Quest for the right Drug
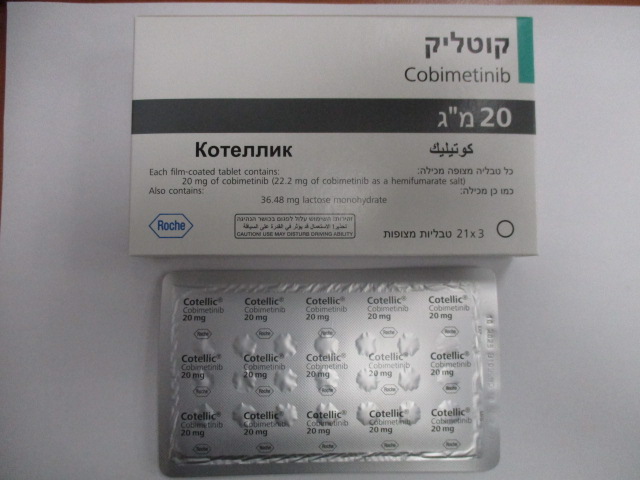
קוטליק COTELLIC (COBIMETINIB AS HEMIFUMARATE)
תרופה במרשם
תרופה בסל
נרקוטיקה
ציטוטוקסיקה
צורת מתן:
פומי : PER OS
צורת מינון:
טבליות מצופות פילם : FILM COATED TABLETS
עלון לרופא
מינוניםPosology התוויות
Indications תופעות לוואי
Adverse reactions התוויות נגד
Contraindications אינטראקציות
Interactions מינון יתר
Overdose הריון/הנקה
Pregnancy & Lactation אוכלוסיות מיוחדות
Special populations תכונות פרמקולוגיות
Pharmacological properties מידע רוקחי
Pharmaceutical particulars אזהרת שימוש
Special Warning עלון לרופא
Physicians Leaflet
Adverse reactions : תופעות לוואי
4.8 Undesirable effects Unresectable or Metastatic Melanoma Summary of the safety profile The safety of Cotellic in combination with vemurafenib has been evaluated in 247 patients with advanced BRAF V600 mutated melanoma in Study GO28141.The median time to onset for the first Grade ≥3 adverse events was 0.6 months in the Cotellic plus vemurafenib arm vs 0.8 months in the placebo plus vemurafenib arm. The safety of Cotellic in combination with vemurafenib has also been evaluated in 129 patients with advanced BRAF V600 mutated melanoma in Study NO25395. The safety profile of Study NO25395 was consistent with that observed in Study GO28141. In Study GO28141, the most common adverse reactions (>20%) observed with a higher frequency in the Cotellic plus vemurafenib arm were diarrhoea, rash, nausea, pyrexia, photosensitivity reaction, increased alanine aminotransferase, increased aspartate aminotransferase, increased blood creatine phosphokinase, and vomiting. The most common adverse reactions (>20%) observed with a higher frequency in the placebo plus vemurafenib arm were arthralgia, alopecia, and hyperkeratosis. Fatigue was observed at similar frequencies in both arms. Please refer to the vemurafenib Prescribing Information for complete descriptions of all undesirable effects associated with vemurafenib treatment. Tabulated list of adverse reactions Adverse drug reactions (ADRs) are based on results from a multi-centre, randomised, double-blind, placebo-controlled, Phase III Study (GO28141) that evaluated the safety and efficacy of Cotellic in combination with vemurafenib as compared to vemurafenib alone in previously untreated BRAF V600 mutation-positive patients with unresectable locally advanced (Stage IIIc) or metastatic melanoma (Stage IV). ADR frequencies are based upon the safety analysis of patients treated with cobimetinib plus vemurafenib with a median follow up of 11.2 months (data cut-off date of 19 September 2014). ADRs which were reported in melanoma patients are listed below by MedDRA body system organ class, frequency and grade of severity. The following convention has been used for the classification of frequency: Very common ≥ 1/10 Common ≥ 1/100 to < 1/10 Uncommon ≥ 1/1,000 to < 1/100 Rare ≥ 1/10,000 to < 1/1,000 Very rare < 1/10,000 Table 3 lists adverse reactions considered associated with the use of Cotellic. Within each frequency grouping, ADRs are presented in order of decreasing severity and were reported according to NCI- CTCAE v 4.0 (common toxicity criteria) for assessment of toxicity in Study GO28141. Table 3 Adverse drug reactions (ADRs) in patients treated with Cotellic in combination with vemurafenib in Study GO28141^ System organ class Very Common Common Uncommon Neoplasms benign, Basal cell carcinoma, malignant and Cutaneous squamous unspecified (incl. cysts cell carcinoma**, and polyps) Keratoacanthoma** Blood and lymphatic Anaemia system disorders Metabolism and Dehydration, nutrition disorders Hypophosphataemia, Hyponatremia, Hyperglycaemia Eye disorders Serous retinopathya, Visual impairment Blurred vision Vascular disorders Hypertension, Haemorrhage* Respiratory, thoracic Pneumonitis and mediastinal disorders Gastrointestinal Diarrhoea, Nausea, disorders Vomiting, Stomatitis Skin and subcutaneous Photosensitivityb, Rash, tissue disorders Rash maculo-papular, Dermatitis acneiform, Hyperkeratosis**, Pruritus c, Dry skin c Musculoskeletal and Rhabdomyolysis*** connective tissue disorders General disorders and Pyrexia, Chills, Oedema administration site peripheralc conditions Investigations Blood CPK increased, Ejection fraction ALT increased, AST decreased, Blood increased, Gamma- bilirubin increased Glutamyltransferase (GGT) increased, Blood ALP increased ^ Data cut-off date of 19 September 2014 * Please refer to the paragraph Haemorrhage in the “Description of selected adverse reactions” section ** Please refer to the paragraph Cutaneous squamous cell carcinoma, keratoacanthoma and hyperkeratosis in the “Description of selected adverse reactions” section. *** Please refer to the paragraph Rhabdomyolysis in the “Description of selected adverse reactions” section. a Includes both chorioretinopathy and retinal detachment events indicative of serous retinopathy (see section 4.4) b Combined figure includes reports of photosensitivity reaction, sunburn, solar dermatitis, actinic elastosis c ADRs identified in a cobimetinib monotherapy study (ML29733; US study). However, these were also reported ADRs for cobimetinib plus vemurafenib combination in clinical trials conducted in patients with unresectable or metastatic melanoma. Histiocytic Neoplasms The safety of Cotellic was evaluated in Study ML29733, a single-center single-arm trial in patients with histiocytic neoplasms (see section 5.1). In Study ML29733, 26 patients with histiocytic neoplasms received Cotellic 60 mg once daily for 21 days on, then 7 days off, in a 28-day treatment cycle. The median treatment duration was 10.7 months. Table 4 presents adverse reactions in at least 15% of patients reported with histiocytic neoplasms treated with Cotellic. Table 5 presents laboratory abnormalities of grades ≥3 reported in patients with histiocytic neoplasms treated Cotellic. In Study ML29733, 4 patients (15%) receiving Cotellic experienced an adverse reaction that resulted in permanent discontinuation of Cotellic. One patient discontinued due to worsening of underlying dyspnea and hypoxia; one patient discontinued due to retinal vascular disorder; one patient discontinued due to hyponatremia; and the other patient discontinued due to pneumonia. Table 4 Incidence of Adverse Reactions Reported Occurring in ≥15% (All Grades) or Any Percentage (Grade ≥3) in Patients with Histiocytic Neoplasms Treated with Cotellic in Study ML29733 All Grades* (%) Grades ≥3* (%) Body Systems (n=26) (n=26) Adverse reactions GASTROINTESTINAL DISORDERS Diarrhea 62 8 Nausea 46 0 Dyspepsia1 27 0 Vomiting 27 0 Dry Mouth 15 0 Oral pain2 15 0 GENERAL DISORDERS AND ADMINISTRATION SITE CONDITIONS Fatigue3 42 0 Edema4 42 4 Pain 15 0 INFECTIONS AND INFESTATIONS Infections5 62 23 Urinary tract infection 23 8 Pulmonary infections6 19 12 INJURY, POISONING AND PROCEDURAL COMPLICATIONS Fall 15 4 INVESTIGATIONS Decreased Ejection Fraction 19 12 RENAL AND URINARY Acute kidney injury 15 12 RESPIRATORY, THORACIC AND MEDIASTINAL DISORDERS Dyspnea 27 15 Cough 15 0 SKIN AND SUBCUTANEOUS TISSUE DISORDERS Acneiform dermatitis 65 0 Dry skin 31 0 Maculo-papular rash 31 0 Pruritus 31 4 VASCULAR DISORDERS Hemorrhage7 19 0 Hypertension 15 4 * NCI CTCAE v4.0. 