selectively blocks the AT1 receptor. In vitro and in vivo losartan and its pharmacologically active carboxylic acid metabolite E-3174 block all physiologically relevant actions of angiotensin II, regardless of the source or route of its synthesis. Losartan does not have an agonist effect nor does it block other hormone receptors or ion channels important in cardiovascular regulation. Furthermore, losartan does not inhibit ACE (kininase II), the enzyme that degrades bradykinin. Consequently, there is thus no increase in bradykinin-mediated undesirable effects. During the administration of losartan the removal of the angiotensin II negative feedback on renin secretion leads to increased plasma-renin activity (PRA). Increase in the PRA leads to an increase in angiotensin II in plasma. Despite these increases, antihypertensive activity and suppression of the plasma aldosterone concentration are maintained, indicating effective angiotensin II receptor blockade. After the discontinuation of losartan, PRA and angiotensin II values fell within 3 days to the baseline values. Both losartan and its principal active metabolite have a far greater affinity for the AT1 receptor than for the AT2 receptor. The active metabolite is 10- to 40-times more active than losartan on a weight for weight basis. In a study specifically designed to assess the incidence of cough in patients treated with losartan as compared to patients treated with ACE inhibitors, the incidence of cough reported by patients receiving losartan or hydrochlorothiazide was similar and was significantly less than in patients treated with an ACE inhibitor. In addition, in an overall analysis of 16 double-blind clinical trials in 4131 patients, the incidence of spontaneously reported cough in patients treated with losartan was similar (3.1%) to that of patients treated with placebo (2.6%) or hydrochlorothiazide (4.1%), whereas the incidence with ACE inhibitors was 8.8%. In nondiabetic hypertensive patients with proteinuria, the administration of losartan potassium significantly reduces proteinuria, fractional excretion of albumin and IgG. Losartan maintains glomerular filtration rate and reduces filtration fraction. Generally losartan causes a decrease in serum uric acid (usually <0.4 mg/dL) which was persistent in chronic therapy. Losartan has no effect on autonomic reflexes and no sustained effect on plasma norepinephrine. In patients with left ventricular failure, 25 mg and 50 mg doses of losartan produced positive haemodynamic and neurohormonal effects characterized by an increase in cardiac index and decreases in pulmonary capillary wedge pressure, systemic vascular resistance, mean systemic arterial pressure and heart rate and a reduction in circulating levels of aldosterone and norepinephrine, respectively. The occurrence of hypotension was dose related in these heart failure patients. Hypertension Studies In controlled clinical studies, once-daily administration of losartan to patients with mild to moderate essential hypertension produced statistically significant reductions in systolic and diastolic blood pressure. Measurement of blood pressure 24 hours post-dose relative to 5-6 hours post-dose demonstrated blood pressure reduction over 24 hours; the natural diurnal rhythm was retained. Blood pressure reduction at the end of the dosing interval was 70 – 80% of the effect seen 5-6 hours post- dose. Discontinuation of losartan in hypertensive patients did not result in an abrupt rise in blood pressure (rebound). Despite the marked decrease in blood pressure, losartan had no clinically significant effect on heart rate. Losartan is equally effective in males and females, and in younger (below the age of 65 years) and older hypertensive patients. LIFE Study The Losartan Intervention For Endpoint reduction in hypertension (LIFE) study was a randomised, triple-blind, active-controlled study in 9193 hypertensive patients aged 55 to 80 years with ECG- documented left ventricular hypertrophy. Patients were randomised to once daily losartan 50 mg or once daily atenolol 50 mg. If goal blood pressure (<140/90 mmHg) was not reached, hydrochlorothiazide (12.5 mg) was added first and, if needed, the dose of losartan or atenolol was then increased to 100 mg once daily. Other antihypertensives, with the exception of ACE inhibitors, angiotensin II antagonists or beta-blockers were added if necessary to reach the goal blood pressure. The mean length of follow up was 4.8 years. The primary endpoint was the composite of