Quest for the right Drug
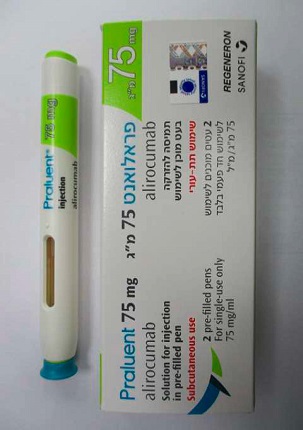
פראלואנט 75 מ"ג/מ"ל PRALUENT 75 MG/ML (ALIROCUMAB)
תרופה במרשם
תרופה בסל
נרקוטיקה
ציטוטוקסיקה
צורת מתן:
תת-עורי : S.C
צורת מינון:
תמיסה להזרקה : SOLUTION FOR INJECTION
עלון לרופא
מינוניםPosology התוויות
Indications תופעות לוואי
Adverse reactions התוויות נגד
Contraindications אינטראקציות
Interactions מינון יתר
Overdose הריון/הנקה
Pregnancy & Lactation אוכלוסיות מיוחדות
Special populations תכונות פרמקולוגיות
Pharmacological properties מידע רוקחי
Pharmaceutical particulars אזהרת שימוש
Special Warning עלון לרופא
Physicians Leaflet
Pharmacological properties : תכונות פרמקולוגיות
Pharmacodynamic Properties
5.1 Pharmacodynamic properties Pharmacotherapeutic group: lipid modifying agents, other lipid modifying agents, ATC code: C10AX14. Mechanism of action Alirocumab is a fully human IgG1 monoclonal antibody that binds with high affinity and specificity to proprotein convertase subtilisin kexin type 9 (PCSK9). PCSK9 binds to the low-density lipoprotein receptors (LDLR) on the surface of hepatocytes to promote LDLR degradation within the liver. LDLR is the primary receptor that clears circulating LDL, therefore the decrease in LDLR levels by PCSK9 results in higher blood levels of LDL-C. By inhibiting the binding of PCSK9 to LDLR, alirocumab increases the number of LDLRs available to clear LDL, thereby lowering LDL-C levels. The LDLR also binds triglyceride-rich VLDL remnant lipoproteins and intermediate-density lipoprotein (IDL). Therefore, alirocumab treatment can produce reductions in these remnant lipoproteins as evidenced by its reductions in apolipoprotein B (Apo B), non-high-density lipoprotein cholesterol (non- HDL-C) and triglycerides (TG). Alirocumab also results in reductions in lipoprotein (a) [Lp(a)], which is a form of LDL that is bound to apolipoprotein (a). However, the LDLR has been shown to have a low affinity for Lp(a), therefore the exact mechanism by which alirocumab lowers Lp(a) is not fully understood. In genetic studies in humans, PCSK9 variants with either loss-of-function or gain-of-function mutations have been identified. Individuals with single allele PCSK9 loss-of-function mutation have lower levels of LDL-C, which correlated with a significantly lower incidence of coronary heart disease. A few individuals have been reported, who carry PCSK9 loss-of-function mutations in two alleles and have profoundly low LDL-C levels, with HDL-C and TG levels in the normal range. Conversely, gain-of- function mutations in the PCSK9 gene have been identified in patients with increased LDL-C levels and a clinical diagnosis of familial hypercholesterolaemia. In a multicenter, double-blind, placebo-controlled, 14 week study, 13 patients with heterozygous familial hypercholesterolaemia (heFH) due to gain-of-function mutations in the PCSK9 gene were randomised to receive either alirocumab 150 mg Q2W or placebo. Mean baseline LDL-C was 151.5 mg/dL (3.90 mmol/L). At week 2, the mean reduction from baseline in LDL-C was 62.5% in the alirocumab-treated patients as compared to 8.8% in the placebo patients. At week 8, the mean reduction in LDL-C from baseline with all patients treated with alirocumab was 72.4%. Pharmacodynamic effects In in vitro assays, alirocumab did not induce Fc-mediated effector function activity (antibody-dependent cell-mediated toxicity and complement-dependent cytotoxicity) either in the presence or absence of PCSK9 and no soluble immune complexes capable of binding complement proteins were observed for alirocumab when bound to PCSK9. Clinical efficacy and safety in primary hypercholesterolaemia and mixed dyslipidaemia Summary of the Phase 3 Clinical Trials Program - 75 mg and/or 150 mg every 2 weeks (Q2W) dosing regimen The efficacy of alirocumab was investigated in ten phase 3 trials (five placebo-controlled and five ezetimibe-controlled studies), involving 5,296 randomized patients with hypercholesterolaemia (heterozygous familial and non-familial) or mixed dyslipidaemia, with 3,188 patients randomized to alirocumab. In the phase 3 studies, 31% of patients had type 2 diabetes mellitus, and 64% of patients had a history of coronary heart disease. Three of the ten studies were conducted exclusively in patients with heterozygous familial hypercholesterolaemia (heFH). The majority of patients in the phase 3 program were taking background lipid-modifying therapy consisting of a maximally tolerated dose of statin, with or without other lipid-modifying therapies, and were at high or very high cardiovascular (CV) risk. Two studies were conducted in patients who were not concomitantly treated with a statin, including one study in patients with documented statin intolerance. Two studies (LONG TERM and HIGH FH), involving a total of 2,416 patients, were performed with a 150 mg every 2 weeks (Q2W) dose only. Eight studies were performed with a dose of 75 mg Q2W, and criteria-based up-titration to 150 