Quest for the right Drug
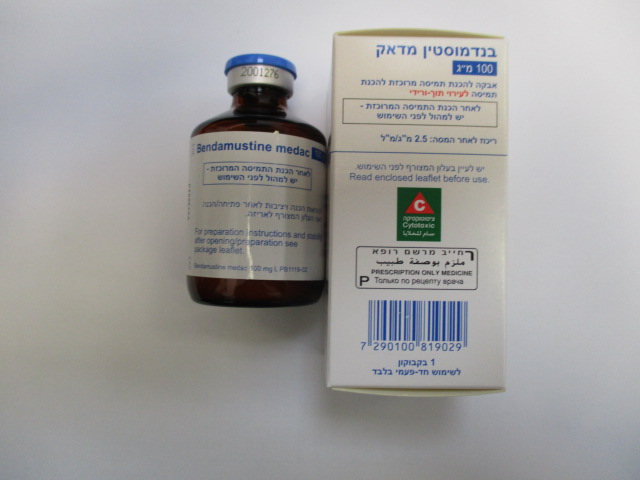
בנדמוסטין מדאק 100 מ"ג BENDAMUSTINE MEDAC 100 MG (BENDAMUSTINE HYDROCHLORIDE)
תרופה במרשם
תרופה בסל
נרקוטיקה
ציטוטוקסיקה
צורת מתן:
תוך-ורידי : I.V
צורת מינון:
אבקה להכנת תמיסה מרוכזת לעירוי : POWDER FOR CONCENTRATE FOR SOLUTION FOR INFUSION
עלון לרופא
מינוניםPosology התוויות
Indications תופעות לוואי
Adverse reactions התוויות נגד
Contraindications אינטראקציות
Interactions מינון יתר
Overdose הריון/הנקה
Pregnancy & Lactation אוכלוסיות מיוחדות
Special populations תכונות פרמקולוגיות
Pharmacological properties מידע רוקחי
Pharmaceutical particulars אזהרת שימוש
Special Warning עלון לרופא
Physicians Leaflet
Posology : מינונים
4.2 Posology and method of administration Posology Monotherapy for chronic lymphocytic leukaemia 100 mg/m² body surface area bendamustine hydrochloride on days 1 and 2; every 4 weeks up to 6 times. Monotherapy for indolent non-Hodgkin's lymphomas refractory to rituximab 120 mg/m² body surface area bendamustine hydrochloride on days 1 and 2; every 3 weeks for at least 6 times. Follicular non-Hodgkin’s lymphoma: Combination with rituximab The dose is 90 mg/m² body surface area bendamustine hydrochloride on days 1 and 2 plus 375 mg/m² rituximab on day 1; repetition every 4 weeks. Hepatic impairment On the basis of pharmacokinetic data, no dose adjustment is necessary in patients with mild hepatic impairment (serum bilirubin < 1.2 mg/dl). A 30% dose reduction is recommended in patients with moderate hepatic impairment (serum bilirubin 1.2 - 3.0 mg/dl). No data is available in patients with severe hepatic impairment (serum bilirubin values of > 3.0 mg/dl) (see section 4.3). Renal impairment On the basis of pharmacokinetic data, no dose adjustment is necessary in patients with a creatinine clearance of > 10 ml/min. Experience in patients with severe renal impairment is limited. Paediatric population The safety and efficacy of bendamustine hydrochloride in children have not yet been established. Current available data is not sufficient to make a recommendation on posology. Elderly patients There is no evidence that dose adjustments are necessary in elderly patients (see also section 5.2). Method of administration For intravenous infusion over 30 - 60 minutes (see section 6.6). Infusion must be administered under the supervision of a physician qualified and experienced in the use of chemotherapeutic agents. Poor bone marrow function is related to increased chemotherapy-induced haematological toxicity. Treatment should not be started if leukocyte and/or platelet values dropped to < 3,000/µl or < 75,000/µl, respectively (see section 4.3). Treatment should be terminated or delayed if leukocyte and/or platelet values dropped to < 3,000/μl or < 75,000/μl, respectively. Treatment can be continued after leukocyte values have increased to > 4,000/μl and platelet values to > 100,000/μl. The leukocyte and platelet Nadir is reached after 14-20 days with regeneration after 3-5 weeks. During therapy free intervals strict monitoring of the blood count is recommended (see section 4.4). In case of non-haematological toxicity dose reductions have to be based on the worst CTC grades in the preceding cycle. A 50% dose reduction is recommended in case of CTC grade 3 toxicity. An interruption of treatment is recommended in case of CTC grade 4 toxicity. If a patient requires a dose modification the individually calculated reduced dose must be given on day 1 and 2 of the respective treatment cycle. For instructions on reconstitution of the medicinal product before administration, see section 6.6.

שימוש לפי פנקס קופ''ח כללית 1994
לא צוין
תאריך הכללה מקורי בסל
לא צוין
הגבלות
לא צוין
מידע נוסף