1 Gastritis, and gastroesophageal reflux disease. 2 Oral dysesthesia and oropharyngeal pain. 3 Malaise 4 Facial edema, edema genital, edema peripheral, periorbital edema, and lymphoedema. 5 Influenza like illness, mucosal infection, paronychia, pharyngitis, pneumonia, bronchitis, sepsis, sinusitis, skin infection, tooth infection, upper respiratory tract infection., and urinary tract infection. 6 Pneumonia and bronchitis. 7 Epistaxis, contusion, purpura, hematoma, and rectal hemorrhage. The following clinically relevant adverse reactions (all grades) of Cotellic were reported with <15% incidence in Study ML29733: Eye disorders: Vision blurred (12%), retinal vascular disorder (4%) and retinopathy (4%). Gastrointestinal disorders: Stomatitis (12%) Nervous system disorders: Headache (12%) Respiratory, thoracic, and mediastinal disorders: Hypoxia (12%), pulmonary edema (4%), and respiratory failure (8%). Table 5 Incidence of Grade ≥3 Laboratory Abnormalities Occurring in Patients with Histiocytic Neoplasms Treated with Cotellic in Study ML29733* Grades 3–4a % Chemistry Increased blood creatine 27 phosphokinase Hyponatremia 18 Hypokalemia 12 Increased blood creatinine 9 Increased AST 9 Hypocalcemia 9 Increased ALT 5 Hematology Lymphopenia 27 Leukopenia 9 Anemia 8 Neutropenia 5 AST - aspartate aminotransferase, ALT - alanine aminotransferase *All the percentages are based on the number of patients who had a baseline result and at least one on-study laboratory test. a NCI CTCAE v4.0 Description of selected adverse reactions Haemorrhage Bleeding events have been reported more frequently in the Cotellic plus vemurafenib arm than in the placebo plus vemurafenib arm (all types and Grades: 13% vs 7%). The median time to first onset was 6.1 months in the Cotellic plus vemurafenib arm. The majority of events were Grade 1 or 2 and non-serious. Most events resolved with no change in Cotellic dose. Major haemorrhagic events (including intracranial and gastrointestinal tract haemorrhage) were reported in the post-marketing setting. The risk of haemorrhage may be increased with concomitant use of antiplatelet or anticoagulant therapy. If haemorrhage occurs, treat as clinically indicated (see section 4.2 and 4.4). In Study ML29733, in patients with histiocytic neoplasms, 19% of patients experienced haemorrhage events (all were of grade 1 severity). Rhabdomyolysis Rhabdomyolysis has been reported in the post-marketing setting. Signs or symptoms of rhabdomyolysis warrant an appropriate clinical evaluation and treatment as indicated, along with Cotellic dose modification or discontinuation according to the severity of the adverse reaction (see section 4.2 and 4.4). Photosensitivity Photosensitivity has been observed with a higher frequency in the Cotellic plus vemurafenib arm vs placebo plus vemurafenib arm (47% vs 35%). The majority of events were Grades 1 or 2, with Grade ≥3 events occurring in 4% of patients in the Cotellic plus vemurafenib arm vs 0% in the placebo plus vemurafenib arm. There were no apparent trends in the time of onset of Grade ≥3 events. Grade ≥3 photosensitivity events in