mg Q2W at week 12 in patients who did not achieve their pre-defined target LDL-C based on their level of CV risk at week 8. The primary efficacy endpoint in all of the phase 3 studies was the mean percent reduction from baseline in LDL-C at week 24 as compared to placebo or ezetimibe. All of the studies met their primary endpoint. In general, administration of alirocumab also resulted in a statistically significant greater percent reduction in total cholesterol (Total-C), non-high-density lipoprotein cholesterol (non-HDL-C), apolipoprotein B (Apo B), and lipoprotein (a) [Lp(a)] as compared to placebo/ ezetimibe, whether or not patients were concomitantly being treated with a statin. Alirocumab also reduced triglycerides (TG), and increased high-density lipoprotein cholesterol (HDL-C) and apolipoprotein A-1 (Apo A-1) as compared to placebo. For detailed results see Table 2 below. Reduction in LDL-C was seen across age, gender, body mass index (BMI), race, baseline LDL-C levels, patients with heFH and non-heFH, patients with mixed dyslipidaemia, and diabetic patients. Although similar efficacy was observed in patients over 75 years, data are limited in this age group. LDL-C reduction was consistent regardless of concomitantly used statins and doses. A significantly higher proportion of patients achieved an LDL-C of ˂70 mg/dL (˂1.81 mmol/L) in the alirocumab group as compared to placebo or ezetimibe at week 12 and week 24. In studies using the criteria-based up-titration regimen, a majority of patients achieved the pre-defined target LDL-C (based on their level of CV risk) on the 75 mg Q2W dose, and a majority of patients maintained treatment on the 75 mg Q2W dose. The lipid-lowering effect of alirocumab was observed within 15 days after the first dose reaching maximum effect at approximately 4 weeks. With long-term treatment, efficacy was sustained over the duration of the studies (up to 2 years. Following discontinuation of alirocumab, no rebound in LDL-C was observed, and LDL-C levels gradually returned to baseline levels. In pre-specified analyses before possible up-titration at week 12 in the 8 studies in which patients started with the 75 mg every 2 weeks dosing regimen, mean reductions in LDL-C ranging from 44.5% to 49.2% were achieved. In the 2 studies in which patients were started and maintained on 150 mg every 2 weeks, the achieved mean reduction of LDL-C at week 12 was 62.6%. In analyses of pooled phase 3 studies that allowed up-titration, among the subgroup of patients up-titrated, an increase from 75 mg Q2W to 150 mg Q2W alirocumab at week 12 resulted in an additional 14% mean reduction in LDL-C in patients on a background statin. In patients not on a background statin, up-titration of alirocumab resulted in an additional 3% mean reduction in LDL-C, with the majority of the effect seen in approximately 25% of patients who achieved at least an additional 10% LDL-C lowering after up-titration. Patients up-titrated to 150 mg Q2W had a higher mean baseline LDL-C. Evaluation of cardiovascular (CV) events In pre-specified analyses of pooled phase 3 studies, treatment-emergent CV events confirmed by adjudication, consisting of coronary heart disease (CHD) death, myocardial infarction, ischemic stroke, unstable angina requiring hospitalisation, congestive heart failure hospitalisation, and revascularisation, were reported in 110 (3.5%) patients in the alirocumab group and 53 (3.0%) patients in the control group (placebo or active control) with HR=1.08 (95% CI, 0.78 to 1.50). Major adverse cardiovascular events (“MACE- plus”, i.e.: CHD death, myocardial infarction, ischemic stroke, and unstable angina requiring hospitalisation) confirmed by adjudication were reported in 52 of 3,182 (1.6%) patients in the alirocumab group and 33 of 1,792 (1.8%) patients in the control group (placebo or active control); HR=0.81 (95% CI, 0.52 to 1.25). In pre-specified final analyses of the LONG TERM study, treatment-emergent CV events confirmed by adjudication occurred in 72 of 1,550 (4.6%) patients in the alirocumab group and in 40 of 788 (5.1%) patients in the placebo group; MACE-plus confirmed by adjudication were reported in 27 of 1,550 (1.7%) patients in the alirocumab group and 26 of 788 (3.3%) patients in the placebo group. Hazard ratios were calculated post-hoc; for all CV events, HR=0.91 (95% CI, 0.62 to 1.34); for MACE-plus, HR=0.52 (95% CI, 0.31 to 0.90). All-cause mortality All-cause mortality in phase 3 studies was 0.6% (20 of 3,182 patients) in the alirocumab group and 0.9% (17 of 1,792 patients) in the control group. The primary cause of death in the majority of these patients was CV events. Combination therapy with a statin Placebo-controlled phase 3 studies (on background statin) in patients with primary hypercholesterolaemia or mixed dyslipidaemia LONG TERM study This multicenter, double-blind, placebo-controlled, 18-month study included 2,310 patients with primary