Quest for the right Drug
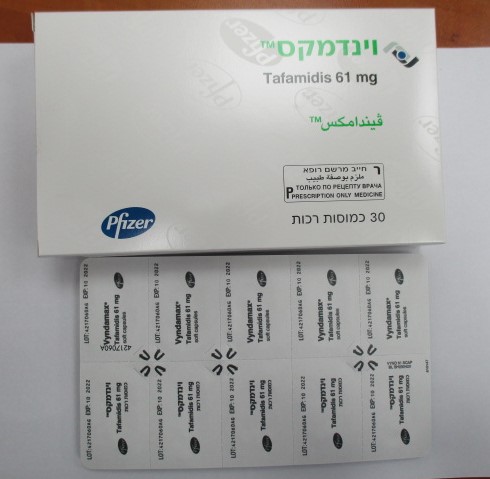
וינדמקס VYNDAMAX (TAFAMIDIS)
תרופה במרשם
תרופה בסל
נרקוטיקה
ציטוטוקסיקה
צורת מתן:
פומי : PER OS
צורת מינון:
קפסולות ג'לטין רכות : CAPSULES SOFT GELATIN
עלון לרופא
מינוניםPosology התוויות
Indications תופעות לוואי
Adverse reactions התוויות נגד
Contraindications אינטראקציות
Interactions מינון יתר
Overdose הריון/הנקה
Pregnancy & Lactation אוכלוסיות מיוחדות
Special populations תכונות פרמקולוגיות
Pharmacological properties מידע רוקחי
Pharmaceutical particulars אזהרת שימוש
Special Warning עלון לרופא
Physicians Leaflet
Pharmacological properties : תכונות פרמקולוגיות
Pharmacodynamic Properties
5.1 Pharmacodynamic properties Pharmacotherapeutic group: Other nervous system drugs, ATC code: N07XX08 Mechanism of action Tafamidis is a selective stabiliser of TTR. Tafamidis binds to TTR at the thyroxine binding sites, stabilising the tetramer and slowing dissociation into monomers, the rate-limiting step in the amyloidogenic process. Pharmacodynamic effects Transthyretin amyloidosis is a severely debilitating condition induced by the accumulation of various insoluble fibrillar proteins, or amyloid, within the tissues in amounts sufficient to impair normal function. The dissociation of the transthyretin tetramer to monomers is the rate-limiting step in the pathogenesis of transthyretin amyloidosis. The folded monomers undergo partial denaturation to produce alternatively folded monomeric amyloidogenic intermediates. These intermediates then misassemble into soluble oligomers, profilaments, filaments, and amyloid fibrils. Tafamidis binds with negative cooperativity to the two thyroxine binding sites on the native tetrameric form of transthyretin preventing dissociation into monomers. The inhibition of TTR tetramer dissociation forms the rationale for the use of tafamidis in ATTR-CM patients. A TTR stabilisation assay was utilised as a pharmacodynamic marker, and assessed the stability of the TTR tetramer. Tafamidis stabilised both the wild-type TTR tetramer and the tetramers of 14 TTR variants tested clinically after once-daily dosing with tafamidis. Tafamidis also stabilised the TTR tetramer for 25 variants tested ex vivo, thus demonstrating TTR stabilisation of 40 amyloidogenic TTR genotypes. In a multicentre, international, double-blind, placebo-controlled, randomised study (see Clinical efficacy and safety section), TTR stabilisation was observed at Month 1 and was maintained through Month 30. Biomarkers associated with heart failure (NT-proBNP and Troponin I) favoured tafamidis over placebo. Clinical efficacy and safety Efficacy was demonstrated in a multicentre, international, double-blind, placebo-controlled, randomised 3-arm study in 441 patients with wild-type or hereditary ATTR-CM. Patients were randomised to either tafamidis meglumine 20 mg (n=88) or 80 mg [administered as four 20 mg tafamidis meglumine capsules] (n=176) or matching placebo (n=177) once daily, in addition to standard of care (e.g. diuretics) for 30 months. Treatment assignment was stratified by the presence or absence of a variant TTR genotype as well as by baseline severity of disease (NYHA Class). Table 1 describes the patient demographics and baseline characteristics. Table 1: Patient demographics and baseline characteristics Characteristic Pooled Tafamidis Placebo N=264 N=177 Age — year Mean (standard deviation) 74.5 (7.2) 74.1 (6.7) Median (minimum, maximum) 75 (46, 88) 74 (51, 89) Sex — number (%) Male 241 (91.3) 157 (88.7) Female 23 (8.7) 20 (11.3) TTR genotype — number (%) ATTRm 63 (23.9) 43 (24.3) ATTRwt 201 (76.1) 134 (75.7) NYHA Class — number (%) NYHA Class I 24 (9.1) 13 (7.3) NYHA Class II 162 (61.4) 101 (57.1) NYHA Class III 78 (29.5) 63 (35.6) Abbreviations: ATTRm=variant transthyretin amyloid, ATTRwt=wild-type transthyretin amyloid, NYHA=New York Heart Association. The primary analysis used a hierarchical combination applying the method of Finkelstein-Schoenfeld (F-S) to all-cause mortality and frequency of cardiovascular-related hospitalisations, which is defined as the number of times a subject is hospitalised (i.e., admitted to a hospital) for cardiovascular-related morbidity. The method compared each patient to every other patient within each stratum in a pair-wise manner that proceeds in a hierarchical fashion using all-cause mortality followed by frequency of cardiovascular-related hospitalisations when patients cannot be differentiated based on mortality. This analysis demonstrated a significant reduction (p=0.0006) in all-cause mortality and frequency of cardiovascular-related hospitalisations in the pooled tafamidis 20 mg and 80 mg dose group versus placebo (Table 2). Table 2: Primary analysis using Finkelstein-Schoenfeld (F-S) Method of all-cause mortality and frequency of cardiovascular-related hospitalisations Primary analysis Pooled Tafamidis Placebo N=264 N=177 Number (%) of subjects alive* at month 30 186 (70.5) 101 (57.1) Average cardiovascular-related hospitalisations during 0.297 0.455 30 months (per patient per year) among those alive at month 30† p-value from F-S Method 0.0006 * Heart transplantation and cardiac mechanical assist device implantation are considered indicators of approaching end stage. As such, these subjects are treated in the analysis as equivalent to death. Therefore, such subjects are not included in the count of “Number of Subjects Alive at Month 30” even if such subjects are alive based on 30 month vital status follow-up assessment. † Descriptive mean among those who survived the 30 months. Analysis of the individual components of the primary analysis (all-cause mortality and cardiovascular-related hospitalisation) also demonstrated significant reductions for tafamidis versus placebo. The hazard ratio from the all-cause mortality Cox-proportional hazard model for pooled tafamidis was 0.698 (95% CI 0.508, 0.958), indicating a 30.2% reduction in the risk of death relative to the placebo group (p=0.0259). A Kaplan-Meier plot of time to event all-cause mortality is presented in Figure 1. Figure 1: All-cause mortality* * Heart transplants and cardiac mechanical assist devices treated as death. Hazard ratio from Cox-proportional hazards model with treatment, TTR genotype (variant and wild-type), and New York Heart Association (NYHA) Baseline classification (NYHA Classes I and II combined and NYHA Class III) as factors. There were significantly fewer cardiovascular-related hospitalisations with tafamidis compared with placebo with a reduction in risk of 32.4% (Table 3). Table 3: Cardiovascular-related hospitalisation frequency Pooled Tafamidis Placebo N=264 N=177 Total (%) number of subjects with 138 (52.3) 107 (60.5) Cardiovascular-related hospitalisations Cardiovascular-related hospitalisations per year* 0.4750 0.7025 Pooled tafamidis versus placebo treatment 0.6761 difference (relative risk ratio)* p-value* < 0.0001 Abbreviation: NYHA=New York Heart Association. * This