Quest for the right Drug
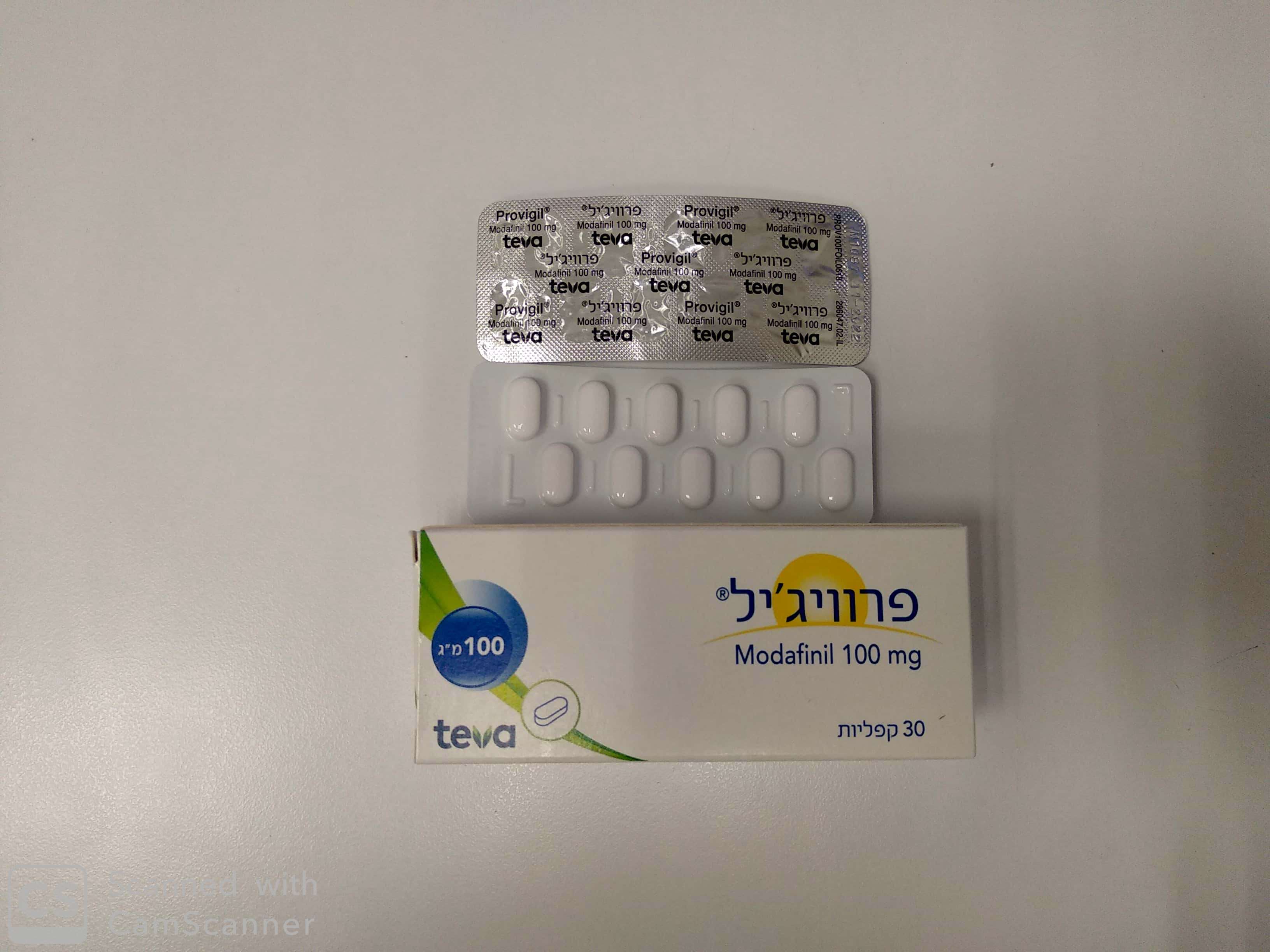
פרוויג'יל PROVIGIL (MODAFINIL)
תרופה במרשם
תרופה בסל
נרקוטיקה
ציטוטוקסיקה
צורת מתן:
פומי : PER OS
צורת מינון:
קפליות : CAPLETS
עלון לרופא
מינוניםPosology התוויות
Indications תופעות לוואי
Adverse reactions התוויות נגד
Contraindications אינטראקציות
Interactions מינון יתר
Overdose הריון/הנקה
Pregnancy & Lactation אוכלוסיות מיוחדות
Special populations תכונות פרמקולוגיות
Pharmacological properties מידע רוקחי
Pharmaceutical particulars אזהרת שימוש
Special Warning עלון לרופא
Physicians Leaflet
Special Warning : אזהרת שימוש
5 WARNINGS AND PRECAUTIONS 5.1 Serious Rash, including Stevens-Johnson Syndrome Serious rash requiring hospitalization and discontinuation of treatment has been reported in association with the use of modafinil. In clinical trials of modafinil, the incidence of rash resulting in discontinuation was approximately 0.8% (13 per 1,585) in pediatric patients (age <17 years); these rashes included 1 case of possible Stevens-Johnson Syndrome (SJS) and 1 case of apparent multi-organ hypersensitivity reaction. Several of the cases were associated with fever and other abnormalities (e.g., vomiting, leukopenia). The median time to rash that resulted in discontinuation was 13 days. No such cases were observed among 380 pediatric patients who received placebo. PROVIGIL is not approved for use in pediatric patients for any indication [see Use in Specific Populations (8.4)]. Rare cases of serious or life-threatening rash, including SJS, Toxic Epidermal Necrolysis (TEN), and Drug Rash with Eosinophilia and Systemic Symptoms (DRESS) have been reported in adults and children in worldwide postmarketing experience. The reporting rate of TEN and SJS associated with modafinil use, which is generally accepted to be an underestimate due to underreporting, exceeds the background incidence rate. Estimates of the background incidence rate for these serious skin reactions in the general population range between 1 to 2 cases per million-person years. There are no factors that are known to predict the risk of occurrence or the severity of rash associated with PROVIGIL. Nearly all cases of serious rash associated with modafinil occurred within 1 to 5 weeks after treatment initiation. However, isolated cases have been reported after prolonged treatment (e.g., 3 months). Accordingly, duration of therapy cannot be relied upon as a means to predict the potential risk heralded by the first appearance of a rash. Although benign rashes also occur with PROVIGIL, it is not possible to reliably predict which rashes will prove to be serious. Accordingly, PROVIGIL should be discontinued at the first sign of rash, unless the rash is clearly not drug-related. Discontinuation of treatment may not prevent a rash from becoming life-threatening or permanently disabling or disfiguring. 5.2 Angioedema and Anaphylaxis Reactions Angioedema and hypersensitivity (with rash, dysphagia, and bronchospasm), were observed in patients treated with armodafinil, the R enantiomer of modafinil (which is the racemic mixture). No such cases were observed in modafinil clinical trials. However, angioedema has been reported in postmarketing experience with modafinil. Patients should be advised to discontinue therapy and immediately report to their physician any signs or symptoms suggesting angioedema or anaphylaxis (e.g., swelling of face, eyes, lips, tongue or larynx; difficulty in swallowing or breathing; hoarseness). 