hypercholesterolaemia at high or very high CV risk and on a maximally tolerated dose of statin, with or without other lipid-modifying therapy. Patients received either alirocumab at a dose of 150 mg Q2W or placebo in addition to their existing lipid-modifying therapy. The LONG TERM study included 17.7% heFH patients, 34.6% with type 2 diabetes mellitus, and 68.6% with a history of coronary heart disease. At week 24, the mean treatment difference from placebo in LDL-C percent change from baseline was - 61.9% (95% CI: -64.3%, -59.4%; p-value: ˂0.0001). For detailed results see Table 2. At week 12, 82.1% of patients in the alirocumab group reached an LDL-C ˂70 mg/dL (˂1.81 mmol/L) compared to 7.2% of patients in the placebo group. Difference versus placebo was statistically significant at week 24 for all lipids/ lipoproteins. COMBO I study A multicenter, double-blind, placebo-controlled, 52 week study included 311 patients categorised as very high CV risk and not at their pre-defined target LDL-C on a maximally tolerated dose of statin, with or without other lipid-modifying therapy. Patients received either 75 mg alirocumab Q2W or placebo in addition to their existing lipid-modifying therapy. Dose up-titration of alirocumab to 150 mg Q2W occurred at week 12 in patients with LDL-C ≥70 mg/dL (≥1.81 mmol/L). At week 24, the mean treatment difference from placebo in LDL-C percent change from baseline was -45.9% (95% CI: - 52.5%, -39.3%; p-value: ˂0.0001). For detailed results see Table 4. At week 12 (before up-titration), 76.0% of patients in the alirocumab group reached an LDL-C of ˂70 mg/dL (˂ 1.81 mmol/L) as compared to 11.3% in the placebo group. The dose was up-titrated to 150 mg Q2W in 32 (16.8%) patients treated beyond 12 weeks. Among the subgroup of patients up-titrated at week 12, an additional 22.8% mean reduction in LDL-C was achieved at week 24. The difference versus placebo was statistically significant at week 24 for all lipids/ lipoproteins except TG and Apo A-1. Placebo-controlled phase 3 studies (on background statin) in patients with heterozygous familial hypercholesterolaemia (heFH) FH I and FH II studies Two multicenter, placebo-controlled, double-blind 18-month studies included 732 patients with heFH receiving a maximally tolerated dose of statin, with or without other lipid-modifying therapy. Patients received either alirocumab 75 mg Q2W or placebo in addition to their existing lipid-modifying therapy. Dose up-titration of alirocumab to 150 mg Q2W occurred at week 12 in patients with LDL-C ≥70 mg/dL (≥1.81 mmol/L). At week 24, the mean treatment difference from placebo in LDL-C percent change from baseline was -55.8% (95% CI: -60.0%, -51.6%; p-value: ˂ 0.0001). For detailed results see Table 2. At week 12 (before up-titration), 50.2% of patients reached an LDL-C of ˂70 mg/dL (˂1.81 mmol/L) as compared to 0.6% in the placebo group. Among the subgroup of patients up-titrated at week 12, an additional 15.7% mean reduction in LDL-C was achieved at week 24. Difference versus placebo was statistically significant at week 24 for all lipids/ lipoproteins. HIGH FH study A third multicenter, double-blind, placebo-controlled 18-month study included 106 heFH patients on a maximally tolerated dose of statin, with or without other lipid-modifying therapies, and a baseline LDL- C ≥160 mg/dL (≥4.14 mmol/L). Patients received either alirocumab at a dose of 150 mg Q2W or placebo in addition to their existing lipid-modifying therapy. At week 24, the mean treatment difference from placebo in LDL-C percent change from baseline was -39.1% (95% CI: -51.1%, -27.1%; p-value: ˂0.0001). For detailed results see Table 2. Mean changes for all other lipids/ lipoproteins were similar to the FH I and FH II studies, however statistical significance was not reached for TG, HDL-C and Apo A- 1. Ezetimibe-controlled phase 3 study (on background statin) in patients with primary hypercholesterolaemia or mixed dyslipidaemia COMBO II study A multicenter, double-blind, ezetimibe-controlled 2 year study included 707 patients categorised as very high CV risk and not at their pre-defined target LDL-C on a maximally tolerated dose of statin. Patients received either alirocumab 75 mg Q2W or ezetimibe 10 mg once daily in addition to their existing statin therapy. Dose up-titration of alirocumab to 150 mg Q2W occurred at week 12 in patients with LDL-C ≥70 mg/dL (≥1.81 mmol/L). At week 24, the mean treatment difference from ezetimibe in LDL-C percent change from baseline was -29.8% (95% CI: -34.4%, -25.3%; p-value: ˂0.0001). For detailed results see Table 2. At week 12 (before up-titration), 77.2% of patients reached an LDL-C of ˂70 mg/dL (˂1.81 mmol/L) as compared to 46.2% in the ezetimibe group. Among the subgroup of patients up- titrated at week 12, an additional 10.5% mean reduction in LDL-C was achieved at week 24. Difference versus ezetimibe was statistically significant at week 24 for all lipids/ lipoproteins