analysis was based on a Poisson regression model with treatment, TTR genotype (variant and wild-type), New York Heart Association (NYHA) Baseline classification (NYHA Classes I and II combined and NYHA Class III), treatment-by-TTR genotype interaction, and treatment-by-NYHA Baseline classification interaction terms as factors. The treatment effect of tafamidis on functional capacity and health status was assessed by the 6-Minute Walk Test (6MWT) and the Kansas City Cardiomyopathy Questionnaire-Overall Summary (KCCQ-OS) score (composed of the Total Symptom, Physical Limitation, Quality of Life, and Social Limitation domains), respectively. A significant treatment effect favouring tafamidis was first observed at Month 6 and remained consistent through Month 30 on both the 6MWT distance and KCCQ-OS score (Table 4). Table 4: 6MWT and KCCQ-OS and component domain scores Endpoints Baseline Mean (SD) Change from Baseline to Treatment p-value Month 30, LS mean (SE) difference Pooled Placebo Pooled Placebo from placebo Tafamidis N=177 Tafamidis LS mean N=264 (95% CI) 6MWT* 350.55 353.26 -54.87 -130.55 75.68 p< 0.0001 (metres) (121.30) (125.98) (5.07) (9.80) (57.56, 93.80) KCCQ-OS* 67.27 65.90 -7.16 -20.81 13.65 p< 0.0001 (21.36) (21.74) (1.42) (1.97) (9.48, 17.83) * Higher values indicate better health status. Abbreviations: 6MWT=6-Minute Walk Test; KCCQ-OS=Kansas City Cardiomyopathy Questionnaire-Overall Summary; LS=least squares; CI=confidence interval. Results from F-S method represented by win ratio for the combined endpoint and its components (all-cause mortality and frequency of cardiovascular-related hospitalisation) consistently favoured tafamidis versus placebo by dose and across all subgroups (wild-type, variant and NYHA Class I & II, and III) except for cardiovascular-related hospitalisation frequency in NYHA Class III (Figure 2) which is higher in the tafamidis treated group compared to placebo (see section 4.2). Analyses of 6MWT and KCCQ-OS also favoured tafamidis relative to placebo within each subgroup. Figure 2: Results from F-S Method and components by subgroup and dose Abbreviations: ATTRm=variant transthyretin amyloid, ATTRwt=wild type transthyretin amyloid, F-S=Finkelstein-Schoenfeld, CI=Confidence Interval. * F-S results presented using win ratio (based on all-cause mortality and frequency of cardiovascular hospitalisation). The Win ratio is the number of pairs of treated-patient “wins” divided by number of pairs of placebo patient “wins.” Heart transplants and cardiac mechanical assist devices treated as death. In applying the F-S method to each dose group individually, tafamidis reduced the combination of all-cause mortality and frequency of cardiovascular-related hospitalisations for both the 80 mg and 20 mg doses compared to placebo (p=0.0030 and p=0.0048, respectively). Results of the primary analysis, 6MWT at Month 30 and KCCQ-OS at Month 30 were statistically significant for both the tafamidis meglumine 80 mg and 20 mg doses versus placebo, with similar results for both doses. Efficacy data for tafamidis 61 mg are not available as this formulation was not evaluated in the double-blind, placebo-controlled, randomised phase 3 study. The relative bioavailability of tafamidis 61 mg is similar to tafamidis meglumine 80 mg at steady-state (see section 5.2). A supra-therapeutic, single, 400 mg oral dose of tafamidis meglumine solution in healthy volunteers demonstrated no prolongation of the QTc interval.