cardiovascular morbidity and mortality as measured by a reduction in the combined incidence of cardiovascular death, stroke and myocardial infarction. Blood pressure was significantly lowered to similar levels in the two groups. Treatment with losartan resulted in a 13.0% risk reduction (p=0.021, 95% confidence interval 0.77-0.98) compared with atenolol for patients reaching the primary composite endpoint. This was mainly attributable to a reduction of the incidence of stroke. Treatment with losartan reduced the risk of stroke by 25% relative to atenolol (p=0.001, 95% confidence interval 0.63-0.89). The rates of cardiovascular death and myocardial infarction were not significantly different between the treatment groups. Dual Blockade of the renin-angiotensin-aldosterone system (RAAS) Two large randomised, controlled trials (ONTARGET (ONgoing Telmisartan Alone and in combination with Ramipril Global Endpoint Trial) and VA NEPHRON-D (The Veterans Affairs Nephropathy in Diabetes) have examined the use of the combination of an ACE-inhibitor with an angiotensin II receptor blocker. ONTARGET was a study conducted in patients with a history of cardiovascular or cerebrovascular disease, or type 2 diabetes mellitus accompanied by evidence of end-organ damage. VA NEPHRON-D was a study in patients with type 2 diabetes mellitus and diabetic nephropathy. These studies have shown no significant beneficial effect on renal and/or cardiovascular outcomes and mortality, while an increased risk of hyperkalaemia, acute kidney injury and/or hypotension as compared to monotherapy was observed. Given their similar pharmacodynamic properties, these results are also relevant for other ACE-inhibitors and angiotensin II receptor blockers. ACE-inhibitors and angiotensin II receptor blockers should therefore not be used concomitantly in patients with diabetic nephropathy. ALTITUDE (Aliskiren Trial in Type 2 Diabetes Using Cardiovascular and Renal Disease Endpoints) was a study designed to test the benefit of adding aliskiren to a standard therapy of an ACE-inhibitor or an angiotensin II receptor blocker in patients with type 2 diabetes mellitus and chronic kidney disease, cardiovascular disease, or both. The study was terminated early because of an increased risk of adverse outcomes. Cardiovascular death and stroke were both numerically more frequent in the aliskiren group than in the placebo group and adverse events and serious adverse events of interest (hyperkalaemia, hypotension and renal dysfunction) were more frequently reported in the aliskiren group than in the placebo group. Hydrochlorothiazide Hydrochlorothiazide is a thiazide diuretic. The mechanism of the antihypertensive effect of thiazide diuretics is not fully known. Thiazides affect the renal tubular mechanisms of electrolyte reabsorption, directly increasing excretion of sodium and chloride in approximately equivalent amounts. The diuretic action of hydrochlorothiazide reduces plasma volume, increases plasma renin activity and increases aldosterone secretion, with consequent increases in urinary potassium and bicarbonate loss, and decreases in serum potassium. The renin-aldosterone link is mediated by angiotensin II and therefore co-administration of an angiotensin II receptor antagonist tends to reverse the potassium loss associated with thiazide diuretics. After oral use, diuresis begins within 2 hours, peaks in about 4 hours and lasts about 6 to 12 hours the antihypertensive effect persists for up to 24 hours. Non-melanoma skin cancer: Based on available data from epidemiological studies, cumulative dose-dependent association between hydrochlorothiazide and NMSC has been observed. One study included a population comprised of 71,533 cases of BCC and of 8,629 cases of SCC matched to 1,430,833 and 172,462 population controls, respectively. High hydrochlorothiazide use (≥50,000 mg cumulative) was associated with an adjusted OR of 1.29 (95% CI: 1.23-1.35) for BCC and 3.98 (95% CI: 3.68-4.31) for SCC. A clear cumulative dose response relationship was observed for both BCC and SCC. Another study showed a possible association between lip cancer (SCC) and exposure to hydrochlorothiazide: 633 cases of lip cancer were matched with 63,067 population controls, using a risk-set sampling strategy. A cumulative dose-response relationship was demonstrated with an adjusted OR 2.1 (95% CI: 1.7-2.6) increasing to OR 3.9 (3.0-4.9) for high use (~25,000 mg) and OR 7.7 (5.7-10.5) for the highest cumulative dose (~100,000 mg) (see also section 4.4).