except for TG, and Apo A-1. Monotherapy or as add-on to non-statin lipid-modifying therapy Ezetimibe-controlled phase 3 trials in patients with primary hypercholesterolaemia (without a background statin) ALTERNATIVE study A multicentre, double-blind, ezetimibe-controlled, 24 week study included 248 patients with documented statin intolerance due to skeletal muscle-related symptoms. Patients received either alirocumab 75 mg Q2W or ezetimibe 10 mg once daily, or atorvastatin 20 mg once daily (as a re- challenge arm). Dose up-titration of alirocumab to 150 mg Q2W occurred at week 12 in patients with LDL-C ≥70 mg/dL (≥1.81 mmol/L) or ≥100 mg/dL (≥2.59 mmol/L), depending on their level of CV risk. At week 24, the mean treatment difference from ezetimibe in LDL-C percent change from baseline was -30.4% (95% CI: -36.6%, -24.2%; p-value: ˂0.0001). For detailed results see Table 2. At week 12 (before up-titration), 34.9% of patients reached an LDL-C of ˂70 mg/dL (˂1.81 mmol/L) as compared to 0% in the ezetimibe group. Among the subgroup of patients up-titrated at week 12, an additional 3.6% mean reduction in LDL-C was achieved at week 24. Difference versus ezetimibe was statistically significant at week 24 for LDL-C, Total-C, Non-HDL-C, Apo B, and Lp(a). This trial evaluated patients who did not tolerate at least two statins (at least one at the lowest approved dose). In these patients, musculo-skeletal adverse events occurred at a lower rate in the alirocumab group (32.5%) as compared to the atorvastatin group (46.0%) (HR= 0.61 [95% CI, 0.38 to 0.99]), and a lower percentage of patients in the alirocumab group (15.9%) discontinued study treatment due to musculo-skeletal adverse events as compared to the atorvastatin group (22.2%). In the five placebo- controlled trials in patients on a maximally tolerated dose of statin (n=3752), the discontinuation rate due to musculo-skeletal adverse events was 0.4% in the alirocumab group and 0.5% in the placebo group. MONO study A multicenter, double-blind, ezetimibe-controlled, 24 week study included 103 patients with a moderate CV risk, not taking statins or other lipid-modifying therapies, and a baseline LDL-C between 100 mg/dL (2.59 mmol/L) to 190 mg/dL (4.91 mmol/L). Patients received either alirocumab 75 mg Q2W or ezetimibe 10 mg once daily. Dose up-titration of alirocumab to 150 mg Q2W occurred at week 12 in patients with LDL-C ≥70 mg/dL (≥1.81 mmol/L). At week 24, the mean treatment difference from ezetimibe in LDL-C percent change from baseline was -31.6% (95% CI: -40.2%, -23.0%; p-value: ˂0.0001). For detailed results see Table 2. At week 12 (before up-titration), 57.7% of patients reached an LDL-C of ˂70 mg/dL (˂1.81 mmol/L) as compared to 0% in the ezetimibe group. The dose was up- titrated to 150 mg Q2W in 14 (30.4%) patients treated beyond 12 weeks. Among the subgroup of patients up-titrated at week 12, an additional 1.4 % mean reduction in LDL-C was achieved at week 24. The difference versus ezetimibe was statistically significant at week 24 for LDL-C, Total-C, Non-HDL- C and Apo B. Table 2: Mean percent change from baseline in LDL-C and other lipids/ lipoproteins in placebo- controlled and ezetimibe-controlled studies – 75 mg and/or 150 mg Q2W dosing regimen Mean Percent Change from Baseline in Placebo-Controlled Studies on Background Statin LONG TERM FHI and FHII (N=732) High FH (N=106) COMBO I (N=311) (N=2310) Placebo Alirocumab Placebo Alirocumab Placebo Alirocumab Placebo Alirocumab Number 780 1530 244 488 35 71 106 205 of patients Mean 122.0 122.8 140.9 141.3 201.0 196.3 104.6 100.3 Baseline (3.16) (3.18) (3.65) (3.66) (5.21) (5.10) (2.71) (2.60) LDL-C in mg/dL (mmol/L) Week 12 LDL-C 1.5 -63.3 5.4 -43.6 -6.6 -46.9 1.1 -46.3 (ITT)a LDL-C (on 1.4 -64.2 5.3 -44.0 -6.6 -46.9 1.7 -47.6 treatmen t)b Week 24 LDL-C 0.8 -61.0c 7.1 -48.8d -6.6 -45.7e -2.3 -48.2f (ITT)a LDL-C (on 0.7 -62.8 6.8 -49.3 -6.6 -45.5 -0.8 -50.7 treatmen t)b Non-HDL- 0.7 -51.6 7.4 -42.8 -6.2 -41.9 -1.6 -39.1 C Apo B 1.2 -52.8 1.9 -41.7 -8.7 -39.0 -0.9 -36.7 Total-C -0.3 -37.8 5.5 -31.2 -4.8 -33.2 -2.9 -27.9 Lp(a) -3.7 -29.3 -8.5 -26.9 -8.7 -23.5 -5.9 -20.5 TG 1.8 -15.6 4.3 -9.8 -1.9 -10.5 -5.4 -6.0 HDL-C -0.6 4.0 0.2 7.8 3.9 7.5 -3.8 3.5 Apo A-1 1.2 4.0 -0.4 4.2 2.0 5.6 -2.5 3.3 Mean percent change from baseline in ezetimibe-controlled studies On background statin Without background statin COMBO II (N=707) ALTERNATIVE (N=248) MONO (N=103) Ezetimibe Alirocumab Ezetimibe Alirocumab Ezetimibe Alirocumab Number of 240 467 122 126 51 52 patients Mean 104.5 108.3 194.2 191.1 138.3 141.1 baseline LDL-C (2.71) (2.81) (5.03) (5.0) (3.58) (3.65) in mg/dL (mmol/L) Week 12 LDL-C -21.8 -51.2 -15.6 -47.0 -19.6 -48.1 (ITT)a LDL-C (on -22.7 -52.4 -18.0 -51.2 -20.4 -53.2 treatment)b Week 24 LDL-C -20.7 -50.6g -14.6 -45.0h -15.6 -47.2i (ITT) a LDL-C (on -21.8 -52.4 -17.1 -52.2 -17.2 -54.1 treatment)b Non-HDL-C -19.2 -42.1 -14.6 -40.2 -15.1 -40.6 Apo B -18.3 -40.7 -11.2 -36.3 -11.0 -36.7 Total-C -14.6 -29.3 -10.9 -31.8 -10.9 -29.6 Lp(a) -6.1 -27.8 -7.3 -25.9 -12.3 -16.7 TG -12.8 -13.0 -3.6 -9.3 -10.8 -11.9 HDL-C 0.5 8.6 6.8 7.7 1.6 6.0 Apo A-1 -1.3 5.0 2.9 4.8 -0.6 4.7 a ITT analysis – intent-to-treat population, includes all lipid data throughout the duration of the study irrespective of adherence to the study treatment. b On-treatment analysis – analysis restricted to the time period that patients actually received treatment. The % LDL-C reduction at week 24 corresponds to a mean absolute change of: c -74.2 mg/dL (-1.92 mmol/L); d -71.1 mg/dL (-1.84 mmol/L); e -90.8 mg/dL (-2.35 mmol/L); f -50.3 mg/dL (-1.30 mmol/L); g -55.4 mg/dL (1.44 mmol/L) ;h -84.2 mg/dL (-2.18 mmol/L); i -66.9 mg/dL (-1.73 mmol/L) Every 4 week (Q4W) dosing regimen CHOICE I study A multicenter, double-blind, placebo-controlled, 48 week study included 540 patients on a maximally tolerated dose of a statin, with or without other lipid-modifying therapy (308 in the alirocumab 300 mg Q4W group, 76 in the alirocumab 75 mg Q2W group, and 156 in the placebo group), and 252 patients not treated with a statin (144 in the alirocumab 300 mg Q4W group, 37 in the alirocumab 75 mg Q2W group, and 71 in the placebo group). Patients received either alirocumab 300 mg Q4W, alirocumab 75 mg Q2W, or placebo in addition to their existing lipid-modifying therapy (statin, non-statin therapy or diet alone). Patients in the alirocumab 300 mg every 4 weeks treatment group received alternating placebo injections to maintain blinding in regard to injection frequency. Overall, 71.6% of patients were categorized at high or very high CV risk and not at their LDL-C target. Dose adjustment in the alirocumab groups to 150 mg Q2W occurred at week 12 in patients with LDL-C ≥70 mg/dL or ≥100 mg/dL, depending on their level of CV risk, or in patients who did not have at least a 30% reduction of LDL-C from baseline. In the cohort of patients on background statin, the mean baseline LDL-C was 112.7 mg/dL. At week 12, the mean percent change from baseline with alirocumab 300 mg Q4W in LDL-C (ITT analysis) was - 55.3% compared to +1.1% for placebo. At week 12 (before dose adjustment), 77.3% of patients treated with alirocumab 300 mg Q4W reached an LDL-C of ˂70 mg/dL as compared to 9.3% in the placebo group. At week 24, the mean percent change from baseline with alirocumab 300 mg Q4W/150 mg Q2W in LDL-C (ITT analysis) was -58.8% compared to -0.1% for placebo. At week 24, the mean treatment difference for alirocumab 300 mg Q4W/150 mg Q2W from placebo in LDL-C percent change from baseline was -58.7% (97.5% CI: -65.0%, -52.4%; p-value: ˂ 0.0001). In patients treated beyond 12 weeks, the dose was adjusted to 150 mg Q2W in 56 (19.3%) of 290 patients in the alirocumab 300 mg Q4W arm. Among the subgroup of patients dose adjusted to 150 mg Q2W at week 12, an additional 25.4% reduction in LDL-C was achieved at week 24. In the cohort of patients not treated with a concomitant statin, the mean baseline LDL-C was 142.1 mg/dL. At week 12, the mean percent change from baseline with alirocumab 300 mg Q4W in LDL-C (ITT analysis) was -58.4% compared to +0.3% for placebo. At week 12 (before dose adjustment), 65.2% of patients treated with alirocumab 300 mg Q4W reached an LDL-C of ˂70 mg/dL as compared to 2.8% in the placebo group. At week 24, the mean percent change from baseline with alirocumab 300 mg Q4W/150 mg Q2W in LDL-C (ITT analysis) was -52.7% compared to -0.3% for placebo. At week 24, the mean treatment difference for alirocumab 300 mg Q4W/150 mg Q2W from placebo in LDL-C percent change from baseline was -52.4% (97.5% CI: -59.8%, -45.0%; p-value: ˂ 0.0001). In patients treated beyond 12 weeks, the dose was adjusted to 150 mg Q2W in 19 (14.7%) of 129 patients in the alirocumab 300 mg Q4W arm. Among the subgroup of patients dose adjusted to 150 mg Q2W at week 12, an additional 7.3% mean reduction in LDL-C was achieved at week 24. In both cohorts, the difference vs placebo was statistically significant at week 24 for all lipid parameters, except for Apo A-1 in the subgroup of patients on background statin. Clinical efficacy and safety in prevention of cardiovascular events ODYSSEY OUTCOMES study A multicentre, double-blind, placebo-controlled trial included 18,924 adult patients (9,462 alirocumab; 9,462 placebo) followed for up to 5 years. Patients had experienced an acute coronary syndrome (ACS) event 4 to 52 weeks prior to randomization and were treated with a lipid-modifying-therapy (LMT) regimen that was statin- intensive (defined as atorvastatin 40 or 80 mg, or rosuvastatin 20 or 40 mg) or at maximally tolerated dose of those statins, with or without other LMT. Patients were randomized 1:1 to receive either alirocumab 75 mg once every two weeks (Q2W) or placebo Q2W. At month 2, if additional LDL-C lowering was required based on pre- specified LDL-C criteria (LDL-C ≥50 mg/dL or 1.29 mmol/L), alirocumab was adjusted to 150 mg