the Cotellic plus vemurafenib arm were treated with primary topical medicinal products in conjunction with dose interruptions of both cobimetinib and vemurafenib (see section 4.2). No evidence of phototoxicity was observed with Cotellic as a single agent. Cutaneous squamous cell carcinoma, keratoacanthoma and hyperkeratosis Cutaneous squamous cell carcinoma has been reported with a lower frequency in the Cotellic plus vemurafenib arm vs placebo plus vemurafenib arm (all Grade: 3% vs 13%). Keratoacanthoma has been reported with a lower frequency in the Cotellic plus vemurafenib arm vs placebo plus vemurafenib arm (all Grade: 2% vs 9%). Hyperkeratosis has been reported with a lower frequency in the Cotellic plus vemurafenib vs placebo plus vemurafenib arm (all Grade: 11% vs 30%). Serous retinopathy Cases of serous retinopathy have been reported in patients treated with Cotellic (see section 4.4.) For patients reporting new or worsening visual disturbances, an ophthalmologic examination is recommended. Serous retinopathy can be managed with treatment interruption, dose reduction or with treatment discontinuation (see Table 1 in section 4.2). Left ventricular dysfunction Decrease in LVEF from baseline has been reported in patients receiving Cotellic (see section 4.4). LVEF should be evaluated before initiation of treatment to establish baseline values, then after the first month of treatment and at least every 3 months or as clinically indicated until treatment discontinuation. Decrease in LVEF from baseline can be managed using treatment interruption, dose reduction or with treatment discontinuation (see section 4.2). Laboratory abnormalities Liver laboratory abnormalities Liver laboratory abnormalities, specifically ALT, AST, and ALP have been observed in patients treated with Cotellic in combination with vemurafenib (see section 4.4). Liver laboratory tests should be monitored before initiation of combination treatment and monthly during treatment, or more frequently if clinically indicated (see section 4.2). Blood creatine phosphokinase increase Asymptomatic increases in blood CPK levels were observed with a higher frequency in the Cotellic plus vemurafenib arm vs placebo plus vemurafenib arm in Study GO28141 (see section 4.2 and 4.4). One event of rhabdomyolysis was observed in each treatment arm of the study with concurrent increases in blood CPK. Table 6 provides the frequency of measured liver laboratory abnormalities and elevated creatine phosphokinase for all Grades and Grades 3-4. Table 6 Liver function and other laboratory tests observed in the Phase III Study GO28141 Changes in reported Cobimetinib plus Placebo plus vemurafenib laboratory data vemurafenib (n = 246) (n = 247) (%) (%) All Grades Grades 3-4 All Grades Grades 3-4 Liver function test Increased ALP 69 7 55 3 Increased ALT 67 11 54 5 Increased AST 71 7 43 2 Increased GGT 62 20 59 17 Increased blood bilirubin 33 2 43 1 Other laboratory abnormalities Increased blood CPK 70 12 14 <1 In Study ML29733, in patients with histiocytic neoplasms, 27% of patients experienced grade 2 CPK elevation and 27% of patients experienced grade 3-4 CPK elevation. Special populations Elderly patients In the Phase III study with Cotellic in combination with vemurafenib in patients with unresectable or metastatic melanoma (n=247), 183 patients (74%) were <65 years of age, and 44 patients (18%) were 65-74 years of age, 16 (6%) were 75-84 years of