Pharmacokinetic Properties
5.2 Pharmacokinetic properties Absorption Losartan Following oral administration, losartan is well absorbed and undergoes first-pass metabolism, forming an active carboxylic acid metabolite and other inactive metabolites. The systemic bioavailability of losartan tablets is approximately 33%. Mean peak concentrations of losartan and its active metabolite are reached in 1 hour and in 3-4 hours, respectively. There was no clinically significant effect on the plasma concentration profile of losartan when the drug was administered with a standardized meal. Distribution Losartan Both losartan and its active metabolite are ≥99% bound to plasma proteins, primarily albumin. The volume of distribution of losartan is 34 litres. Studies in rats indicate that losartan crosses the blood- brain barrier poorly, if at all. Hydrochlorothiazide Hydrochlorothiazide crosses the placental but not the blood-brain barrier and is excreted in breast milk. Biotransformation Losartan About 14% of an intravenously- or orally-administered dose of losartan is converted to its active metabolite. Following oral and intravenous administration of 14C-labelled losartan potassium, circulating plasma radioactivity primarily is attributed to losartan and its active metabolite. Minimal conversion of losartan to its active metabolite was seen in about one percent of individuals studied. In addition to the active metabolite, inactive metabolites are formed, including two major metabolites formed by hydroxylation of the butyl side chain and a minor metabolite, an N-2 tetrazole glucuronide. Elimination Losartan Plasma clearance of losartan and its active metabolite is about 600 ml/min and 50 ml/min, respectively. Renal clearance of losartan and its active metabolite is about 74 ml/min and 26 ml/min, respectively. When losartan is administered orally, about 4% of the dose is excreted unchanged in the urine, and about 6% of the dose is excreted in the urine as active metabolite. The pharmacokinetics of losartan and its active metabolite are linear with oral losartan potassium doses up to 200 mg. Following oral administration, plasma concentrations of losartan and its active metabolite decline polyexponentially with a terminal half-life of about 2 hours and 6-9 hours, respectively. During once- daily dosing with 100 mg, neither losartan nor its active metabolite accumulates significantly in plasma. Both biliary and urinary excretion contribute to the elimination of losartan and its metabolites. Following an oral dose of 14C-labelled losartan in man, about 35% of radioactivity is recovered in the urine and 58% in the faeces. Hydrochlorothiazide Hydrochlorothiazide is not metabolized but is eliminated rapidly by the kidney. When plasma levels have been followed for at least 24 hours, the plasma half-life has been observed to vary between 5.6 and 14.8 hours. At least 61 percent of the oral dose is eliminated unchanged within 24 hours. Characteristics in Patients Losartan-Hydrochlorothiazide The plasma concentrations of losartan and its active metabolite and the absorption of hydrochlorothiazide in elderly hypertensives are not significantly different from those in young hypertensives. Losartan Following oral administration in patients with mild to moderate alcoholic cirrhosis of the liver, plasma concentrations of losartan and its active metabolite were, respectively, 5-fold and 1.7-fold greater than those seen in young male volunteers. Pharmacokinetic studies showed that the AUC of losartan in Japanese and non-Japanese healthy male subjects is not different. However, the AUC of the carboxylic acid metabolite (E-3174) appears to be different between the two groups, with an approximately 1.5 fold higher exposure in Japanese subjects than in non-Japanese subjects. The clinical significance of these results is not known. Neither losartan nor the active metabolite can be removed by haemodialysis.

פרטי מסגרת הכללה בסל
התרופה האמורה תינתן לחולים הסובלים מיתר לחץ דם או אי ספיקת לב הסובלים בנוסף מרגישות לטיפול בתכשירים השייכים למשפחת מעכבי ACE או שפיתחו תופעות לוואי לטיפול כאמור
מסגרת הכללה בסל
התוויות הכלולות במסגרת הסל
| התוויה | תאריך הכללה | תחום קליני | Class Effect | מצב מחלה |
|---|---|---|---|---|
| חולה הסובל מיתר לחץ דם או אי ספיקת לב הסובל בנוסף מרגישות לטיפול בתכשירים השייכים למשפחת מעכבי ACE או שפיתח תופעות לוואי לטיפול | ||||
| OLMESARTAN MEDOXOMIL | ||||
| VALSARTAN | ||||
| LOSARTAN | ||||
| IRBESARTAN | ||||
| CANDESARTAN | ||||
| טיפול בחלבון בשתן מתחת ל-1 גרם ומעל ל-30 מ"ג, עבור חולה שלא סובל מיתר לחץ דם או אי ספיקת לב, הסובל בנוסף מרגישות לטיפול בתכשירים השייכים למשפחת מעכבי ACE או שפיתח תופעות לוואי לטיפול כאמור. | ||||
| חולה הסובל מפרוטאינוריה מעל 1 גרם, בשילוב עם מעכבי ACE |
שימוש לפי פנקס קופ''ח כללית 1994
לא צוין
תאריך הכללה מקורי בסל
01/03/2002
הגבלות
תרופה מוגבלת לרישום ע'י רופא מומחה או הגבלה אחרת
מידע נוסף
עלון מידע לצרכן
02.06.19 - עלון לצרכן אנגלית 30.08.22 - עלון לצרכן אנגלית 02.06.19 - עלון לצרכן עברית 30.08.22 - עלון לצרכן עברית 02.06.19 - עלון לצרכן ערבית 15.12.21 - עלון לצרכן ערבית 11.10.22 - עלון לצרכן ערבית 05.12.22 - עלון לצרכן אנגלית 05.12.22 - עלון לצרכן עברית 08.01.23 - עלון לצרכן ערבית 04.05.14 - החמרה לעלון 21.01.20 - החמרה לעלון 18.10.21 - החמרה לעלון 30.08.22 - החמרה לעלון 05.12.22 - החמרה לעלוןלתרופה במאגר משרד הבריאות
אוקסאאר פלוס