Q2W. For patients who had their dose adjusted to 150 mg Q2W and who had two consecutive LDL-C values below 25 mg/dL (0.65 mmol/L), down-titration from 150 mg Q2W to 75 mg Q2W was performed. Patients on 75 mg Q2W who had two consecutive LDL-C values below 15 mg/dL (0.39 mmol/L) were switched to placebo in a blinded fashion. Approximately 2,615 (27.7%) of 9,451 patients treated with alirocumab required dose adjustment to 150 mg Q2W. Of these 2,615 patients, 805 (30.8%) were down-titrated to 75 mg Q2W. Overall, 730 (7.7%) of 9,451 patients switched to placebo. A total of 99.5% of patients were followed for survival until the end of the trial. The median follow-up duration was 33 months. The index ACS event was a myocardial infarction in 83.2% of patients (34.6% STEMI, 48.6% NSTEMI) and an episode of unstable angina in 16.8% of patients. Most patients (88.8%) were receiving high intensity statin therapy with or without other LMT at randomization. The mean LDL-C value at baseline was 92.4 mg/dL (2.39 mmol/L). Alirocumab significantly reduced the risk for the primary composite endpoint of the time to first occurrence of Major Adverse Cardiovascular Events (MACE-plus) consisting of coronary heart disease (CHD) death, non-fatal myocardial infarction (MI), fatal and non-fatal ischemic stroke, or unstable angina (UA) requiring hospitalization (HR 0.85, 95% CI: 0.78, 0.93; p-value=0.0003). Alirocumab also significantly reduced the following composite endpoints: risk of CHD event; major CHD event; cardiovascular event; and the composite of all-cause mortality, non-fatal MI, and non-fatal ischemic stroke. A reduction of all-cause mortality was also observed, with only nominal statistical significance by hierarchical testing (HR 0.85, 95% CI: 0.73, 0.98). The results are presented in Table 3. Table 3: Efficacy of alirocumab in ODYSSEY OUTCOMES (overall population) Endpoint Number of events Alirocumab Placebo Hazard ratio N=9,462 N=9,462 (95% CI) n (%) n (%) p-value Primary endpoint (MACE- 0.85 (0.78, 0.93) 903 (9.5%) 1052 (11.1%) plusa) 0.0003 0.92 (0.76, 1.11) CHD death 205 (2.2%) 222 (2.3%) 0.38 0.86 (0.77, 0.96) Non-fatal MI 626 (6.6%) 722 (7.6%) 0.006f 0.73 (0.57, 0.93) Ischemic stroke 111 (1.2%) 152 (1.6%) 0.01f 0.61 (0.41, 0.92) Unstable anginab 37 (0.4%) 60 (0.6%) 0.02f Secondary endpoints 0.88 (0.81, 0.95) CHD eventc 1199 (12.7%) 1349 (14.3%) 0.0013 0.88 (0.80, 0.96) Major CHD eventd 793 (8.4%) 899 (9.5%) 0.0060 0.87 (0.81, 0.94) Cardiovascular evente 1301 (13.7%) 1474 (15.6%) 0.0003 All-cause mortality, non-fatal 0.86 (0.79, 0.93) 973 (10.3%) 1126 (11.9%) MI, non-fatal ischemic stroke 0.0003 0.92 (0.76, 1.11) CHD death 205 (2.2%) 222 (2.3%) 0.3824 0.88 (0.74, 1.05) CV death 240 (2.5%) 271 (2.9%) 0.1528 0.85 (0.73, 0.98) All-cause mortality 334 (3.5%) 392 (4.1%) 0.0261f Favours Alirocumab Favours Placebo a MACE-plus defined as a composite of: coronary heart disease (CHD) death, non-fatal myocardial infarction (MI), fatal and non-fatal ischemic stroke, or unstable angina (UA) requiring hospitalization b Unstable angina requiring hospitalization c CHD event defined as: major CHD eventd, unstable angina requiring hospitalization, ischemia-driven coronary revascularization procedure d Major CHD event defined as: CHD death, non-fatal MI e Cardiovascular event defined as follows: CV death, any non-fatal CHD event, and non-fatal ischemic stroke f Nominal significance The Kaplan-Meier estimates of the cumulative incidence of the primary endpoint for the overall patient population over time are presented in Figure 1. Figure 1 Primary composite endpoint cumulative incidence over 4 years in ODYSSEY OUTCOMES Overall population Hazard Ratio: 0.85 95% CI (0.78, 0.93) Cu mu lati Placebo ve inci Alirocumab den ce of eve nt Time (months) Neurocognitive function A 96 week, randomized, double-blinded, placebo‑controlled trial evaluated the effect of alirocumab on neurocognitive function after 96 weeks of treatment (~2 years) in patients with heterozygous familial hypercholesterolemia (HeFH) or non-familial hypercholesterolemia at high or very high cardiovascular risk. Neurocognitive function was assessed using the Cambridge Neuropsychological Test Automated Battery (CANTAB). A total of 2171 patients were randomized; 1087 patients were treated with alirocumab 75 mg and/or 150 mg every 2 weeks and 1084 patients were treated with placebo. A majority (>80%) of patients in each group completed the 96-week, double-blind treatment period. Over the 96 weeks of treatment, alirocumab showed no effect on neurocognitive function. The percentage of patients who experienced neurocognitive disorders was low in the alirocumab (1.3%) treatment groups and comparable to placebo (1.7%). No safety concerns related to neurocognitive function were observed in patients treated with alirocumab who experienced either 2 consecutive LDL- C values <25 mg/dL (<0.65 mmol/L) or <15 mg/dL (<0.39 mmol/L) during the treatment period.