5.3 Multi-organ Hypersensitivity Reactions Multi-organ hypersensitivity reactions, including at least one fatality in postmarketing experience, have occurred in close temporal association (median time to detection 13 days: range 4-33) to the initiation of modafinil. Although there have been a limited number of reports, multi-organ hypersensitivity reactions may result in hospitalization or be life-threatening. There are no factors that are known to predict the risk of occurrence or the severity of multi-organ hypersensitivity reactions. Signs and symptoms of this disorder were diverse; however, patients typically, although not exclusively, presented with fever and rash associated with other organ system involvement. Other associated manifestations included myocarditis, hepatitis, liver function test abnormalities, hematological abnormalities (e.g., eosinophilia, leukopenia, thrombocytopenia), pruritus, and asthenia. Because multi-organ hypersensitivity is variable in its expression, other organ system symptoms and signs, not noted here, may occur. If a multi-organ hypersensitivity reaction is suspected, PROVIGIL should be discontinued. Although there are no case reports to indicate cross-sensitivity with other drugs that produce this syndrome, the experience with drugs associated with multi-organ hypersensitivity would indicate this to be a possibility. 5.4 Persistent Sleepiness Patients with abnormal levels of sleepiness who take PROVIGIL should be advised that their level of wakefulness may not return to normal. Patients with excessive sleepiness, including those taking PROVIGIL, should be frequently reassessed for their degree of sleepiness and, if appropriate, advised to avoid driving or any other potentially dangerous activity. Prescribers should also be aware that patients may not acknowledge sleepiness or drowsiness until directly questioned about drowsiness or sleepiness during specific activities. 5.5 Psychiatric Symptoms Psychiatric adverse reactions have been reported in patients treated with modafinil. In the adult PROVIGIL controlled trials, psychiatric symptoms resulting in treatment discontinuation (at a frequency >0.3%) and reported more often in patients treated with PROVIGIL compared to those treated with placebo were anxiety (1%), nervousness (1%), insomnia (<1%), confusion (<1%), agitation (<1%), and depression (<1%). Postmarketing adverse reactions associated with the use of modafinil have included mania, delusions, hallucinations, suicidal ideation, and aggression, some resulting in hospitalization. Many, but not all, patients had a prior psychiatric history. One healthy male volunteer developed ideas of reference, paranoid delusions, and auditory hallucinations in association with multiple daily 600 mg doses of PROVIGIL (three times the recommended dose) and sleep deprivation. There was no evidence of psychosis 36 hours after drug discontinuation. Caution should be exercised when PROVIGIL is given to patients with a history of psychosis, depression, or mania. Consideration should be given to the possible emergence or exacerbation of psychiatric symptoms in patients treated with PROVIGIL. If psychiatric symptoms develop in association with PROVIGIL administration, consider discontinuing PROVIGIL. 5.6 Effects on Ability to Drive and Use Machinery Although PROVIGIL has not been shown to produce functional impairment, any drug affecting the CNS may alter judgment, thinking or motor skills. Patients should be cautioned about operating an automobile or other hazardous machinery until it is reasonably certain that PROVIGIL therapy will not adversely affect their ability to engage in such activities. 