Quest for the right Drug
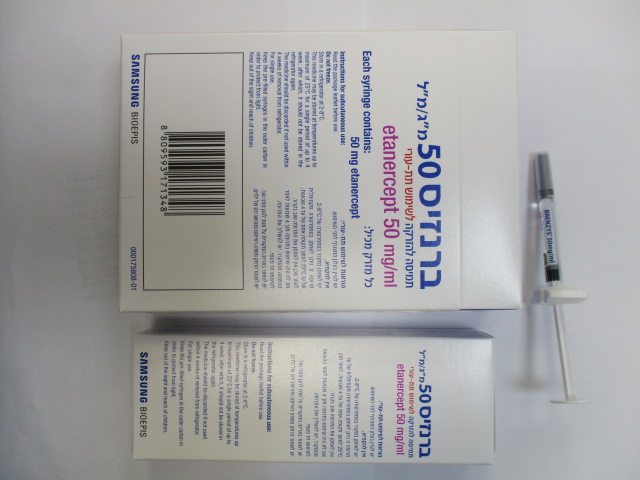
ברנזיס 50 מ"ג/מ"ל BRENZYS 50 MG/ML (ETANERCEPT)
תרופה במרשם
תרופה בסל
נרקוטיקה
ציטוטוקסיקה
צורת מתן:
תת-עורי : S.C
צורת מינון:
תמיסה להזרקה : SOLUTION FOR INJECTION
עלון לרופא
מינוניםPosology התוויות
Indications תופעות לוואי
Adverse reactions התוויות נגד
Contraindications אינטראקציות
Interactions מינון יתר
Overdose הריון/הנקה
Pregnancy & Lactation אוכלוסיות מיוחדות
Special populations תכונות פרמקולוגיות
Pharmacological properties מידע רוקחי
Pharmaceutical particulars אזהרת שימוש
Special Warning עלון לרופא
Physicians Leaflet
Adverse reactions : תופעות לוואי
4.8 Undesirable effects Summary of the safety profile The most commonly reported adverse reactions are injection site reactions (such as pain, swelling, itching, reddening and bleeding at the puncture site), infections (such as upper respiratory infections, bronchitis, bladder infections and skin infections), allergic reactions, development of autoantibodies, itching, and fever. Serious adverse reactions have also been reported for etanercept. TNF-antagonists, such as etanercept, affect the immune system and their use may affect the body’s defenses against infection and cancer. Serious infections affect fewer than 1 in 100 patients treated with etanercept. Reports have included fatal and life-threatening infections and sepsis. Various malignancies have also been reported with use of etanercept, including cancers of the breast, lung, skin and lymph glands (lymphoma). Serious haematological, neurological and autoimmune reactions have also been reported. These include rare reports of pancytopenia and very rare reports of aplastic anaemia. Central and peripheral demyelinating events have been seen rarely and very rarely, respectively, with etanercept use. There have been rare reports of lupus, lupus-related conditions, and vasculitis. Tabulated list of adverse reactions The following list of adverse reactions is based on experience from clinical trials in adults and on postmarketing experience. Within the System Organ Class, adverse reactions are listed under headings of frequency (number of patients expected to experience the reaction), using the following categories: very common (≥1/10); common (≥1/100 to <1/10); uncommon (≥1/1,000 to <1/100); rare (≥1/10,000 to <1/1,000); very rare (<1/10,000); not known (cannot be estimated from the available data). System Organ Very Common Uncommon Rare Very Rare Frequency Not Class Common ≥ 1/100 ≥ 1/1,000 to < 1/100 ≥ 1/10,000 to < 1/10,000 Known ≥ 1/10 to < 1/10 < 1/1,000 (Cannot be Estimated from Available Data) Infections and Infection Serious infections Tuberculosis, Hepatitis B infestations (including (including opportunistic reactivation, upper pneumonia, infection (including listeria respiratory cellulitis, arthritis invasive fungal, tract bacterial, sepsis and protozoal, bacterial, infection, parasitic infection)* atypical bronchitis, mycobacterial, viral cystitis, infections and skin Legionella)* infection)* Neoplasms Non-melanoma skin Malignant melanoma Merkel cell benign, cancers* (see (see section 4.4), carcinoma (see malignant and section 4.4) lymphoma, section 4.4) unspecified leukaemia (including cysts and polyps) Blood and Thrombocytopenia, Pancytopenia* Aplastic Histiocytosis lymphatic anaemia, anaemia* haematophagic system disorders leukopenia, (macrophage neutropenia activation syndrome)* Immune system Allergic Vasculitis Serious Worsening of disorders reactions (see (including anti- allergic/anaphylactic symptoms of Skin and neutrophilic reactions (including dermatomyositis subcutaneous cytoplasmic angioedema, tissue antibody positive bronchospasm), disorders), vasculitis) sarcoidosis autoantibody formation* Nervous system CNS demyelinating disorders cases suggestive of multiple sclerosis or localised demyelinating conditions, such as optic neuritis and transverse myelitis (see section 4.4), peripheral demyelinating System Organ Very Common Uncommon Rare Very Rare Frequency Not Class Common ≥ 