age, and 4 patients (2%) were aged 85 years. The proportion of patients experiencing adverse events (AE) was similar in the patients aged 65 years and those aged 65 years. Patients ≥65 years were more likely to experience serious adverse events (SAEs) and experience AEs leading to discontinuation of cobimetinib than those 65 years. Paediatric population The safety of Cotellic in children and adolescents has not been fully established. The safety of Cotellic was assessed in a multi-centre, open-label, dose-escalation study in 55 paediatric patients aged 2 to 17 years with solid tumours. The safety profile of Cotellic in these patients was consistent with that in the adult population (see section 5.2). Renal impairment No pharmacokinetic trial in subjects with renal impairment has been conducted. Dose adjustment is not recommended for mild to moderate renal impairment based on the results of the population pharmacokinetic analysis. There are minimal data for Cotellic in patients with severe renal impairment. Cotellic should be used with caution in patients with severe renal impairment. Hepatic impairment No dose adjustment is recommended in patients with hepatic impairment (see section 5.2). Reporting of suspected adverse reactions Reporting suspected adverse reactions after authorisation of the medicinal product is important. It allows continued monitoring of the benefit/risk balance of the medicinal product. Any suspected adverse events should be reported to the Ministry of Health according to the National Regulation by using an online form: https://sideeffects.health.gov.il

פרטי מסגרת הכללה בסל
א. התרופה תינתן במקרים האלה:1. בשילוב עם Vemurafenib לטיפול במלנומה מתקדמת (גרורתית או שאיננה נתיחה) המבטאים מוטציה ב-BRAF. במהלך מחלתו יהיה החולה זכאי לטיפול בתרופה אחת בלבד מהתרופות המפורטות להלן - Binimetinib, Cobimetinib, Trametinib.לעניין זה מלנומה בשלב מתקדם (לא נתיח או גרורתי) לא תוגדר כאותה מחלה כמו מלנומה בשלב בר הסרה בניתוח.2. כמונותרפיה, לטיפול בחולים מבוגרים עם ממאירויות היסטיוציטיות (Histiocytic neoplasms).ב. מתן התרופה האמורה ייעשה לפי מרשם של רופא מומחה באונקולוגיה או רופא מומחה בהמטולוגיה.
מסגרת הכללה בסל
התוויות הכלולות במסגרת הסל
| התוויה | תאריך הכללה | תחום קליני | Class Effect | מצב מחלה |
|---|---|---|---|---|
| התרופה תינתן בשילוב עם Vemurafenib לטיפול במלנומה מתקדמת (גרורתית או שאיננה נתיחה) המבטאים מוטציה ב-BRAF. | ||||
| כמונותרפיה, לטיפול בחולים מבוגרים עם ממאירויות היסטיוציטיות (Histiocytic neoplasms). | 17/03/2024 | אונקולוגיה | ממאירויות היסטיוציטיות, Histiocytic neoplasms. |
שימוש לפי פנקס קופ''ח כללית 1994
לא צוין
תאריך הכללה מקורי בסל
12/01/2017
הגבלות
תרופה מוגבלת לרישום ע'י רופא מומחה או הגבלה אחרת
מידע נוסף
עלון מידע לצרכן
12.11.20 - עלון לצרכן אנגלית 12.11.20 - עלון לצרכן אנגלית 25.08.22 - עלון לצרכן עברית 12.11.20 - עלון לצרכן ערבית 12.11.20 - עלון לצרכן 21.09.20 - עלון לצרכן אנגלית 25.08.22 - עלון לצרכן עברית 21.09.20 - עלון לצרכן ערבית 11.10.22 - עלון לצרכן אנגלית 11.10.22 - עלון לצרכן עברית 11.10.22 - עלון לצרכן ערבית 08.03.23 - עלון לצרכן אנגלית 08.03.23 - עלון לצרכן עברית 08.03.23 - עלון לצרכן ערבית 25.10.23 - עלון לצרכן עברית 06.12.23 - עלון לצרכן אנגלית 06.12.23 - עלון לצרכן ערבית 11.04.24 - עלון לצרכן עברית 03.07.24 - עלון לצרכן אנגלית 06.07.24 - עלון לצרכן עברית 03.07.24 - עלון לצרכן ערבית 05.05.19 - החמרה לעלון 05.08.20 - החמרה לעלון 28.02.23 - החמרה לעלון 16.03.23 - החמרה לעלון 25.10.23 - החמרה לעלון 11.04.24 - החמרה לעלוןלתרופה במאגר משרד הבריאות
קוטליק