5.7 Cardiovascular Events In modafinil clinical studies, cardiovascular adverse reactions, including chest pain, palpitations, dyspnea, and transient ischemic T-wave changes on ECG occurred in three subjects in association with mitral valve prolapse or left ventricular hypertrophy. In a Canadian clinical trial, a 35 year old obese narcoleptic male with a prior history of syncopal episodes experienced a 9-second episode of asystole after 27 days of modafinil treatment (300 mg/day in divided doses). PROVIGIL is not recommended in patients with a history of left ventricular hypertrophy or in patients with mitral valve prolapse who have experienced the mitral valve prolapse syndrome when previously receiving CNS stimulants. Findings suggestive of mitral valve prolapse syndrome include but are not limited to ischemic ECG changes, chest pain, or arrhythmia. If new onset of any of these findings occurs, consider cardiac evaluation. Consider increased monitoring in patients with a recent history of myocardial infarction or unstable angina. Blood pressure monitoring in short term (< 3 months) controlled trials showed no clinically significant changes in mean systolic and diastolic blood pressure in patients receiving PROVIGIL as compared to placebo. However, a retrospective analysis of the use of antihypertensive medication in these studies showed that a greater proportion of patients on PROVIGIL required new or increased use of antihypertensive medications (2.4%) compared to patients on placebo (0.7%). The differential use was slightly larger when only studies in OSA were included, with 3.4% of patients on PROVIGIL and 1.1% of patients on placebo requiring such alterations in the use of antihypertensive medication. Increased monitoring of heart rate and blood pressure may be appropriate in patients on PROVIGIL. Caution should be exercised when prescribing PROVIGIL to patients with known cardiovascular disease. 5.8 Excipients with known effects Patients with rare hereditary problems of galactose intolerance, total lactase deficiency or glucose-galactose malabsorption should not take this medicine. This medicine contains less than 1 mmol sodium (23 mg) per tablet, that is to say essentially ‘sodium-free’. 6 ADVERSE REACTIONS The following serious adverse reactions are described elsewhere in the labeling: • Serious Rash, including Stevens-Johnson Syndrome [see Warnings and Precautions (5.1)] • Angioedema and Anaphylaxis Reactions [see Warnings and Precautions (5.2)] • Multi-organ Hypersensitivity Reactions [see Warnings and Precautions (5.3)] • Persistent Sleepiness [see Warnings and Precautions (5.4)] • Psychiatric Symptoms [see Warnings and Precautions (5.5)] • Effects on Ability to Drive and Use Machinery [see Warnings and Precautions (5.6)] • Cardiovascular Events [see Warnings and Precautions (5.7)] 6.1 Clinical Trials Experience Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a drug cannot be directly compared to rates in the clinical trials of another drug and may not reflect the rates observed in practice. PROVIGIL has been evaluated for safety in over 3,500 patients, of whom more than 2,000 patients with excessive sleepiness associated with OSA, SWD, and narcolepsy. Most Common Adverse Reactions In placebo-controlled clinical trials, the most common adverse reactions (≥ 5%) associated with the use of PROVIGIL more frequently than placebo-treated patients were headache, nausea, nervousness, rhinitis, diarrhea, back pain, anxiety, insomnia, dizziness, and dyspepsia. The adverse reaction profile was similar across these studies. Table 1 presents the adverse reactions that occurred at a rate of 1% or more and were more frequent in PROVIGIL-treated patients than in placebo-treated patients in the placebo-controlled clinical trials. Table 1. Adverse Reactions in Pooled Placebo-Controlled Trials* in Narcolepsy, OSA, and SWD PROVIGIL Placebo (%) (%) (n = 934) (n=567) Headache 34 23 Nausea 11 3 Nervousness 7 3 Rhinitis 7 6 Back Pain 6 5 Diarrhea 