Pharmacokinetic Properties
5.2 Pharmacokinetic properties Absorption After oral administration of the soft capsule once daily, the maximum peak concentration (Cmax) is achieved within a median time (tmax) of 4 hours for tafamidis 61 mg and 2 hours for tafamidis meglumine 80 mg (4 x 20 mg) after dosing in the fasted state. Concomitant administration of a high fat, high calorie meal altered the rate of absorption, but not the extent of absorption. These results support the administration of tafamidis with or without food. Distribution Tafamidis is highly protein bound (> 99%) in plasma. The apparent steady-state volume of distribution is 18.5 litres. The extent of tafamidis binding to plasma proteins has been evaluated using animal and human plasma. The affinity of tafamidis for TTR is greater than that for albumin. Therefore, in plasma, tafamidis is likely to bind preferentially to TTR despite the significantly higher concentration of albumin (600 μM) relative to TTR (3.6 μM). Biotransformation and elimination There is no explicit evidence of biliary excretion of tafamidis in humans. Based on preclinical data, it is suggested that tafamidis is metabolised by glucuronidation and excreted via the bile. This route of biotransformation is plausible in humans, as approximately 59% of the total administered dose is recovered in faeces, and approximately 22% recovered in urine. Based on population pharmacokinetic results, the apparent oral clearance of tafamidis is 0.263 L/h and the population mean half-life is approximately 49 hours. Dose and time linearity Exposure from once-daily dosing with tafamidis meglumine increased with increasing dose up to 480 mg single dose and multiple doses up to 80 mg/day. In general, increases were proportional or near proportional to dose and tafamidis clearance was stationary over time. The relative bioavailability of tafamidis 61 mg is similar to tafamidis meglumine 80 mg at steady-state. Tafamidis and tafamidis meglumine are not interchangeable on a per mg basis. Pharmacokinetic parameters were similar after single and repeated administration of 20 mg dose of tafamidis meglumine, indicating a lack of induction or inhibition of tafamidis metabolism. Results of once-daily dosing with 15 mg to 60 mg oral solution tafamidis meglumine for 14 days demonstrated that steady-state was achieved by Day 14. Special populations Hepatic impairment Pharmacokinetic data indicated decreased systemic exposure (approximately 40%) and increased total clearance (0.52 L/h versus 0.31 L/h) of tafamidis meglumine in patients with moderate hepatic impairment (Child-Pugh Score of 7-9 inclusive) compared to healthy subjects due to a higher unbound fraction of tafamidis. As patients with moderate hepatic impairment have lower TTR levels than healthy subjects, dosage adjustment is not necessary as the stoichiometry of tafamidis with its target protein TTR would be sufficient for stabilisation of the TTR tetramer. The exposure to tafamidis in patients with severe hepatic impairment is unknown. Renal impairment Tafamidis has not specifically been evaluated in a dedicated study of patients with renal impairment. The influence of creatinine clearance on tafamidis pharmacokinetics was evaluated in a population pharmacokinetic analysis in patients with creatinine clearance greater than 18 mL/min. Pharmacokinetic estimates indicated no difference in apparent oral clearance of tafamidis in patients with creatinine clearance less than 80 mL/min compared to those with creatinine clearance greater than or equal to 80 mL/min. Dosage adjustment in patients with renal impairment is considered not necessary. Elderly Based on population pharmacokinetic results, subjects ≥ 65 years had an average 15% lower estimate of apparent oral clearance at steady-state compared to subjects less than 65 years old. However, the difference in clearance results in < 20% increases in mean Cmax and AUC compared to younger subjects and is not clinically significant. Pharmacokinetic/pharmacodynamic relationships In vitro data indicated that tafamidis does not significantly inhibit cytochrome P450 enzymes CYP1A2, CYP3A4, CYP3A5, CYP2B6, CYP2C8, CYP2C9, CYP2C19, and CYP2D6. Tafamidis is not expected to cause clinically relevant drug interaction due to induction of CYP1A2, CYP2B6 or CYP3A4. In vitro studies suggest that it is unlikely tafamidis will cause drug interactions at clinically relevant concentrations with substrates of UDP glucuronosyltransferase (UGT) systemically. Tafamidis may inhibit intestinal activities of UGT1A1. Tafamidis showed a low potential to inhibit Multi-Drug Resistant Protein (MDR1) (also known as P-glycoprotein; P-gp) systemically and in the gastrointestinal (GI) tract, organic cation transporter 2 (OCT2), multidrug and toxin extrusion transporter 1 (MATE1) and MATE2K, organic anion transporting polypeptide 1B1 (OATP1B1) and OATP1B3 at clinically relevant concentrations.