1/100 ≥ 1/1,000 to < 1/100 ≥ 1/10,000 to < 1/10,000 Known ≥ 1/10 to < 1/10 < 1/1,000 (Cannot be Estimated from Available Data) events, including Guillain-Barré syndrome, chronic inflammatory demyelinating polyneuropathy, demyelinating polyneuropathy, and multifocal motor neuropathy (see section 4.4), seizure Eye disorders Uveitis, scleritis Cardiac Worsening of New onset cardiac disorders cardiac failure failure congestive congestive (see (see section 4.4) section 4.4) Respiratory, Interstitial lung thoracic, and disease (including mediastinal pneumonitis and disorders pulmonary fibrosis)* Gastrointestinal Inflammatory bowel disorders disease Hepatobiliary Elevated liver Autoimmune disorders enzymes* hepatitis* Skin and Pruritus, rash Angioedema, Stevens-Johnson Toxic subcutaneous psoriasis (including syndrome, cutaneous epidermal tissue disorders new onset or vasculitis (including necrolysis worsening and hypersensitivity pustular, primarily vasculitis), erythema palms and soles), multiforme, urticaria, lichenoid reactions psoriasiform rash Musculoskeletal Cutaneous lupus and connective erythematosus, tissue disorders subacute cutaneous lupus erythematosus,lupus- like syndrome General Injection Pyrexia disorders and site administration reactions site conditions (including bleeding, bruising, erythema, itching, pain, swelling)* *see Description of selected adverse reactions, below. Description of selected adverse reactions Malignancies and lymphoproliferative disorders One hundred and twenty-nine (129) new malignancies of various types were observed in 4,114 rheumatoid arthritis patients treated in clinical trials with etanercept for up to approximately 6 years, including 231 patients treated with etanercept in combination with methotrexate in the 2-year active- controlled study. The observed rates and incidences in these clinical trials were similar to those expected for the population studied. A total of 2 malignancies were reported in clinical studies of approximately 2 years duration involving 240 etanercept-treated psoriatic arthritis patients. In clinical studies conducted for more than 2 years with 351 ankylosing spondylitis patients, 6 malignancies were reported in etanercept-treated patients. In a group of 2,711 plaque psoriasis patients treated with etanercept in double-blind and open-label studies of up to 2.5 years, 30 malignancies and 43 nonmelanoma skin cancers were reported. In a group of 7,416 patients treated with etanercept in rheumatoid arthritis, psoriatic arthritis, ankylosing spondylitis and psoriasis clinical trials, 18 lymphomas were reported. Reports of various malignancies (including breast and lung carcinoma and lymphoma) have also been received in the postmarketing period (see section 4.4). Injection site reactions Compared to placebo, patients with rheumatic diseases treated with etanercept had a significantly higher incidence of injection site reactions (36% vs. 9%). Injection site reactions usually occurred in the first month. Mean duration was approximately 3 to 5 days. No treatment was given for the majority of injection site reactions in the etanercept treatment groups, and the majority of patients who were given treatment received topical preparations, such as corticosteroids, or oral antihistamines. Additionally, some patients developed recall injection site reactions characterised by a skin reaction at the most recent site of injection, along with the simultaneous appearance of injection site reactions at previous injection sites. These reactions were generally transient and did not recur with treatment. In controlled trials in patients with plaque psoriasis, approximately 13.6% of patients treated with etanercept developed injection site reactions compared with 3.4% of placebo-treated patients during the first 12 weeks of treatment. Serious infections In placebo-controlled trials, no increase in the incidence of serious infections (fatal, life-threatening, or requiring hospitalisation or intravenous antibiotics) was observed. Serious