Quest for the right Drug
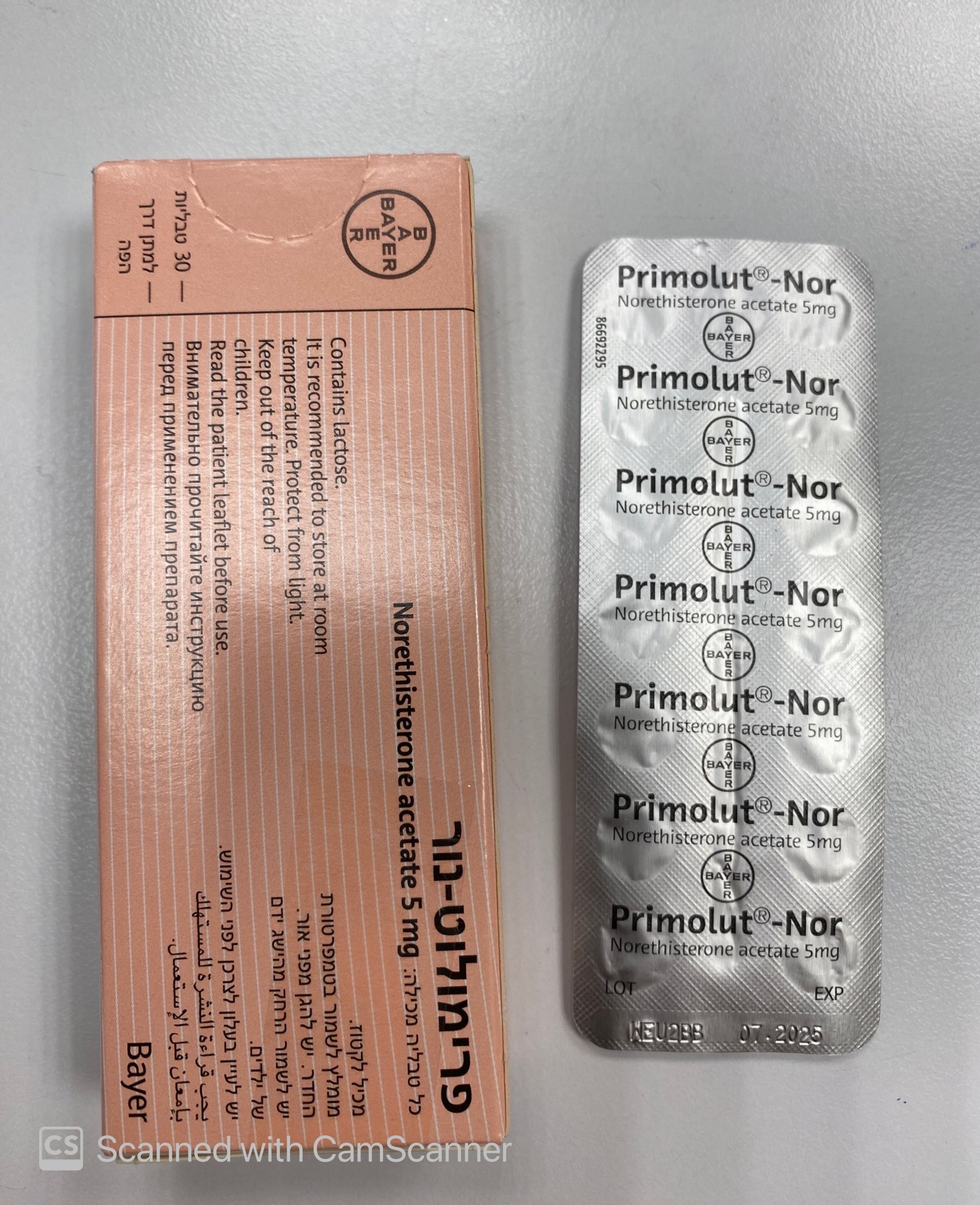
פרימולוט-נור PRIMOLUT-NOR (NORETHISTERONE ACETATE)
תרופה במרשם
תרופה בסל
נרקוטיקה
ציטוטוקסיקה
צורת מתן:
פומי : PER OS
צורת מינון:
טבליה : TABLETS
עלון לרופא
מינוניםPosology התוויות
Indications תופעות לוואי
Adverse reactions התוויות נגד
Contraindications אינטראקציות
Interactions מינון יתר
Overdose הריון/הנקה
Pregnancy & Lactation אוכלוסיות מיוחדות
Special populations תכונות פרמקולוגיות
Pharmacological properties מידע רוקחי
Pharmaceutical particulars אזהרת שימוש
Special Warning עלון לרופא
Physicians Leaflet
Special Warning : אזהרת שימוש
4.4 Special warnings and precautions for use Medical Examination A complete personal and family medical history should be taken for each woman. Physical examination should be guided by this and by the contraindications (section 4.3) and warnings (section 4.4) for this product. The frequency and nature of these assessments should be based upon relevant guidelines which should be adapted to the individual woman and should include measurement of blood pressure, and if judged appropriate by the clinician, breast, abdominal and pelvic examination including cervical cytology. Therapy should be discontinued immediately if the following occur: New onset of migraine-type headaches or more frequent occurrence of unusually severe headaches Sudden perceptual disorders (e.g. disturbances of vision or hearing) First signs of thrombophlebitis or thromboembolic symptoms, feeling of pain and tightness in the chest Pending operations (six weeks beforehand), immobilisation (e.g. after accidents) Onset of jaundice or deterioration in liver function, anicteric hepatitis, general pruritus Significant increase in blood pressure Pregnancy. If any of the conditions/risk factors mentioned below is present or deteriorates while using Primolut-Nor, an individual risk-benefit analysis should be done before Primolut-Nor is started or continued. • Circulatory disorders It has been concluded from epidemiological surveys that the use of oral oestrogen/progestogen containing ovulation inhibitors is associated by an increased incidence of thromboembolic diseases. Therefore, one should keep the possibility of an increased thromboembolic risk in mind, particularly where there is a history of thromboembolic diseases. A patient who develops symptoms suggestive of thromboembolic complications should stop treatment immediately. The need for treatment should be reassessed before continuing therapy. Generally recognised risk factors for venous thromboembolism (VTE) include: 1. Positive personal or family history (VTE in a sibling or a parent at a relatively early age) 2. Age 3. Obesity 4. Systemic lupus erythematous (SLE) 5. Prolonged immobilisation 6. Major surgery 7. Major trauma. Patients with a history of VTE or known thrombophilic states have an increased risk of VTE. The treatment with steroid hormone may add to this risk. Personal or strong family history of thromboembolism or recurrent spontaneous abortion should be investigated in order to exclude a thromboembolic predisposition. Until a thorough evaluation of thrombophilic factors has been made or anticoagulant treatment initiated, use of progestogens in these patients should be viewed as contraindicated. Where a patient is already taking anticoagulants, the risk and benefits of progestogen therapy should be carefully considered. The risk of VTE may be temporarily increased with prolonged immobilisation, major trauma or major surgery. As in all post-operative patients, scrupulous attention should be given to prophylactic measures to prevent VTE. Where