פרטי מסגרת הכללה בסל
א. התרופה תינתן לטיפול בחולים העונים על כל אלה:1. קרדיומיופתיה מסוג wild type or hereditary transthyretin-mediated amyloidosis (ATTR-CM) 2. אבחנה של ATTR. לעניין זה אבחנה של ATTR תקבע על פי שני התנאים הבאים:א. קליניקה אופיינית ובדיקות דימות (אקו או MRI) ב. קליטה דרגה 2 או 3 במיפוי עם bone-seeking tracers .במידה ושני התנאים דלעיל לא מתקיימים במלואם וקיים חשד קליני משמעותי יש להמשיך לבירור בביופסיה והאבחנה תקבע על פיה.3. דרגות תפקוד NYHA 1 או NYHA 2 או NYHA 3.ב. מתן התרופה ייעשה לפי מרשם של רופא מומחה בקרדיולוגיה.
מסגרת הכללה בסל
התוויות הכלולות במסגרת הסל
| התוויה | תאריך הכללה | תחום קליני | Class Effect | מצב מחלה |
|---|---|---|---|---|
| א. התרופה תינתן לטיפול בחולים העונים על כל אלה: 1. קרדיומיופתיה מסוג wild type or hereditary transthyretin-mediated amyloidosis (ATTR-CM) 2. אבחנה של ATTR. לעניין זה אבחנה של ATTR תקבע על פי שני התנאים הבאים: א. קליניקה אופיינית ובדיקות דימות (אקו או MRI) ב. קליטה דרגה 2 או 3 במיפוי עם bone-seeking tracers . במידה ושני התנאים דלעיל לא מתקיימים במלואם וקיים חשד קליני משמעותי יש להמשיך לבירור בביופסיה והאבחנה תקבע על פיה. 3. דרגות תפקוד NYHA 1 או NYHA 2. ב. מתן התרופה ייעשה לפי מרשם של רופא מומחה בקרדיולוגיה. | 01/03/2021 | לב וכלי דם | קרדיומיופתיה מסוג wild type or hereditary transthyretin-mediated amyloidosis (ATTR-CM) | |
| א. התרופה תינתן לטיפול בחולים העונים על כל אלה: 1. קרדיומיופתיה מסוג wild type or hereditary transthyretin-mediated amyloidosis (ATTR-CM) 2. אבחנה של ATTR. לעניין זה אבחנה של ATTR תקבע על פי שני התנאים הבאים: א. קליניקה אופיינית ובדיקות דימות (אקו או MRI) ב. קליטה דרגה 2 או 3 במיפוי עם bone-seeking tracers . במידה ושני התנאים דלעיל לא מתקיימים במלואם וקיים חשד קליני משמעותי יש להמשיך לבירור בביופסיה והאבחנה תקבע על פיה. 3. דרגות תפקוד NYHA 1 או NYHA 2 או NYHA 3. ב. מתן התרופה ייעשה לפי מרשם של רופא מומחה בקרדיולוגיה. | 03/02/2022 | לב וכלי דם | קרדיומיופתיה מסוג wild type or hereditary transthyretin-mediated amyloidosis (ATTR-CM) |
שימוש לפי פנקס קופ''ח כללית 1994
לא צוין
תאריך הכללה מקורי בסל
01/03/2021
הגבלות
תרופה מוגבלת לרישום ע'י רופא מומחה או הגבלה אחרת
מידע נוסף