Pharmacokinetic Properties
5.2 Pharmacokinetic properties Absorption After subcutaneous administration of 50 mg to 300 mg alirocumab, median times to maximum serum concentration (tmax) were 3-7 days. The pharmacokinetics of alirocumab after single subcutaneous administration of 75 mg into the abdomen, upper arm or thigh were similar. The absolute bioavailability of alirocumab after subcutaneous administration was about 85% as determined by population pharmacokinetic analysis. Monthly exposure with 300 mg every 4 weeks treatment was similar to that of 150 mg every 2 weeks. The fluctuations between Cmax and Ctrough were higher for the every 4 weeks dosage regimen. Steady state was reached after 2 to 3 doses with an accumulation ratio up to a maximum of about 2-fold. Distribution Following intravenous administration, the volume of distribution was about 0.04 to 0.05 L/kg indicating that alirocumab is distributed primarily in the circulatory system. Biotransformation Specific metabolism studies were not conducted, because alirocumab is a protein. Alirocumab is expected to degrade to small peptides and individual amino acids. Elimination Two elimination phases were observed for alirocumab. At low concentrations, the elimination is predominately through saturable binding to target (PCSK9), while at higher concentrations the elimination of alirocumab is largely through a non-saturable proteolytic pathway. Based on a population pharmacokinetic analysis, the median apparent half-life of alirocumab at steady state was 17 to 20 days in patients receiving alirocumab as monotherapy at subcutaneous doses of either 75 mg Q2W or 150 mg Q2W. When co-administered with a statin, the median apparent half-life of alirocumab was 12 days. Linearity/non-linearity A slightly greater than dose proportional increase was observed, with a 2.1- to 2.7-fold increase in total alirocumab concentrations for a 2-fold increase in dose from 75 mg to 150 mg Q2W. Special populations Elderly Based on a population pharmacokinetic analysis, age was associated with a small difference in alirocumab exposure at steady state, with no impact on efficacy or safety. Gender Based on a population pharmacokinetic analysis, gender has no impact on alirocumab pharmacokinetics. Race Based on a population pharmacokinetic analysis, race had no impact on alirocumab pharmacokinetics. Following single-dose subcutaneous administration of 100 mg to 300 mg alirocumab, there was no meaningful difference in exposure between Japanese and Caucasian healthy subjects. Body weight Body weight was identified as one significant covariate in the final population PK model impacting alirocumab pharmacokinetics. Alirocumab exposure (AUC0-14d) at steady state at both the 75 and 150 mg Q2W dosing regimen was decreased by 29% and 36% in patients weighing more than 100 kg as compared to patients weighing between 50 kg and 100 kg. This did not translate into a clinically meaningful difference in LDL-C lowering. Hepatic impairment In a phase 1 study, after administration of a single 75 mg subcutaneous dose, alirocumab pharmacokinetic profiles in subjects with mild and moderate hepatic impairment were similar as compared to subjects with normal hepatic function. No data are available in patients with severe hepatic impairment. Renal impairment Since monoclonal antibodies are not known to be eliminated via renal pathways, renal function is not expected to impact the pharmacokinetics of alirocumab. Population pharmacokinetic analyses showed that alirocumab exposure (AUC0-14d) at steady state at both the 75 and 150 mg Q2W dosing regimen was increased by 22%-35%, and 49%-50% in patients with mild and moderate renal impairment, respectively, compared to patients with normal renal function. The distribution of body weight and age, two covariates impacting alirocumab exposure, were different among renal function categories and most likely explain the observed pharmacokinetic differences. Limited data are available in patients with severe renal impairment; in these patients the exposure to alirocumab was approximately 2-fold higher compared with subjects with normal renal function. Pharmacokinetic/pharmacodynamic relationship(s) The pharmacodynamic effect of alirocumab in lowering LDL-C is indirect, and mediated through the binding to PCSK9. A concentration-dependent reduction in free PCSK9 and LDL-C is observed until target saturation is achieved. Upon saturation of PCSK9 binding, further increases in alirocumab concentrations do not result in a further LDL-C reduction, however an extended duration of the LDL-C lowering effect is observed.