6 5 Anxiety 5 1 Dizziness 5 4 Dyspepsia 5 4 Insomnia 5 1 Anorexia 4 1 Dry Mouth 4 2 Pharyngitis 4 2 Chest Pain 3 1 Hypertension 3 1 Abnormal Liver Function 2 1 Constipation 2 1 Depression 2 1 Palpitation 2 1 Paresthesia 2 0 Somnolence 2 1 Tachycardia 2 1 Vasodilatation 2 0 Abnormal Vision 1 0 Agitation 1 0 Asthma 1 0 Chills 1 0 Confusion 1 0 Dyskinesia 1 0 Edema 1 0 Emotional Lability 1 0 Eosinophilia 1 0 Epistaxis 1 0 Flatulence 1 0 Hyperkinesia 1 0 Hypertonia 1 0 Mouth Ulceration 1 0 Sweating 1 0 Taste Perversion 1 0 Thirst 1 0 Tremor 1 0 Urine Abnormality 1 0 Vertigo 1 0 * Adverse Reactions that occurred in ≥ 1% of PROVIGIL-treated patients (either 200, 300, or 400 mg once daily) and greater incidence than placebo Dose-Dependent Adverse Reactions In the placebo-controlled clinical trials which compared doses of 200, 300, and 400 mg/day of PROVIGIL and placebo, the following adverse reactions were dose related: headache and anxiety. Adverse Reactions Resulting in Discontinuation of Treatment In placebo-controlled clinical trials, 74 of the 934 patients (8%) who received PROVIGIL discontinued due to an adverse reaction compared to 3% of patients that received placebo. The most frequent reasons for discontinuation that occurred at a higher rate for PROVIGIL than placebo patients were headache (2%), nausea, anxiety, dizziness, insomnia, chest pain, and nervousness (each <1%). Laboratory Abnormalities Clinical chemistry, hematology, and urinalysis parameters were monitored in the studies. Mean plasma levels of gamma glutamyltransferase (GGT) and alkaline phosphatase (AP) were found to be higher following administration of PROVIGIL, but not placebo. Few patients, however, had GGT or AP elevations outside of the normal range. Shifts to higher, but not clinically significantly abnormal, GGT and AP values appeared to increase with time in the population treated with PROVIGIL in the placebo-controlled clinical trials. No differences were apparent in alanine aminotransferase (ALT), aspartate aminotransferase (AST), total protein, albumin, or total bilirubin. 6.2 Postmarketing Experience The following adverse reactions have been identified during post approval use of PROVIGIL. Because these reactions are reported voluntarily from a population of uncertain size, it is not always possible to reliably estimate their frequency or establish a causal relationship to drug exposure. Cardiovascular: Stroke Hematologic: agranulocytosis Psychiatric disorders: psychomotor hyperactivity Reporting of suspected adverse reactions Reporting suspected adverse reactions after authorisation of the medicinal product is important. It allows continued monitoring of the benefit/risk balance of the medicinal product. Any suspected adverse events should be reported to the Ministry of Health according to the National Regulation by using an online form https://sideeffects.health.gov.il/
Effects on Driving

פרטי מסגרת הכללה בסל
התרופה תינתן לטיפול במקרים האלה: 1.שיפור עירנות בחולי נרקולפסיה. התחלת הטיפול בתרופה ייעשה לפי מרשם של רופא מומחה ממעבדת שינה. 2. נטייה מוגברת לשינה בחולי טרשת נפוצה פעילה עם ניקוד שווה או גבוה מ-40 לפי סקלת FIS (Fatigue impact scale). התחלת הטיפול בתרופה ייעשה לפי מרשם של רופא מומחה בנוירולוגיה ממרפאת טרשת נפוצה.
מסגרת הכללה בסל
התוויות הכלולות במסגרת הסל
| התוויה | תאריך הכללה | תחום קליני | Class Effect | מצב מחלה |
|---|---|---|---|---|
| לשיפור העירנות | MODAFINIL, ARMODAFINIL | |||
| נטייה מוגברת לשינה בחולי טרשת נפוצה פעילה, עם ניקוד שווה או גבוה מ-40 לפי סקלת FIS (Fatigue impact scale) | ||||
| שיפור עירנות בחולי נרקולפסיה. |
שימוש לפי פנקס קופ''ח כללית 1994
לא צוין
תאריך הכללה מקורי בסל
01/01/2009
הגבלות
תרופה מוגבלת לרישום ע'י רופא מומחה או הגבלה אחרת
מידע נוסף