infections occurred in 6.3% of rheumatoid arthritis patients treated with etanercept for up to 48 months. These included abscess (at various sites), bacteraemia, bronchitis, bursitis, cellulitis, cholecystitis, diarrhoea, diverticulitis, endocarditis (suspected), gastroenteritis, hepatitis B, herpes zoster, leg ulcer, mouth infection, osteomyelitis, otitis, peritonitis, pneumonia, pyelonephritis, sepsis, septic arthritis, sinusitis, skin infection, skin ulcer, urinary tract infection, vasculitis, and wound infection. In the 2-year active- controlled study where patients were treated with either etanercept alone, methotrexate alone or etanercept in combination with methotrexate, the rates of serious infections were similar among the treatment groups. However, it cannot be excluded that the combination of etanercept with methotrexate could be associated with an increase in the rate of infections. There were no differences in rates of infection among patients treated with etanercept and those treated with placebo for plaque psoriasis in placebo-controlled trials of up to 24 weeks duration. Serious infections experienced by etanercept-treated patients included cellulitis, gastroenteritis, pneumonia, cholecystitis, osteomyelitis, gastritis, appendicitis, Streptococcal fasciitis, myositis, septic shock, diverticulitis and abscess. In the double-blind and open-label psoriatic arthritis trials, 1 patient reported a serious infection (pneumonia). Serious and fatal infections have been reported during use of etanercept; reported pathogens include bacteria, mycobacteria (including tuberculosis), viruses and fungi. Some have occurred within a few weeks after initiating treatment with etanercept in patients who have underlying conditions (e.g., diabetes, congestive heart failure, history of active or chronic infections) in addition to their rheumatoid arthritis (see section 4.4). Brenzys treatment may increase mortality in patients with established sepsis. Opportunistic infections have been reported in association with etanercept, including invasive fungal, parasitic (including protozoal), viral (including herpes zoster), bacterial (including Listeria and Legionella), and atypical mycobacterial infections. In a pooled data set of clinical trials, the overall incidence of opportunistic infections was 0.09% for the 15,402 subjects who received etanercept. The exposure-adjusted rate was 0.06 events per 100 patient-years. In postmarketing experience, approximately half of all of the case reports of opportunistic infections worldwide were invasive fungal infections. The most commonly reported invasive fungal infections included Candida, Pneumocystis, Aspergillus, and Histoplasma. Invasive fungal infections accounted for more than half of the fatalities amongst patients who developed opportunistic infections. The majority of the reports with a fatal outcome were in patients with Pneumocystis pneumonia, unspecified systemic fungal infections, and aspergillosis (see section 4.4). Autoantibodies Adult patients had serum samples tested for autoantibodies at multiple timepoints. Of the rheumatoid arthritis patients evaluated for antinuclear antibodies (ANA), the percentage of patients who developed new positive ANA (≥ 1:40) was higher in patients treated with etanercept (11%) than in placebo- treated patients (5%). The percentage of patients who developed new positive anti-double-stranded DNA antibodies was also higher by radioimmunoassay (15% of patients treated with etanercept compared to 4% of placebo-treated patients) and by Crithidia luciliae assay (3% of patients treated with etanercept compared to none of placebo-treated patients). The proportion of patients treated with etanercept who developed anticardiolipin antibodies was similarly increased compared to placebo- treated patients. The impact of long-term treatment with etanercept on the development of autoimmune diseases is unknown. There have been rare reports of patients, including rheumatoid factor positive patients, who