Quest for the right Drug
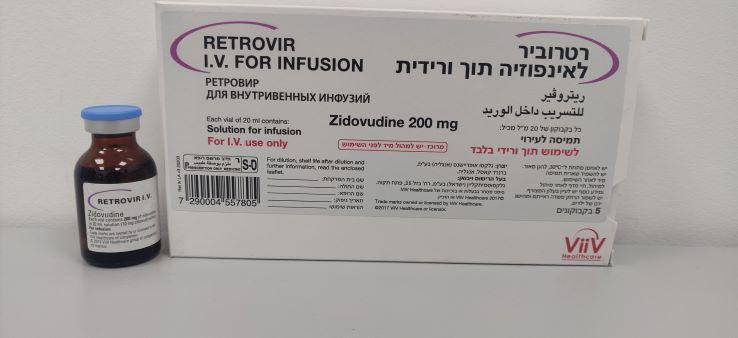
רטרוביר לאינפוזיה תוך ורידית RETROVIR IV FOR INFUSION (ZIDOVUDINE)
תרופה במרשם
תרופה בסל
נרקוטיקה
ציטוטוקסיקה
צורת מתן:
תוך-ורידי : I.V
צורת מינון:
תמיסה לאינפוזיה : SOLUTION FOR INFUSION
עלון לרופא
מינוניםPosology התוויות
Indications תופעות לוואי
Adverse reactions התוויות נגד
Contraindications אינטראקציות
Interactions מינון יתר
Overdose הריון/הנקה
Pregnancy & Lactation אוכלוסיות מיוחדות
Special populations תכונות פרמקולוגיות
Pharmacological properties מידע רוקחי
Pharmaceutical particulars אזהרת שימוש
Special Warning עלון לרופא
Physicians Leaflet
Pharmacological properties : תכונות פרמקולוגיות
Pharmacodynamic Properties
5.1 Pharmacodynamic properties Pharmacotherapeutic group: nucleoside analogue , ATC code: J05A F01 Mode of action: Zidovudine is an antiviral agent which is highly active in vitro against retroviruses including the Human Immunodeficiency Virus (HIV). Zidovudine is phosphorylated in both infected and uninfected cells to the monophosphate (MP) derivative by cellular thymidine kinase. Subsequent phosphorylation of zidovudine-MP to the diphosphate (DP), and then the triphosphate (TP) derivative is catalysed by cellular thymidylate kinase and non-specific kinases respectively. Zidovudine-TP acts as an inhibitor of and substrate for the viral reverse transcriptase. The formation of further proviral DNA is blocked by incorporation of zidovudine-MP into the chain and subsequent chain termination. Competition by zidovudine-TP for HIV reverse transcriptase is approximately 100-fold greater than for cellular DNA polymerase alpha. Clinical virology: The relationships between in vitro susceptibility of HIV to zidovudine and clinical response to therapy remain under investigation. In vitro sensitivity testing has not been standardised and results may therefore vary according to methodological factors. Reduced in vitro sensitivity to zidovudine has been reported for HIV isolates from patients who have received prolonged courses of Retrovir therapy. The available information indicates that for early HIV disease, the frequency and degree of reduction of in vitro sensitivity is notably less than for advanced disease. The reduction of sensitivity with the emergence of zidovudine resistant strains limits the usefulness of zidovudine monotherapy clinically. In clinical studies, clinical end-point data indicate that zidovudine, particularly in combination with lamivudine, and also with didanosine or zalcitabine results in a significant reduction in the risk of disease progression and mortality. The use of a protease inhibitor in a combination of zidovudine and lamivudine, has been shown to confer additional benefit in delaying disease progression, and improving survival compared to the double combination on its own. The anti-viral effectiveness in vitro of combinations of anti-retroviral agents are being investigated. Clinical and in vitro studies of zidovudine in combination with lamivudine indicate that zidovudine-resistant virus isolates can become zidovudine sensitive when they simultaneously acquire resistance to lamivudine. Furthermore there is clinical evidence that zidovudine plus lamivudine delays the emergence of zidovudine resistance in anti-retroviral naive patients. No antagonistic effects in vitro were seen with zidovudine and other antiretrovirals (tested agents: abacavir, didanosine, lamivudine and interferon-alpha). Resistance to thymidine analogues (of which zidovudine is one) is well characterised and is conferred by the stepwise accumulation of up to six specific mutations in the HIV reverse transcriptase at codons 41, 67, 70, 210, 215 and 219. Viruses acquire phenotypic resistance to thymidine analogues through the combination of mutations at codons 41 and 215 or by the accumulation of at least four of the six mutations. These thymidine analogue mutations alone do not cause high-level cross-resistance to any of the other nucleosides, allowing for the subsequent use of any of the other approved reverse transcriptase inhibitors. Two patterns of multi-drug resistance mutations, the first characterised by mutations in the HIV reverse transcriptase at codons 62, 75, 77, 116 and 151 and the second involving a T69S mutation plus a 6-base pair insert at the same position, result in phenotypic resistance to AZT as well as to the other approved nucleoside reverse transcriptase inhibitors. Either of these two patterns of multinucleoside resistance mutations severely limits future therapeutic options. In the US ACTGO76 trial, Retrovir was shown to be effective in reducing the rate of maternal-foetal transmission of HIV-1 (23% infection rate for placebo versus 8% for zidovudine) when administered (100 mg five times a day) to HIV-positive pregnant women (from week 14-34 of pregnancy) and their newborn infants (2 mg/kg every 6 hours) until 6 weeks of age. In the shorter duration 1998 Thailand CDC study, use of oral Retrovir therapy only (300 mg twice daily), from week 36 of pregnancy until delivery, also reduced the rate of maternal-foetal transmission of HIV (19% infection rate for placebo versus 9% for zidovudine). These data, and data from a published study comparing zidovudine regimens to prevent maternal-foetal HIV transmission have shown that short maternal treatments (from week 36 of pregnancy) are less efficacious than longer maternal treatments (from week 14-34 of pregnancy) in the reduction of perinatal HIV transmission.