פרטי מסגרת הכללה בסל
א. התרופה תינתן למניעה שניונית של אירועים קרדיווסקולריים בחולים עם מחלה קרדיווסקולרית ידועה שחוו בעבר אוטם שריר הלב או שבץ מוחי איסכמי לא אמבולי וערכי ה-LDL שלהם מעל 100 מ"ג/דצ"ל, למרות טיפול מרבי בסטטינים בשילוב עם Ezetimibe, למשך חודשיים לפחות. ב. תחילת הטיפול בתרופה ייעשה לפי מרשם של רופא מומחה בקרדיולוגיה או רופא מומחה בליפידים או רופא מומחה בנוירולוגיה.
מסגרת הכללה בסל
התוויות הכלולות במסגרת הסל
| התוויה | תאריך הכללה | תחום קליני | Class Effect | מצב מחלה |
|---|---|---|---|---|
| א. התרופה תינתן למניעה שניונית של אירועים קרדיווסקולריים בחולים עם מחלה קרדיווסקולרית ידועה שחוו אוטם שריר הלב או שבץ מוחי איסכמי לא אמבולי בשלוש השנים טרם ההערכה וערכי ה-LDL שלהם מעל 100 מ"ג/דצ"ל, למרות טיפול מרבי בסטטינים בשילוב עם Ezetimibe, למשך חודשיים לפחות. ב. תחילת הטיפול בתרופה ייעשה לפי מרשם של רופא מומחה בקרדיולוגיה או רופא מומחה בליפידים או רופא מומחה בנוירולוגיה. | 30/01/2020 | ליפידים | היפרכולסטרולמיה, דיסליפידמיה | |
| 4. הוראות לשימוש בתרופה ALIROCUMAB (Praluent) א. התרופה תינתן למניעה שניונית של אירועים קרדיווסקולריים בחולים עם מחלה קרדיווסקולרית ידועה שחוו אוטם שריר הלב או שבץ מוחי איסכמי לא אמבולי בשלוש השנים טרם ההערכה וערכי ה-LDL שלהם מעל 130 מ"ג/דצ"ל, למרות טיפול מרבי בסטטינים בשילוב עם Ezetimibe, למשך חודשיים לפחות. ב. תחילת הטיפול בתרופה ייעשה לפי מרשם של רופא מומחה בקרדיולוגיה או רופא מומחה בליפידים. | 11/01/2018 | ליפידים | היפרכולסטרולמיה, דיסליפדמיה | |
| א. התרופה תינתן למניעה שניונית של אירועים קרדיווסקולריים בחולים עם מחלה קרדיווסקולרית ידועה שחוו בעבר אוטם שריר הלב או שבץ מוחי איסכמי לא אמבולי וערכי ה-LDL שלהם מעל 100 מ"ג/דצ"ל, למרות טיפול מרבי בסטטינים בשילוב עם Ezetimibe, למשך חודשיים לפחות. ב. תחילת הטיפול בתרופה ייעשה לפי מרשם של רופא מומחה בקרדיולוגיה או רופא מומחה בליפידים או רופא מומחה בנוירולוגיה. | 01/02/2023 | ליפידים | EVOLOCUMAB, ALIROCUMAB | היפרכולסטרולמיה, דיסליפידמיה |
שימוש לפי פנקס קופ''ח כללית 1994
לא צוין
תאריך הכללה מקורי בסל
11/01/2018
הגבלות
תרופה מוגבלת לרישום ע'י רופא מומחה או הגבלה אחרת
מידע נוסף
עלון מידע לצרכן
27.04.21 - עלון לצרכן אנגלית 25.05.22 - עלון לצרכן אנגלית 23.08.20 - עלון לצרכן עברית 25.05.22 - עלון לצרכן עברית 27.04.21 - עלון לצרכן ערבית 25.05.22 - עלון לצרכן ערבית 25.06.19 - עלון לצרכן 12.10.22 - עלון לצרכן עברית 16.03.23 - עלון לצרכן אנגלית 16.03.23 - עלון לצרכן עברית 05.06.23 - עלון לצרכן עברית 16.03.23 - עלון לצרכן ערבית 26.01.24 - עלון לצרכן עברית 25.03.24 - עלון לצרכן אנגלית 25.03.24 - עלון לצרכן אנגלית 25.03.24 - עלון לצרכן עברית 25.03.24 - עלון לצרכן עברית 25.03.24 - עלון לצרכן ערבית 25.03.24 - עלון לצרכן ערבית 04.04.24 - עלון לצרכן אנגלית 04.04.24 - עלון לצרכן עברית 04.04.24 - עלון לצרכן ערבית 06.12.18 - החמרה לעלון 25.05.20 - החמרה לעלון 23.08.20 - החמרה לעלון 05.10.20 - החמרה לעלון 02.05.22 - החמרה לעלון 14.09.22 - החמרה לעלון 12.10.22 - החמרה לעלון 05.06.23 - החמרה לעלוןלתרופה במאגר משרד הבריאות
פראלואנט 75 מ"ג/מ"ל