have developed other autoantibodies in conjunction with a lupus-like syndrome or rashes that are compatible with subacute cutaneous lupus or discoid lupus by clinical presentation and biopsy. Pancytopenia and aplastic anaemia There have been postmarketing reports of pancytopenia and aplastic anaemia, some of which had fatal outcomes (see section 4.4). Interstitial lung disease In controlled clinical trials of etanercept across all indications, the frequency (incidence proportion) of interstitial lung disease in patients receiving etanercept without concomitant methotrexate was 0.06% (frequency rare). In the controlled clinical trials that allowed concomitant treatment with etanercept and methotrexate, the frequency (incidence proportion) of interstitial lung disease was 0.47% (frequency uncommon). There have been postmarketing reports of interstitial lung disease (including pneumonitis and pulmonary fibrosis), some of which had fatal outcomes. Concurrent treatment with anakinra In studies when adult patients received concurrent treatment with etanercept plus anakinra, a higher rate of serious infections compared to etanercept alone was observed and 2% of patients (3/139) developed neutropenia (absolute neutrophil count < 1,000/mm3). While neutropenic, one patient developed cellulitis that resolved after hospitalisation (see sections 4.4 and 4.5). Elevated liver enzymes In the double-blind periods of controlled clinical trials of etanercept across all indications, the frequency (incidence proportion) of adverse events of elevated liver enzymes in patients receiving etanercept without concomitant methotrexate was 0.54% (frequency uncommon). In the double-blind periods of controlled clinical trials that allowed concomitant treatment with etanercept and methotrexate, the frequency (incidence proportion) of adverse events of elevated liver enzymes was 4.18% (frequency common). Autoimmune hepatitis In controlled clinical trials of etanercept across all indications, the frequency (incidence proportion) of autoimmune hepatitis in patients receiving etanercept without concomitant methotrexate was 0.02% (frequency rare). In the controlled clinical trials that allowed concomitant treatment with etanercept and methotrexate, the frequency (incidence proportion) of autoimmune hepatitis was 0.24% (frequency uncommon). Paediatric population Undesirable effects in paediatric patients with juvenile idiopathic arthritis In general, the adverse events in paediatric patients with juvenile idiopathic arthritis were similar in frequency and type to those seen in adult patients. Differences from adults and other special considerations are discussed in the following paragraphs. The types of infections seen in clinical trials in juvenile idiopathic arthritis patients aged 2 to 18 years were generally mild to moderate and consistent with those commonly seen in outpatient paediatric populations. Severe adverse events reported included varicella with signs and symptoms of aseptic meningitis, which resolved without sequelae (see also section 4.4), appendicitis, gastroenteritis, depression/personality disorder, cutaneous ulcer, oesophagitis/gastritis, group A streptococcal septic shock, type I diabetes mellitus, and soft tissue and post-operative wound infection. In one study in children with juvenile idiopathic arthritis aged 4 to 17 years, 43 of 69 (62%) children experienced an infection while receiving etanercept during 3 months of the study (part 1, open-label), and the frequency and severity of infections was similar in 58 patients completing 12 months of open- label extension therapy. The types and proportion of adverse events in juvenile idiopathic arthritis patients were similar to those seen in trials of etanercept in adult patients with rheumatoid arthritis, and the majority were mild. Several adverse events were reported more commonly in 69 juvenile idiopathic arthritis patients receiving 3 months of etanercept compared to the 349 adult rheumatoid arthritis patients. These included