prolonged immobilisation is likely to follow elective surgery, particularly abdominal or orthopaedic surgery to the lower limbs, consideration should be given to stopping progestogen therapy 4-6 weeks pre-operatively. Treatment should not be restarted until the patient is fully remobilised. There is no consensus about the possible role of varicose veins and superficial thrombophlebitis in venous thromboembolism. • Known Hyperlipidaemias Women with hypertriglyceridemia, or a family history thereof, may be at increased risk of pancreatitis when using COCs. Women with hyperlipiaedmia are at increased risk of arterial disease (see section 4.4 “Circulatory disorders”). However, routine screening of women on COCs is not appropriate. • Tumours In rare cases, benign liver tumours, and even more rarely, malignant liver tumours have been reported in users of hormonal substances such as the one contained in Primolut-Nor. In isolated cases, these tumours have led to life-threatening intra-abdominal haemorrhages. If severe upper abdominal complaints, liver enlargement or signs of intra-abdominal haemorrhage occur, a liver tumour should be included in the differential diagnosis and, if necessary, the preparation should be withdrawn. • Other Primolut-No r can influence carbohydrate metabolism. Parameters of carbohydrate metabolism should be examined carefully in all diabetics before and regularly during treatment. Chloasma may occasionally occur, especially in women with a history of chloasma gravidarum. Women with a tendency to chloasma should minimise exposure to the sun or ultraviolet radiation when taking Primolut-Nor. Patients who have a history of depression should be carefully observed and the drug discontinued if the depression recurs to a serious degree. Patients with rare hereditary problems of galactose intolerance, the Lapp lactase deficiency or glucose-galactose malabsorption should not take this medicine. Any patient who develops an acute impairment of vision, proptosis, diplopia or migraine headache should be carefully evaluated ophthalmologically to exclude papilloedema or retinal lesions before continuing medication. Progestogens may cause fluid retention. Special care should be taken when prescribing norethisterone in patients with conditions which might be aggravated by this factor: • Epilepsy • Migraine • Asthma • Cardiac dysfunction • Renal dysfunction. If menstrual bleeding should fail to follow a course of Primolut-Nor, or if the patient wishes to postpone menstruation in special circumstances, the possibility of pregnancy must be excluded before a further course is given. Additional warnings based on the partial metabolisation of norethisterone to ethinylestradiol After oral administration, norethisterone is partly metabolised to ethinylestradiol resulting in an equivalent dose of about 4-6 micrograms ethinylestradiol per 1 milligram of orally administered norethisterone or norethisterone acetate (see section 5.2) Due to the partial conversion of norethisterone to ethinylestradiol, administration of Primolut- Nor is expected to result in similar pharmacological effects as seen with COCs. Therefore, the following general warnings associated with the use of COCs should also be considered: • Circulatory disorders (thromboembolic events) Venous thromboembolic events (VTE) Epidemiological studies have shown that the incidence of venous thromboembolism (VTE) in users of oral contraceptives with low oestrogen content (<50 µg ethinylestradiol) ranges from about 20 to 40 cases per 100,000 women-years, but this risk estimate varies according to the progestogen. This