Pharmacokinetic Properties
5.2 Pharmacokinetic properties Adults: Absorption: Dose-independent kinetics were observed in patients receiving one-hour infusions of 1 to 5 mg/kg 3 to 6 times daily. Mean steady state peak (Cssmax) and trough (Cssmin) plasma concentrations in adults following a one-hour infusion of 2.5 mg/kg every 4 hours were 4.0 and 0.4 µM, respectively (or 1.1 and 0.1 µg/ml). Distribution: The mean terminal plasma half-life was 1.1 hours, the mean total body clearance was 27.1 ml/min/kg and the apparent volume of distribution was 1.6 litres/kg. In adults, the average cerebrospinal fluid/plasma zidovudine concentration ratio 2 to 4 hours after chronic intermittent oral dosing was found to be approximately 0.5. Data indicate that zidovudine crosses the placenta and is found in amniotic fluid and foetal blood. Zidovudine has also been detected in semen and milk. Plasma protein binding is relatively low (34 to 38%) and drug interactions involving binding site displacement are not anticipated. Biotransformation: Zidovudine is primarily eliminated by hepatic conjugation to an inactive glucoronidated metabolite. The 5’-glucuronide of zidovudine is the major metabolite in both plasma and urine, accounting for approximately 50-80% of the administered dose eliminated by renal excretion. 3’-amino-3’-deoxythymidine (AMT) has been identified as a metabolite of zidovudine following intravenous dosing. Elimination: Renal clearance of zidovudine greatly exceeds creatinine clearance, indicating that significant tubular secretion takes place. Paediatrics: Absorption: In children over the age of 5-6 months, the pharmacokinetic profile of zidovudine is similar to that in adults. Cssmax levels were 1.46 µg/ml following an intravenous dose of 80 mg zidovudine/m2 body surface area, 2.26 µg/ml following 120 mg/m2 and 2.96 µg/ml following 160 mg/m2. Distribution: With intravenous dosing, the mean terminal plasma half-life and total body clearance were 1.5 hours and 30.9 ml/min/kg respectively. In children the mean cerebrospinal fluid/plasma zidovudine concentration ratio ranged from 0.52-0.85, as determined during oral therapy 0.5 to 4 hours after dosing and was 0.87 as determined during intravenous therapy 1-5 hours after a 1 hour infusion. During continuous intravenous infusion, the mean steady-state cerebrospinal fluid/plasma concentration ratio was 0.24. Biotransformation: The major metabolite is 5’-glucuronide. After intravenous dosing, 29% of the dose was recovered unchanged in the urine and 45% excreted as the glucuronide. Elimination: Renal clearance of zidovudine greatly exceeds creatinine clearance indicating that significant tubular secretion takes place. The data available on the pharmacokinetics in neonates and young infants indicate that glucuronidation of zidovudine is reduced with a consequent increase in bioavailability, reduction in clearance and longer half-life in infants less than 14 days old but thereafter the pharmacokinetics appear similar to those reported in adults. Pregnancy: The pharmacokinetics of zidovudine has been investigated in a study of eight women during the third trimester of pregnancy. As pregnancy progressed, there was no evidence of drug accumulation. The pharmacokinetics of zidovudine was similar to that of non-pregnant adults. Consistent with passive transmission of the drug across the placenta, zidovudine concentrations in infant plasma at birth were essentially equal to those in maternal plasma at delivery. Elderly: No specific data are available on the pharmacokinetics of zidovudine in the elderly. Renal impairment: Compared to healthy subjects, patients with advanced renal failure have a 50% higher peak plasma concentration after oral administration. Systemic exposure (measured as area under the zidovudine concentration time curve) is increased 100%; the half-life is not significantly altered. In renal failure there is substantial accumulation of the major glucuronide metabolite but this does not appear to cause toxicity. Haemodialysis and peritoneal dialysis have no significant effect on zidovudine elimination whereas elimination of the inactive glucuronide metabolite is increased. (see section 4.2). Hepatic impairment: There are limited data concerning the pharmacokinetics of zidovudine in patients with hepatic impairment (see section 4.2). No specific data are available on the pharmacokinetics of zidovudine in the elderly.

שימוש לפי פנקס קופ''ח כללית 1994
לא צוין
תאריך הכללה מקורי בסל
01/01/1995
הגבלות
תרופה מוגבלת לרישום ע'י רופא מומחה או הגבלה אחרת
מידע נוסף
עלון מידע לצרכן
23.12.15 - עלון לצרכן 22.08.17 - עלון לצרכן 17.01.19 - עלון לצרכן 10.03.19 - עלון לצרכן 02.11.22 - עלון לצרכן עברית 09.01.23 - עלון לצרכן אנגלית 09.01.23 - עלון לצרכן ערבית 01.03.23 - עלון לצרכן אנגלית 01.03.23 - עלון לצרכן עברית 01.03.23 - עלון לצרכן ערבית 13.10.21 - החמרה לעלון 14.09.22 - החמרה לעלוןלתרופה במאגר משרד הבריאות
רטרוביר לאינפוזיה תוך ורידית