headache (19% of patients, 1.7 events per patient year), nausea (9%, 1.0 event per patient year), abdominal pain (19%, 0.74 events per patient year), and vomiting (13%, 0.74 events per patient year). There were 4 reports of macrophage activation syndrome in juvenile idiopathic arthritis clinical trials. There have been reports of inflammatory bowel disease and uveitis in JIA patients being treated with etanercept from post-marketing sources, including a very small number of cases indicating a positive rechallenge (see section 4.4). Undesirable effects in paediatric patients with plaque psoriasis In a 48-week study in 211 children aged 4 to 17 years with paediatric plaque psoriasis, the adverse events reported were similar to those seen in previous studies in adults with plaque psoriasis. Reporting of suspected adverse reactions Reporting suspected adverse reactions after authorisation of the medicinal product is important. It allows continued monitoring of the benefit/risk balance of the medicinal product. Any suspected adverse events should be reported to the Ministry of Health according to the National Regulation by using an online form https://sideeffects.health.gov.il

פרטי מסגרת הכללה בסל
1. התרופה תינתן לטיפול בחולה הסובל מאחד מאלה: א. ארתריטיס ראומטואידית - כאשר התגובה לתכשירים ממשפחת ה-DMARDs איננה מספקת, בכפוף לתנאי פסקה 3; ב. ארתריטיס כרוני בצעירים (Juvenile chronic arthritis) - בקטינים שמלאו להם 4 שנים וטרם מלאו להם 17 שנים הסובלים ממהלך מחלה רב מפרקי פעיל ושלא הגיבו לטיפול ב-methotrexate או שאינם מסוגלים לקבל טיפול כאמור; ג. דלקת מפרקים פסוריאטית קשה כאשר התגובה לתכשירים ממשפחת ה-DMARDs איננה מספקת ולאחר כשלון או אי סבילות ל-salazopyrin או methotrexate; ד. אנקילוזינג ספונדילטיס קשה אם החולה לא הגיב לטיפול קונבנציונלי; במקרה של הוריאנט דמוי אנקילוזינג ספונדיליטיס הקשור בפסוריאזיס, תהיה ההוריה כמו באנקילוזינג ספונדיליטיס ראשונית; ה. פסוריאזיס מלווה בוריאנט דמוי אנקילוזינג ספונדיליטיס, אם החולה לא הגיב לטיפול קונבנציונלי; ו. פסוריאזיס - בהתקיים כל אלה: 1. החולה סובל מאחד מאלה: א. מחלה מפושטת מעל ל-50% של שטח גוף או PASI מעל 50. ב. נגעים באזורי גוף רגישים - אזורים אלו יכללו פנים, צוואר, קיפולי עור, כפות ידיים, כפות רגליים, אזור הגניטליה והישבן;2. החולה קיבל שני טיפולים סיסטמיים לפחות בלא שיפור של 50% לפחות ב-PASI לאחר סיום הטיפול בהשוואה לתחילת הטיפול; בהתייחס לחולה העונה על האמור בפסקת משנה (1)(ב) - החולה קיבל שני טיפולים סיסטמיים לפחות בלא שיפור משמעותי לאחר סיום הטיפול בהשוואה לתחילת הטיפול; 3. התרופה תינתן על פי מרשם של רופא מומחה בדרמטולוגיה. 3. הטיפול בתרופה לחולה העונה על תנאי פסקה (1) (א), יינתן בהתקיים כל אלה: 1. קיימת עדות לדלקת פרקים (RA-Rheumatoid Arthritis) פעילה המתבטאת בשלושה מתוך אלה: א. מחלה דלקתית (כולל כאב ונפיחות) בארבעה פרקים ויותר; ב. שקיעת דם או CRP החורגים מהנורמה באופן משמעותי (בהתאם לגיל החולה); ג. שינויים אופייניים ל-RA בצילומי רנטגן של הפרקים הנגועים; ד. פגיעה תפקודית המוגדרת כהגבלה משמעותית בתפקודו היומיומי של החולה ובפעילותו בעבודה. 2. לאחר מיצוי הטיפול בתרופות השייכות למשפחת ה-NSAIDs ובתרופות השייכות למשפחת ה-DMARDs. לעניין זה יוגדר מיצוי הטיפול כהעדר תגובה קלינית לאחר טיפול קו ראשון בתרופות אנטי דלקתיות ממשפחת ה-NSAIDs וטיפול קו שני ב-3 תרופות לפחות ממשפחת ה-DMARDs שאחת מהן מתוטרקסאט, במשך 3 חודשים רצופים לפחות. 3. הטיפול יינתן באישור רופא מומחה בראומטולוגיה.
מסגרת הכללה בסל
התוויות הכלולות במסגרת הסל
| התוויה | תאריך הכללה | תחום קליני | Class Effect | מצב מחלה |
|---|---|---|---|---|
| juvenile idiopathic rheumatoid arthritis | ADALIMUMAB, ETANERCEPT | |||
| Psoriatic arthritis | ADALIMUMAB, ETANERCEPT, INFLIXIMAB, USTEKINUMAB, SECUKINUMAB | |||
| Psoriasis | ADALIMUMAB, ALEFACEPT, ETANERCEPT, INFLIXIMAB, EFALIZUMAB, USTEKINUMAB, SECUKINUMAB, IXEKIZUMAB | |||
| Rheumatoid arthritis | ETANERCEPT, INFLIXIMAB, ABATACEPT, TOCILIZUMAB, TOFACITINIB, CERTOLIZUMAB PEGOL, SARILUMAB | |||
| Ankylosing spondylitis | ADALIMUMAB, ETANERCEPT, INFLIXIMAB, USTEKINUMAB, SECUKINUMAB, CERTOLIZUMAB PEGOL |
שימוש לפי פנקס קופ''ח כללית 1994
לא צוין
תאריך הכללה מקורי בסל
01/03/2002
הגבלות
תרופה מוגבלת לרישום ע'י רופא מומחה או הגבלה אחרת
מידע נוסף