compares with 5 to 10 cases per 100,000 women-years for non- users. The use of any combined oral contraceptive carries an increased risk of VTE compared with no use. This increased risk is less than the risk of VTE associated with pregnancy, which is estimated as 60 cases per 100,000 pregnancies. The excess risk of VTE is highest during the first year a woman initially starts using a COC or when she restarts COC use after a pill-free interval of at least a month. VTE may be life-threatening or may have a fatal outcome (in 1-2 % of the cases). VTE manifesting as deep venous thrombosis and/or pulmonary embolism, may occur during the use of all COCs. Extremely rarely, thrombosis has been reported to occur in other blood vessels, e.g. hepatic, mesenteric, renal, cerebral or retinal veins and arteries, in COC users. Common signs/symptoms of VTE include: • Severe pain in the calf of one leg; swelling of the lower leg • Sudden breathlessness, chest pain. Arterial thromboembolic related conditions The use of a combined oral contraceptive may also increase the risk of conditions such as stroke and myocardial infarction which are secondary to arterial thromboembolic events. Common signs/symptoms associated with arterial thromboembolism include: • sudden severe pain in the chest, whether or not reaching to the left arm; • sudden coughing for no apparent reason • any unusual severe, prolonged headache, especially if it occurs for the first time or gets progressively worse, or is associated with any of the following symptoms: o sudden partial or complete loss of vision or diplopia; o aphasia; o vertigo; o collapse with or without focal epilepsy; o weakness or very marked numbness suddenly affecting one side or one part of the body. Risk Factors for Thromboembolic Events: • Age • Obesity (body mass index over 30 kg/m2) • A positive family history (i.e. venous or arterial thromboembolism ever in a sibling or parent at a relatively early age). If a hereditary predisposition is known or suspected, the woman should be referred to a specialist for advice before deciding about any COC use • Prolonged immobilisation, major surgery, any surgery to the legs, or major trauma. In these situations it is advisable to discontinue COC use (in the case of elective surgery at least four weeks in advance) and not to resume until two weeks after complete remobilisation • Smoking (with heavier smoking and increasing age the risk further increases, especially in women over 35 years of age) • Dyslipoproteinaemia • Hypertension • Migraine (An increase in frequency or severity of migraine during COC use may be prodromal of a cerebrovascular event and therefore a reason for immediate discontinuation of the COC). • Valvular heart disease • Atrial fibrillation Other factors affecting circulatory events Other medical conditions which have been associated with adverse circulatory events include: • Diabetes mellitus • Systemic lupus erythematosus (SLE) • Haemolytic uremic syndrome • Chronic inflammatory bowel disease (Crohn’s disease/Ulcerative colitis) • Sickle cell disease. Biochemical factors that may be indicative of hereditary or acquired predisposition for venous or arterial thrombosis include: • Activated Protein C (APC) resistance • Hyperhomocysteinaemia • Antithrombin-III deficiency • Protein C deficiency • Protein S deficiency • Antiphospholipid antibodies (anticardiolipin antibodies, lupus anticoagulant). When considering risk/benefit, the physician should take into account that adequate treatment of a condition may reduce the associated risk of thrombosis and that the risk associated with pregnancy is higher than that associated with COC use (<0.05 mg ethinylestradiol). • Tumours Cervical Cancer The most important risk factor for cervical cancer is persistent HPV infection. Some epidemiological studies have indicated that long-term use of COCs may further contribute to this increased risk but there continues to be controversy about the extent to which this finding is attributable to confounding effects, e.g., cervical screening and sexual behaviour including use of barrier contraceptives. Breast Cancer A meta-analysis from 54 epidemiological studies reported that there is a slightly increased relative risk (RR = 1.24) of having breast cancer diagnosed in women who are currently using COCs. The excess risk gradually disappears during the course of the 10 years after cessation of COC use. Because breast cancer is rare in women under 40 years of age, the excess number of breast cancer diagnoses in current and recent COC users is small in relation to the overall risk of breast cancer. These studies do not provide evidence for causation. The observed pattern of increased risk may be due to an earlier diagnosis of breast cancer in COC users, the biological effects of COCs or a combination of both. The breast cancers diagnosed in ever-users tend to be less advanced clinically than the cancers diagnosed in never-users. Malignancies may be life-threatening or may have a fatal outcome. • Other Blood pressure Although small increases in blood pressure have been reported in many women taking COCs, clinically relevant increases are rare. However, if a sustained clinically significant hypertension develops during the use of a COC then it is prudent for the physician to withdraw the COC and treat the hypertension. Where considered appropriate, COC use may be resumed if normotensive values can be achieved with antihypertensive therapy. Conditions which deteriorate in pregnancy or during previous COC use The following conditions have been reported to occur or deteriorate with both pregnancy and COC use, but the evidence of an association with COC use is inconclusive: • jaundice and/or pruritus related to cholestasis • gallstone formation • porphyria • systemic lupus erythematosus (SLE) • haemolytic uremic syndrome • Sydenham’s chorea • herpes gestationis • otosclerosis-related hearing loss. In women with hereditary angioedema exogenous estrogens may induce or exacerbate symptoms of angioedema. Acute or chronic disturbances of liver function may necessitate the discontinuation of COC use until markers of liver function return to normal. Recurrence of cholestatic jaundice which occurred first during pregnancy or previous use of sex steroids necessitates the discontinuation of COCs. Crohn’s disease and ulcerative colitis have been associated with COC use. ALT elevations During clinical trials with patients treated for hepatitis C virus infections (HCV) with the medicinal products containing ombitasvir/paritaprevir/ritonavir and dasabuvir with or without ribavirin, transaminase (ALT) elevations higher than 5 times the upper limit of normal (ULN) occurred significantly more frequent in women using ethinylestradiol-containing medications such as combined hormonal contraceptives (CHCs). As norethisterone is partly metabolized into ethinylestradiol, this warning applies to women using norethisterone (see sections 4.3 and 4.5).
Effects on Driving
4.7 Effects on ability to drive and use machines None known.

שימוש לפי פנקס קופ''ח כללית 1994
Amenorrhea, dysfunctional uterine bleeding, endometriosis
תאריך הכללה מקורי בסל
01/01/1995
הגבלות
תרופה שאושרה לשימוש כללי בקופ'ח
מידע נוסף
